
The evolution of minimally invasive inguinal hernia repairs
Introduction
One of the earliest records of interventions on inguinal hernias dates back to 1550 BC, in which the Eber papyrus describes physicians reducing the hernia and applying heat to the hernia sac. The first surgical inguinal hernia repair was reported by Demetrius Cantemir in 1716, via an open transabdominal approach (1). Although laparoscopic surgery was first introduced by George Kelling in 1901, surgical repair of inguinal hernias remained in an open fashion for the majority of the 1900s. Ger and colleagues described the first laparoscopic inguinal hernia repair conducted in dogs in 1982, in which the abdominal opening of the patent vaginalis processus was closed by a novel stapling device (2). Bogojavalensky later developed the laparoscopic plug and patch repair, inserting a synthetic mesh plug into the hernia defect opening over the peritoneum (3). This technique fell out of favor due to increased risk of small bowel obstructions secondary to adhesions as well as high recurrence rates (4). In 1991, Fitzgibbons et al. described the intraperitoneal onlap mesh (IPOM) repair in pigs using a polypropylene mesh, in which an adhesion barrier was affixed over the peritoneum covering the hernia defect (5). Later that year, Toy and Smoot described a similar laparoscopic IPOM technique in ten patients with high ligation of hernia sac, resulting in a tension-free repair and mesh placement over the peritoneum without groin dissection (6). The IPOM technique was also later abandoned due to the risk of mesh erosion into the bowel. Schultz et al. were was the first to describe a laparoscopic approach in which the peritoneum was dissected to identify the defect and polypropylene mesh was used to obliterate the defect (7).
Anatomy
Proper understanding of abdominal wall and inguinofemoral anatomy is paramount to surgical repair of inguinal hernias. Bordered by the muscles of the abdominal wall, the inguinal canal is the space through which the gonadal structures (spermatic cord and vas deferens in males, round ligament in females) exit the peritoneal cavity. The anterior wall of the inguinal canal is formed by the aponeurosis of the external oblique, while the posterior wall is formed by the transversalis fascia. The roof of the inguinal canal comprises the transversalis fascia, internal oblique, and transversus abdominis muscles; and the floor is formed by the inguinal ligament. The deep opening into the canal is the internal (deep) ring and the superficial opening out of the canal (into the scrotum in males) is the external (superficial) ring.
Inguinal hernias are defined by their relationship to the inguinal canal, as well as within Hasselbach’s triangle (Figure 1) (8). Bordered by the rectus sheath medially, the inferior epigastric vessels laterally, and the inguinal ligament inferiorly, Hasselbach’s triangle distinguishes direct from indirect inguinal hernias. Direct inguinal hernias are caused by weakness in the transversalis fascia, which forms the posterior wall of the inguinal canal. As true hernias, direct hernias pass through the abdominal wall medial to the inferior epigastric vessels, into the inguinal canal and out through the external inguinal ring. In contrast, indirect hernias are caused by a patent processus vaginalis, an embryonic remnant of the peritoneal tunnel leading to the inguinal canal. In male fetal development, the testes migrate through the process vaginalis, led by the gubernaculum, into the scrotum. Persistence of the processus vaginalis allows abdominal contents to pass through the internal ring, through the inguinal canal, and out through the external ring. Thus, direct hernias travel deep to superficial, passing medially to the internal ring, while indirect hernias travel lateral to medial within the inguinal canal before exiting in the external ring. Though femoral hernias are not true inguinal hernias, they are often described and managed along the same vein. Femoral hernias occur below the inguinal ligament and are caused by herniation of the peritoneal contents through the empty space medial to the femoral vein within the femoral triangle, which is defined by the inguinal ligament superiorly, the adductor longus medially, and the sartorius muscle laterally (Figure 1). The European Hernia Society classifies groin hernias based on three criteria: the size of the hernia orifice, anatomic location and whether it is a primary or recurrent hernia (9). Classic open approaches to inguinofemoral hernia repairs focus on identifying and repairing defects in these individual spaces, usually with reinforcing mesh to prevent recurrence.
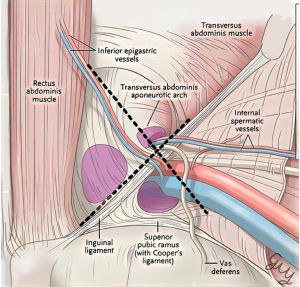
While open repairs target inguinal ring and femoral space defects individually, laparoscopic repairs allow for a single operative fix of direct inguinal hernias, indirect inguinal hernias, and femoral hernias through reinforcement of the myopectineal orifice (Figure 1). First described by Fruchaud in 1956, the myopectineal orifice encompasses the space through which both inguinal and femoral hernias can occur (8,10). Placement of a large piece of mesh encompassing the entirety of the myopectineal orifice allows repair of all three hernia types and forms the foundation of laparoscopic, and later, robotic, inguinal hernia repair.
