Littre’s hernia: a case report of a rare intraoperative finding
Highlight box
Key findings
• A herniating mass continuous with the ileum may represent Littre’s hernia, or a herniating Meckel’s diverticulum. Symptomatic Meckel’s diverticulum requires treatment with diverticulectomy, wedge resection, or ileal segment resection. Asymptomatic cases do not require surgical intervention.
What is known and what is new?
• It is known that Littre’s hernia is the protrusion of a Meckel’s diverticulum through an abdominal opening. This manuscript adds to the existing, but limited, evidence that Littre’s hernia can complicate umbilical hernias. Further, this manuscript demonstrates the operative approach to resolving this type of hernia without the use of mesh. Lastly, this manuscript points out that Littre’s hernia may be mistaken for a malignant mass.
What is the implication, and what should change now?
• Surgeons need to be aware of the diagnosis of Littre’s hernia. Further, they must be prepared to tailor surgical treatment to each individual case, as treatments vary.
Introduction
A Meckel’s diverticulum (MD) is a remnant of the omphalomesenteric duct through which the fetal midgut communicates with the umbilical vesicle until the 5th week of gestation. The mucosa of these diverticula may contain gastric (23–50%), pancreatic (5–16%) or colonic tissue (1). Its reported incidence ranges from 0.6–4% making it the most common congenital anomaly of the intestinal tract (2). MD is most commonly clinically silent and present in 2% of the adult population. When symptoms are present, they can include gastrointestinal bleeding, bowel obstruction, inflammation and/or perforation. Littre’s hernia (LH) is a rare complication of MD in which a MD is contained within a hernia sac. Although MD is more common in men, LH is more common in women likely due to the higher incidence of obturator and femoral hernias. LH typically presents as an inguinal, femoral, or umbilical hernia. Previous reports have estimated a 1% incidence of LH among all cases of MD. While the true incidence of LH is unknown, only 67 symptomatic cases have been previously described in adults, with nine reports demonstrating LH localized at the umbilicus (3-23).
All but one of the case reports on umbilical LH are pediatric, as the presentation in adults is unusual. It is generally poorly visualized by ultrasound or computed tomography (CT) and does not present with specific signs or symptoms (24). It is typically found intraoperatively during the hernia repair and confirmed by pathology. All symptomatic MD are typically resected but there is controversy regarding resection of incidentally found asymptomatic MD. Previously, reports describe single stage herniorrhaphy with or without diverticulectomy and/or small bowel resection as well as two-stage laparoscopic surgery as possible interventions for umbilical LH (4-11). We describe the case of an umbilical LH repaired laparoscopically, employing partial bowel resection including the MD and foregoing the use of mesh in a patient presenting for elective repair of a symptomatic umbilical hernia. We present the following case in accordance with the CARE reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-22-45/rc).
Case presentation
We present the case of a 59-year-old obese male [body mass index (BMI) of 40.87 kg/m²] with a previous medical history of hypertension, hypercholesterolemia, and type 2 diabetes mellitus who initially presented to the general surgery office with complaints of an umbilical hernia which had been increasing in size with worsening tenderness for over 2 years. He reported no history of smoking or drinking, and there was no relevant family history. On physical examination, he exhibited tenderness overlying the umbilical hernia with reducibility. The patient denied obstructive symptoms such as changes in bowel movements, nausea, or vomiting. Additionally, he denied hematochezia on review of symptoms.
An elective laparoscopic umbilical hernia repair with mesh was scheduled. The patient was brought to the operative suite and placed in the supine position. Once adequate general endotracheal anesthesia was achieved, the patient was positioned appropriately with all pressure points protected. The abdomen was entered via a left upper quadrant incision at Palmer’s point followed by insertion a transparent 12 mm trocar using a direct view technique in the mid upper abdomen. The abdomen was then insufflated to 15 mmHg pressure. Two additional ports were placed under direct vision: the first 10 mm port placed at the level of the umbilicus along the right anterior axillary line and a second 5 mm port placed on the left side of the abdomen at the same level.