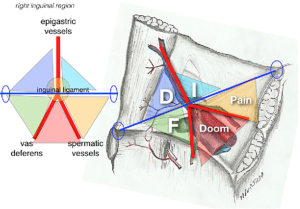
Additional anatomic considerations must be considered when repairing inguinal hernias via a minimally invasive approach. Laparoscopic visualization of groin anatomy allows clear identification of type of hernia defect (Figure 2) (11). In the classic “five triangles” view, the rectus sheath is oriented medially with the iliopubic tract traveling from the pubic symphysis at midline out laterally and superiorly towards the anterior superior iliac spine (ASIS). The inferior epigastric vessels travel perpendicularly to the pubic tract, separating at the pubic tract into the vas deferens (which travels inferiorly) and the spermatic vessels (which travel laterally). Counterclockwise from Hasselbach’s triangle [1], which defines the space through which direct hernias occur, are: [2] the triangular space containing the internal inguinal ring (through which indirect hernias occur), [3] the “triangle of pain” (in which the lateral cutaneous nerve, the femoral branch of the genitofemoral nerve, and the femoral nerve pass), [4] the “triangle of doom” (which contains the external iliac artery and vein), and [5] the triangular space through which femoral hernias occur. When placing mesh in an endoscopic hernia repair, care must be taken to avoid fixation of mesh in the triangles of doom and pain to prevent vascular or nerve injury, while covering all potential spaces in the myopectineal orifice.
Finally, dissection of the potential space in the preperitoneal plane allows proper mesh placement outside the peritoneal cavity, a cornerstone of modern laparoscopic techniques such as transabdominal preperitoneal (TAPP) repair and totally extraperitoneal (TEP) repair. While the two repairs use different approaches, both utilize the same potential preperitoneal space above the peritoneum and below the transversalis fascia, known as the Space of Bogros. In TAPP, surgeons enter the peritoneal cavity and access the preperitoneal plane through a transverse peritoneal incision, later closing the peritoneal flap with sutures or tacks. In contrast, TEP accesses the preperitoneal space through an infraumbilical incision, avoiding entering the peritoneal cavity entirely.
Evolution of TAPP and TEP repairs
Laparo-endoscopic meshed-based repairs are recommended for unilateral and bilateral groin hernias due to lower incidence of postoperative and chronic pain based on multiple international guidelines (12,13). The two most common laparoscopic inguinal hernia repairs used today began in 1992 when Arregui et al. described a laparoscopic preperitoneal approach that employed the same principles of open repairs by replacing and reinforcing the attenuated transversalis fascia. This became known as the TAPP repair. After entering the preperitoneal space by excising the hernia sac, the defect is closed with sutures. Then mesh is placed over the internal ring, testicular vessels, and spermatic cord laterally, Hesselbach’s triangle medially and Cooper’s ligament inferiorly. The mesh is then secured to transversalis fascia superiorly, iliolumbar tract inferiorly and transversus abdominis lateral to internal inguinal ring. The peritoneum is then reapproximated. Arregui et al. found that laparoscopic repairs reduced postoperative pain and recovery time (14). In 1991, Dulucq described the first series of TEP laparoscopic repairs in which the preperitoneal space is dissected using a laparoscope or balloon dissector. This method eliminates both early and late complications related to violation of the peritoneal cavity (15). Sharma et al. conducted the first prospective randomized trial comparing laparoscopic TAPP and TEP approaches for bilateral inguinal hernias with 60 patients included in the study and results analyzed on postoperative days 8 and 30. They found both techniques to be equivalent in terms of postoperative mortality, morbidity, wound infection and early recurrence. However, TEP repairs were found to have increased operating time and more subcutaneous emphysema (16). A meta-analysis of 15 randomized clinical trials that included 1,359 patients subsequently found no significant differences between TEP and TAPP repairs in terms of early postoperative pain, operative time, wound-related complications, hospital length of stay, return to work/daily activities, and costs (17). Similar results were seen in a meta-analysis conducted by Feng et al. in which ten randomized controlled trials with a total of 1,047 patients were analyzed (18). Current international guidelines do not make specific recommendations between laparoscopic TAPP vs. TEP repairs and instead emphasize that the choice should be based on surgeon expertise and preference (12,13). Ielpo et al. found in a prospective randomized controlled trial comparing open Lichtenstein (OL) vs. TAPP that TAPP repairs were associated with less short term and chronic pain, postoperative complications and shorter length of stay (19). Aiolfi et al. conducted a meta-analysis of 35 randomized controlled trials in 2021 comparing Lichtenstein repair with laparoscopic TAPP and TEP repairs. They found that laparoscopic TAPP and TEP repairs were associated with significantly reduced early postoperative pain, return to work/activities, chronic pain, hematoma and wound infection while hernia recurrence, seroma and hospital length of stay similar across all three treatments (20). Additionally, laparoscopic repairs allow surgeons to detect and repair bilateral hernias concurrently (21). Finally, laparoscopic approaches also offer the advantage of closing three potential spaces through which intraabdominal contents can herniate through. prophylactically treating indirect hernias, direct hernias, and femoral hernias with one repair (Table 1) (10,17,19-32).
Table 1
| Author | Year | Type of study | Results |
|---|---|---|---|
| Ali et al. | 2023 | RCT | Mesh non-fixation in TAPP repairs had similar recurrence and postoperative complications compared to fixation with shorter operative time and lower postoperative pain |
| Hidalgo et al. | 2023 | Retrospective cohort | TAPP and TEP had similar outcomes in bilateral inguinal hernia repair |
| Sartori et al. | 2023 | Meta-analysis | Laparoscopic approach seems to be safe approach for acute incarcerated groin hernias |
| Sekhon Inderjit Singh et al. | 2022 | Meta-analysis—22 RCTs | Chronic groin pain rates lower in laparoscopic repairs compared to open repairs at >5 years (4.69% vs. 6.91%). Lower risk of chronic groin pain in TEP repair, not seen in TAPP |
| Aiolfi et al. | 2021 | Meta-Analysis—35 RCTs | Laparoscopic TAPP and TEP repair associated with significantly reduced early postoperative pain, return to work/activities, chronic pain, hematoma, and wound infection compared to the Lichtenstein tension-free repair. Hernia recurrence, seroma, and hospital length of stay seem similar across treatments |
| Aiolfi et al. | 2021 | Meta-analysis—15 RCTs | TAPP vs. TEP similar in recurrence and chronic pain |
| Kler et al. | 2021 | Meta-analysis—2 RCTs and 26 observational studies | No observed difference between TAPP and TEP repairs in terms of return to activity, complications, and postoperative pain in 3-month period |
| Hung et al. | 2020 | Meta-analysis—14 RCTs | TAPP had lower seroma rate and TEP has lower scrotal/cord edema |
| Lydeking et al. | 2020 | Multi-center single blinded RCTs | TAPP and open Lichtenstein repairs had similar recurrence rate after at 12 years. TAPP repair had lower rates of chronic pain, although not statistically significant (4% vs. 7%) |
| Aiolfi et al. | 2019 | Meta-analysis—16 RCTs | No difference found in comparing open, TAPP, TEP, rTAPP in terms of short-term seroma, postoperative chronic pain, recurrence, urinary retention, SSI and LOS |
| Bullen et al. | 2019 | Meta-analysis—12 RCTs | Laparoscopic repair associated with reduced rate of acute and chronic pain with similar recurrence rate between open vs. laparoscopic |
| Ielpo et al. | 2018 | Clinical and cost-effectiveness analysis within RCTs | TAPP repair had less early postoperative pain, shorter LOS and fewer postoperative complications when compared to open Lichtenstein repair. TAPP more cost effective than open repairs |
| Ielpo et al. | 2018 | Prospective RCT | TAPP compared to OL had less postoperative pain, shorter LOS, less postoperative complication, and less chronic pain |
| Yang et al. | 2018 | RCT | TAPP repairs had lower long-tern postoperative complications, faster recovery and lower rates of chronic pain compared to OL in recurrent hernia |
| Scheuermann et al. | 2017 | Meta-analysis—8 RCTs | Reduced rate of chronic inguinal pain in TAPP compared to OL |
| Kargar et al. | 2015 | Prospective RCT | TAPP compared to OL had lower incidence of hematoma, seroma, and infection |
Method: search term on PubMed includes “laparoscopic inguinal hernia repair”. Only RCT, meta-analysis and systemic review articles were reviewed from 2015–2023. RCT, randomized controlled trial; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal; rTAPP, robotic transabdominal preperitoneal; SSI, surgical site infection; LOS, length of stay; OL, open Lichtenstein.
Currently, laparoscopic mesh-based hernia repairs are recommended by multiple international guidelines for repair of inguinal hernias, although each guideline has slight variances. In general, all guidelines recommend laparoscopic approach for bilateral hernias. The Royal College of Surgeons (RCS) recommends a laparoscopic approach in bilateral hernias and in women due to the risk of undiagnosed femoral hernias (33). The European Hernia Society recommends a laparoscopic approach in patients who are employed due to reduced time off work (9). The international HerniaSurge guidelines recommend a laparoscopic approach generally for all men with unilateral hernias (12) However, the rate of laparoscopic inguinal hernia repairs around the world is variable. In an analysis of the incidence and subsequent repair of inguinal hernias in US Armed Forces members from 2010–2019, 45.5% were performed laparoscopically vs. 54.5% in an open fashion. The overall proportion of laparoscopic repairs increased from 11.5% in 2010 to 28.4% in 2019 while open repairs peaked in 2013 (32.5%) and decreased to 21.6% in 2019 (34). In a study conducted in England, Palser et al. found that 65.5% of bilateral hernias, 17.1% of unilateral hernias, and 31.3% of recurrent hernias were performed laparoscopically in men. The authors hypothesized that the variation in rates of laparoscopic approaches is due to the shorter learning curve of open repairs, as well as reduced index operation costs (35). In Spain, the rate of laparoscopic repairs is much lower for bilateral inguinal hernia repairs, with rates of 12% to 29%. The biggest factor contributing to the type of repair performed was the region that the patient was operated in and whether the hospital/surgeon utilized laparoscopy (36).
Evolution of robotic inguinal hernia repairs
Robotic inguinal hernia repairs represent a natural progression of minimally invasive inguinal hernia surgery. The first robotic transabdominal inguinal hernia repairs were performed during concurrent radical prostatectomies (37). However, this approach was quickly adapted by general surgeons due to the advantages of robotic surgery including 10× magnification, three-dimensional views, enhanced endo-wrist dexterity and shorter learning curve (38). The first robotic series of inguinal hernia repairs was published in 2015 in which Engan et al. described a single site TAPP repair (39). Like laparoscopy, both robotic extended TEP (eTEP) and TAPP are technically feasible; however, robotic TAPPs are performed with higher frequency given relative ease of intracorporeal suturing with the robotic console. Robotic inguinal hernia repairs have been found to be comparable to laparoscopic repairs. A recent meta-analysis by Solaini et al. found that robotic repairs have similar perioperative complications and safety profiles compared to laparoscopic repairs; however, the robotic approach was found to take more time in unilateral repairs (40). Similar results were found in the RIVAL trial, which is the first prospective randomized controlled trial that compared laparoscopic and robotic TAPP repairs (41). However multiple studies have shown that after the initial learning curve, operative times significantly decrease (42,43). Tatarian et al. found that robotic TAPP had significantly lower risk of complications and shorter length of stay compared to laparoscopic TAPP and open repairs in a propensity score analysis of 153,727 patients that underwent inguinal hernia repairs in New York State (44). Over the past several years, robotic repairs have risen dramatically with over one-third of inguinal hernia repairs performed on the platform due to the short learning curve compared to laparoscopic repairs, more defined visualization, and improved ergonomics. Proietti et al. found in a cumulative summation test that it takes 43 robotic TAPPs to achieve 90% proficiency and significant reduction in operative time from 71 to 60 minutes (45). While it takes about 100 to 240 operations to develop proficiency for laparoscopic repairs (46-48). Moreover, more complex cases including recurrent hernias are performed robotically due to its stability and increased dexterity. Kudsi et al. found that although a higher number of complex inguinal hernia defined in the study as (I) cases of recurrence after previous laparoscopic repair; (II) cases of previous prostatectomy; (III) cases of inguinal hernias that did not retract after induction of anesthesia and (IV) cases of scrotal inguinal hernias were performed robotically, the mean operative time, intraoperative and postoperative complications were similar to laparoscopic repairs (49). Kolachalam et al. found that in a propensity matched population of obese patients, robotic repairs had lower rates of postoperative complications (3.2% vs. 10.8%) and shorter length of stay (1.9 vs. 4.4 days) compared to open repairs. The study also found that of the seven surgeons enrolled in the trial, three had no previous experience in laparoscopic hernia repairs prior to adoption of the robotic-assisted approach (50). Therefore, robotic-assisted repairs may be a promising approach for patients with complex hernias such as those with recurrent hernias or post-prostatectomy as well as obese patients. Robotic inguinal hernia repairs have been shown to be as safe and effective as laparoscopic repairs and with further implementation of robotic programs across the country, an invaluable tool for complex cases (Table 2) (21,38,40-43,51-57).
Table 2
| Author | Year | Type of study | Results |
|---|---|---|---|
| Ayuso et al. | 2023 | Prospective case study | No difference in recurrence rate, wound infection and readmissions between laparoscopic and robotic inguinal hernia repairs. Operative times were longer for robotic repairs, however 50-minute decrease between beginning and end of study |
| Miller et al. | 2023 | RCT | Laparoscopic and robotic inguinal hernia repairs have similar long-term outcomes (hernia recurrence, neuropathic pain, health-related quality of life and physical activity) |
| Ephraim et al. | 2022 | Retrospective study | Significant decrease in operative times in robotic repairs after initial learning curve |
| Gundogdu et al. | 2020 | Retrospective | Robotic repairs had lower complication rate and less postoperative pain compared with laparoscopic repairs but with longer operative times |
| Hsu et al. | 2023 | Retrospective study | Robotic, laparoscopic, and open repairs had no difference in postoperative complications. Resident involvement associated with shorter operative times |
| Solaini et al. | 2022 | Meta-analysis | Robotic group with longer operative time in unilateral repair. Laparoscopic and robotic repair with similar operative times in bilateral repairs. Similar safety profiles. Robotic repairs had higher costs |
| Bou-Ayash et al. | 2021 | Case series | Robotic approach is feasible option for incarcerated inguinal hernias with shorter LOS and low complication rates |
| Kakiashvili et al. | 2021 | Retrospective study | Robotic and laparoscopic groups had similar operatives. Robotic repairs were associated with decreased postoperative pain compared to open and laparoscopic repairs |
| Qabbani et al. | 2021 | Meta-analysis | No difference in postoperative pain, hernia recurrence or readmission rate between open, laparoscopic and robotic repair. Robotic repair had longer operative time and less complications compared to laparoscopic |
| Zhao et al. | 2021 | Meta-analysis | Laparoscopic and robotic repairs have similar safety profiles and clinical efficacy in Caucasian patients |
| Awad et al. | 2020 | Retrospective study | After initial 20 cases, mean operative time, operative cost and postoperative complications were decreased |
| Prabhu et al. | 2020 | RCT | No difference in post operative complications such as wound events, readmissions, and pain between laparoscopic vs. robotic repairs. Robotic repairs associated with longer operative time and higher median cost |
| Aiolfi et al. | 2019 | Meta-analysis | No difference in postoperative hematoma, SSI, urinary retention and hospital LOS between OL, laparoscopic TAPP, TEP and robotic TAPP |
Method: search terms on PubMed include “robotic inguinal hernia repair”, and articles were reviewed from 2015 to 2023. RCT, randomized controlled trial; LOS, length of stay; SSI, surgical site infection; OL, open Lichtenstein; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal.
Financial implications of minimally invasive inguinal hernia repairs
The cost of minimally invasive inguinal hernia repairs is often cited as a limitation to the its implementation, especially in robotic repairs. For unilateral hernias, operating room (OR) and total hospital costs for laparoscopic repairs are found to be on average significantly higher than open repairs ($3,207 vs. $3,723). However, costs were found to be similar in elective bilateral repairs (58). Ielpo et al. also found that index cost of laparoscopic TAPP repairs is higher compared to OL repairs, but, the mean quality adjusted life years 1 year postoperatively were higher for TAPPs compared to OL, translating to higher cost-effectiveness after TAPPs (29). Perez et al. found that patients undergoing laparoscopic repairs had a decreased length of stay, which resulted in more than $2,000 in healthcare savings compared to open repairs (59). Lam et al. found that laparoscopic repairs were more cost-effective than open repairs in cases that required overnight stays; however, same day open repairs were even more effective at 18.43% savings (60). Robotic-assisted repairs have a higher median cost compared to laparoscopic repairs ($3,258 vs. $1,421) (41). However, Awad et al. found that increasing surgeon experience, defined as after 20 cases, was associated with lower mean direct operative cost by $538.17 as well as shorter operative times (51). Therefore, it can be extrapolated that with further implementation of robotic programs across the country, the mean cost and operative times will continue to decrease. Other strategies can be employed to reduce the cost of robotic repairs. One study found that reducing robotic instruments cost by 30% or increasing the use of individual instruments to 15 times (compared to the current use of 10 times) would allow robotic repairs to match the current reimbursement rates (61). Both are possibilities in the future given advances in technology, increasing marketplace competition among robotic platforms and introduction of robotic platforms such as the Cambridge Medical Robotics whose mission is to offer a more affordable alternative to the current Da Vinci system (62).
Conclusions
Although minimally invasive inguinal hernia repairs have been found to be superior to open repairs in terms of postoperative complications and length of stay, its adoption has not been as universe as other laparoscopic approaches such as cholecystectomies. Most surgeons in the United States continues to prefer open approaches, even for bilateral and recurrent inguinal hernias. The reasons for this preference may be due to the longer learning curve associated with laparoscopic TAPP and TEP repairs as well as the increased economic costs. Robotic-assisted repairs may provide the solution to increasing the rate of minimally invasive inguinal hernia repairs given its shorter learning curve, improved visualization, and enhanced ergonomics especially in the repair of complex and recurrent inguinal hernias.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-57/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-57/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hori T, Yasukawa D. Fascinating history of groin hernias: Comprehensive recognition of anatomy, classic considerations for herniorrhaphy, and current controversies in hernioplasty. World J Methodol 2021;11:160-86. [Crossref] [PubMed]
- Ger R. The management of certain abdominal herniae by intra-abdominal closure of the neck of the sac. Preliminary communication. Ann R Coll Surg Engl 1982;64:342-4. [PubMed]
- Bogojavlensky S. editor. Laparoscopic treatment of inguinal and femoral hernias. Proceedings of the 18th Annual meeting of the American Association of Gynecological Laparoscopists. Washington, DC: 1989.
- Tetik C, Arregui ME, Dulucq JL, et al. Complications and recurrences associated with laparoscopic repair of groin hernias. A multi-institutional retrospective analysis. Surg Endosc 1994;8:1316-22; discussion 1322-3. [Crossref] [PubMed]
- Fitzgibbons RJ Jr, Salerno GM, Filipi CJ, et al. A laparoscopic intraperitoneal onlay mesh technique for the repair of an indirect inguinal hernia. Ann Surg 1994;219:144-56. [Crossref] [PubMed]
- Toy FK, Smoot RT Jr. Toy-Smooth laparoscopic hernioplasty. Surg Laparosc Endosc 1991;1:151-5. [PubMed]
- Schultz L, Graber J, Pietrafitta J, et al. Laser laparoscopic herniorraphy: a clinical trial preliminary results. J Laparoendosc Surg 1990;1:41-5. [Crossref] [PubMed]
- Tansawet A, Rodsakan T, Kasetsermwiriya W, et al. The Myopectineal Orifice: A Study of Thai Cadavers. Front Surg 2022;9:843344. [Crossref] [PubMed]
- Miserez M, Alexandre JH, Campanelli G, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia 2007;11:113-6. Erratum in: Hernia 2008;12:335. [Crossref] [PubMed]
- Yang B, Zhou S, Li Y, et al. A Comparison of Outcomes between Lichtenstein and Laparoscopic Transabdominal Preperitoneal Hernioplasty for Recurrent Inguinal Hernia. Am Surg 2018;84:1774-80. [Crossref] [PubMed]
- Furtado M, Claus CMP, Cavazzola LT, et al. Systemization of laparoscopic inguinal hernia repair (TAPP) based on a new anatomical concept: inverted Y and five triangles. Arq Bras Cir Dig 2019;32:e1426. [Crossref] [PubMed]
- International guidelines for groin hernia management. Hernia 2018;22:1-165. [Crossref] [PubMed]
- van Veenendaal N, Simons M, Hope W, et al. Consensus on international guidelines for management of groin hernias. Surg Endosc 2020;34:2359-77. [Crossref] [PubMed]
- Arregui ME, Davis CJ, Yucel O, et al. Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc 1992;2:53-8. [PubMed]
- Dulucq JL. Treatment of Inguinal Hernias by setting up a sub peritoneal prosthetic patch in retroperitoneoscopy. Cahiers de Chir. 1991;79:15-6.
- Sharma D, Yadav K, Hazrah P, et al. Prospective randomized trial comparing laparoscopic transabdominal preperitoneal (TAPP) and laparoscopic totally extra peritoneal (TEP) approach for bilateral inguinal hernias. Int J Surg 2015;22:110-7. [Crossref] [PubMed]
- Aiolfi A, Cavalli M, Del Ferraro S, et al. Total extraperitoneal (TEP) versus laparoscopic transabdominal preperitoneal (TAPP) hernioplasty: systematic review and trial sequential analysis of randomized controlled trials. Hernia 2021;25:1147-57. [Crossref] [PubMed]
- Wei FX, Zhang YC, Han W, et al. Transabdominal Preperitoneal (TAPP) Versus Totally Extraperitoneal (TEP) for Laparoscopic Hernia Repair: A Meta-Analysis. Surg Laparosc Endosc Percutan Tech 2015;25:375-83. [Crossref] [PubMed]
- Ielpo B, Duran H, Diaz E, et al. A prospective randomized study comparing laparoscopic transabdominal preperitoneal (TAPP) versus Lichtenstein repair for bilateral inguinal hernias. Am J Surg 2018;216:78-83. [Crossref] [PubMed]
- Aiolfi A, Cavalli M, Ferraro SD, et al. Treatment of Inguinal Hernia: Systematic Review and Updated Network Meta-analysis of Randomized Controlled Trials. Ann Surg 2021;274:954-61. [Crossref] [PubMed]
- Aiolfi A, Cavalli M, Micheletto G, et al. Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 2019;23:473-84. [Crossref] [PubMed]
- Scheuermann U, Niebisch S, Lyros O, et al. Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair - A systematic review and meta-analysis of randomized controlled trials. BMC Surg 2017;17:55. [Crossref] [PubMed]
- Kler A, Sekhon N, Antoniou GA, et al. Totally extra-peritoneal repair versus trans-abdominal pre-peritoneal repair for the laparoscopic surgical management of sportsman's hernia: A systematic review and meta-analysis. Surg Endosc 2021;35:5399-413. [Crossref] [PubMed]
- Hung TY, Wu CC, Chen LS, et al. Safety of two common laparoscopic inguinal herniorrhaphy approaches: an updated systematic review with meta-analysis of randomized clinical trials. Transl Androl Urol 2020;9:2007-21. [Crossref] [PubMed]
- Lydeking L, Johansen N, Oehlenschläger J, et al. Re-recurrence and pain 12 years after laparoscopic transabdominal preperitoneal (TAPP) or Lichtenstein's repair for a recurrent inguinal hernia: a multi-centre single-blinded randomised clinical trial. Hernia 2020;24:787-92. [Crossref] [PubMed]
- Ali RF, Elhussainy RM, Aouf AM, et al. Outcomes Of Mesh Fixation Versus Non Fixation In Laparoscopic Transabdominal Preperitoneal Inguinal Hernia Repair: A Randomized Clinical Study. J Pak Med Assoc 2023;73:S8-S12. [Crossref] [PubMed]
- Bullen NL, Massey LH, Antoniou SA, et al. Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 2019;23:461-72. [Crossref] [PubMed]
- Sartori A, Balla A, Botteri E, et al. Laparoscopic approach in emergency for the treatment of acute incarcerated groin hernia: a systematic review and meta-analysis. Hernia 2023;27:485-501. [Crossref] [PubMed]
- Ielpo B, Nuñez-Alfonsel J, Duran H, et al. Cost-effectiveness of Randomized Study of Laparoscopic Versus Open Bilateral Inguinal Hernia Repair. Ann Surg 2018;268:725-30. [Crossref] [PubMed]
- Kargar S, Shiryazdi SM, Zare M, et al. Comparison of postoperative short-term complications after laparoscopic transabdominal preperitoneal (TAPP) versus Lichtenstein tension free inguinal hernia repair: a randomized trial study. Minerva Chir 2015;70:83-9. [PubMed]
- Sekhon Inderjit Singh HK, Massey LH, Arulampalam T, et al. Chronic groin pain following inguinal hernia repair in the laparoscopic era: Systematic review and meta-analysis. Am J Surg 2022;224:1135-49. [Crossref] [PubMed]
- Hidalgo NJ, Guillaumes S, Bachero I, et al. Bilateral inguinal hernia repair by laparoscopic totally extraperitoneal (TEP) vs. laparoscopic transabdominal preperitoneal (TAPP). BMC Surg 2023;23:270. [Crossref] [PubMed]
- The Royal College of Surgeons of England. Commissioning Guide: Groin Hernia. British Hernia Society; 2013.
- Stahlman S, Fan M. Incidence of inguinal hernia and repair procedures and rate of subsequent pain diagnoses, active component service members, U.S. Armed Forces, 2010-2019. MSMR 2020;27:11-6. [PubMed]
- Palser TR, Swift S, Williams RN, et al. Variation in outcomes and use of laparoscopy in elective inguinal hernia repair. BJS Open 2019;3:466-75. [Crossref] [PubMed]
- Hidalgo NJ, Guillaumes S, Bachero I, et al. Trends and predictors of laparoscopic bilateral inguinal hernia repair in Spain: a population-based study. Surg Endosc 2023;37:4784-94. [Crossref] [PubMed]
- Finley DS, Rodriguez E Jr, Ahlering TE. Combined inguinal hernia repair with prosthetic mesh during transperitoneal robot assisted laparoscopic radical prostatectomy: a 4-year experience. J Urol 2007;178:1296-9; discussion 1299-300. [Crossref] [PubMed]
- Qabbani A, Aboumarzouk OM, ElBakry T, et al. Robotic inguinal hernia repair: systematic review and meta-analysis. ANZ J Surg 2021;91:2277-87. [Crossref] [PubMed]
- Engan C, Engan M, Bonilla V, et al. Description of robotically assisted single-site transabdominal preperitoneal (RASS-TAPP) inguinal hernia repair and presentation of clinical outcomes. Hernia 2015;19:423-8. [Crossref] [PubMed]
- Solaini L, Cavaliere D, Avanzolini A, et al. Robotic versus laparoscopic inguinal hernia repair: an updated systematic review and meta-analysis. J Robot Surg 2022;16:775-81. [Crossref] [PubMed]
- Prabhu AS, Carbonell A, Hope W, et al. Robotic Inguinal vs Transabdominal Laparoscopic Inguinal Hernia Repair: The RIVAL Randomized Clinical Trial. JAMA Surg 2020;155:380-7. [Crossref] [PubMed]
- Ayuso SA, Marturano MN, Katzen MM, et al. Laparoscopic versus robotic inguinal hernia repair: a single-center case-matched study. Surg Endosc 2023;37:631-7. [Crossref] [PubMed]
- Ephraim K, Haggai B, Mohammad A, et al. Learning curve of robotic inguinal hernia repair in the hands of an experienced laparoscopic surgeon: a comparative study. J Robot Surg 2022;16:1307-12. [Crossref] [PubMed]
- Tatarian T, Nie L, McPartland C, et al. Comparative perioperative and 5-year outcomes of robotic and laparoscopic or open inguinal hernia repair: a study of 153,727 patients in the state of New York. Surg Endosc 2021;35:7209-18. [Crossref] [PubMed]
- Proietti F, La Regina D, Pini R, et al. Learning curve of robotic-assisted transabdominal preperitoneal repair (rTAPP) for inguinal hernias. Surg Endosc 2021;35:6643-9. [Crossref] [PubMed]
- Haidenberg J, Kendrick ML, Meile T, et al. Totally extraperitoneal (TEP) approach for inguinal hernia: the favorable learning curve for trainees. Curr Surg 2003;60:65-8. [Crossref] [PubMed]
- Schouten N, Simmermacher RK, van Dalen T, et al. Is there an end of the "learning curve" of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 2013;27:789-94. [Crossref] [PubMed]
- McCormack K, Wake B, Perez J, et al. Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 2005;9:1-203. iii-iv. [Crossref] [PubMed]
- Kudsi OY, Kaoukabani G, Bou-Ayash N, et al. A comparison of clinical outcomes and costs between robotic and open ventral hernia repair. Am J Surg 2023;226:87-92. [Crossref] [PubMed]
- Kolachalam R, Dickens E, D'Amico L, et al. Early outcomes of robotic-assisted inguinal hernia repair in obese patients: a multi-institutional, retrospective study. Surg Endosc 2018;32:229-35. [Crossref] [PubMed]
- Awad MA, Buzalewski J, Anderson C, et al. Robotic Inguinal Hernia Repair Outcomes: Operative Time and Cost Analysis. JSLS 2020;24:e2020.00058.
- Kakiashvili E, Bez M, Abu Shakra I, et al. Robotic inguinal hernia repair: Is it a new era in the management of inguinal hernia? Asian J Surg 2021;44:93-8. [Crossref] [PubMed]
- Bou-Ayash N, Gokcal F, Kudsi OY. Robotic Inguinal Hernia Repair for Incarcerated Hernias. J Laparoendosc Adv Surg Tech A 2021;31:926-30. [Crossref] [PubMed]
- Miller BT, Prabhu AS, Petro CC, et al. Laparoscopic versus robotic inguinal hernia repair: 1- and 2-year outcomes from the RIVAL trial. Surg Endosc 2023;37:723-8. [Crossref] [PubMed]
- Hsu JL, Kelley JK, Zambito GM, et al. Comparison of Robotic, Laparoscopic, and Open Unilateral Repair of Non-recurrent Inguinal Hernia. Am Surg 2023;89:4793-800. [Crossref] [PubMed]
- Zhao F, Wang B, Chen J. Comparison between robotic and laparoscopic inguinal hernia repair in Caucasian patients: a systematic review and meta-analysis. Ann Transl Med 2021;9:885. [Crossref] [PubMed]
- Gundogdu E, Guldogan CE, Ozmen MM. Bilateral Inguinal Hernia Repair: Robotic TAPP Versus Laparoscopic TEP. Surg Laparosc Endosc Percutan Tech 2020;31:439-43. [Crossref] [PubMed]
- Spencer Netto F, Quereshy F, Camilotti BG, et al. Hospital costs associated with laparoscopic and open inguinal herniorrhaphy. JSLS 2014;18:e2014.00217.
- Perez AJ, Strassle PD, Sadava EE, et al. Nationwide Analysis of Inpatient Laparoscopic Versus Open Inguinal Hernia Repair. J Laparoendosc Adv Surg Tech A 2020;30:292-8. [Crossref] [PubMed]
- Lam CS, Dhedli PK, Russell S, et al. Cost-Effectiveness of Laparoscopic and Open Pediatric Inguinal Hernia Repair. J Laparoendosc Adv Surg Tech A 2022;32:805-10. [Crossref] [PubMed]
- Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009;13:407-14. [Crossref] [PubMed]
- Eckhoff JA, Müller DT, Brunner SN, et al. Do the costs of robotic surgery present an insurmountable obstacle? A narrative review. International Journal of Abdominal Wall and Hernia Surgery 2023;6:71-6. [Crossref]
Cite this article as: Xie J, Koo DC, Lee MJ, Sugiyama G. The evolution of minimally invasive inguinal hernia repairs. Ann Laparosc Endosc Surg 2024;9:13.