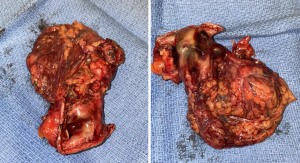
A portion of ileum along with omentum was found herniating through the umbilical defect. Upon dissection of the hernia sac and moderate adhesions, a mass-like structure contiguous with the ileum was reduced from the hernia defect. Intraoperatively upon gross inspection, it was presumed to be a malignant mass versus an incarcerated MD, thus a 4–5 cm ileal bowel resection was undertaken. The specimen was removed through the umbilical defect after the skin and hernia sac were opened, partially excised and sent for pathology. The indication for small bowel resection was two-fold: one—due to clinical suspicion for a mass of unknown etiology and two—due to significant adhesions and concern for viability of this segment of bowel. The resected specimen can be seen in Figure 1. The entirety of the bowel was then inspected for other masses or lesions, but no other gross abnormalities were identified. Because of the need for bowel resection and escalation of wound class, we elected to proceed with a primary closure of the hernia and omit the use of mesh in attempts to mitigate infectious complications. The abdominal wall defect was approximated and closed under minimal tension with an absorbable monofilament suture. 0-vicryl suture was used to close the fascia of the 12-mm trocar site. The remaining port sites were irrigated and closed with 4-monocryl in a subcuticular fashion. An abdominal binder with a bandage with wicking action and absorbency, was placed over the hernia site to provide countertraction and reduce dead space. Pathology later confirmed that the resected bowel was indeed a MD, confirming an umbilical LH.
The patient recovered without postoperative complications and was discharged home on post-operative day one. The patient had no recurrence of symptoms during a 6-month follow-up period. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
MD is a congenital anomaly that is largely asymptomatic in 90% of cases. It is typically described by the “rule of 2s” in which the MD is seen in 2% of the population, diagnosed under 2 years of age, measures 2 inches in length, 2 cm in diameter, lies 2 feet proximal to the ileocecal junction, is 2× more common in males and is symptomatic in 2% of patients. Park et al. demonstrated in a review of 1,476 patients with MD—that when symptomatic, most children presented with obstruction while most adults presented with bleeding (25). Obstructive MD can occur by way of various mechanisms, including intussusception, volvulus around the umbilical attachment or incarceration/strangulation within a hernia. “The Mayo Clinic Experience” review identified four risk factors predisposing to symptomatic MD in adults: age less than 50 years, male sex, diverticulum length greater than 2 cm and the presence of histologically abnormal tissue (25).
LH, however, occurs more frequently in women (60.4%) (26). LH occurs in the inguinal region 50% of the time, femoral 20%, umbilical and others 10%. Our case is rare as it describes an umbilical LH incidentally found during a routine umbilical hernia repair. Less than 10 previous umbilical LH have been reported in the literature.
Our patient was asymptomatic from the MD however, symptoms that can alert the surgeon to the possibility of a LH include a history of rectal bleeding, incomplete reduction or enterocutaneous fistula in a patient with a hernia (27,28). Most symptomatic cases present with non-specific symptoms of abdominal pain and occasional anorexia with malaise. Signs and symptoms of intestinal obstruction in LH are reported in 34% of cases (3). Technetium-99m scan can confirm the diagnosis pre-operatively but is often unnecessary and costly.
The management of MD is largely dictated by clinical presentation. If symptomatic, surgical resection is indicated. This can be done by means of diverticulectomy, wedge resection or ileal segment resection depending on the integrity of bowel and presence of ectopic tissue within the MD. When asymptomatic or incidentally diagnosed on imaging, foregoing surgical resection is preferred although optimal management remains controversial. In an epidemiologic, population-based study Cullen et al. recommended resection in patients younger than 80 years (29). The paper published by the Mayo Clinic experience recommended removing all incidental diverticula that fulfill any of the 4 criteria identified to be associated with symptomatic MD (25). It remains unresolved whether diverticulectomy alone is sufficient in resection of MD versus a small bowel resection. Patients with ectopic tissue can have indirect involvement present as ulceration of small bowel adjacent to the diverticulum (30). There can also be involvement of the base of the diverticula. It is unclear whether retained ectopic tissue will become symptomatic (30).
Morbidity and mortality of surgical resection of MD is generally low as reported by the literature. In one small study the morbidity and mortality in a group of asymptomatic patients who underwent MD resection were found to be 20% and 3% (31). However, the complications did not correlate directly with the diverticulectomy itself. In our case presentation the Meckel’s was resected as a safer alternative in the setting of a mass of unknown etiology and significant adherence to the surrounding bowel in this chronic umbilical hernia. Regarding the use of mesh, one systematic review of 53 cases of LH reported MD resection in all patients but the use of mesh in only 9 cases (17%), while the remaining underwent primary suture repair (3). Although it is unknown how many mesh repairs were complicated by mesh infection, only four patients experienced post-operative complications including wound dehiscence and minor surgical site infections (3). It is understood that the risk of field contamination was the primary factor for avoiding the use of mesh. It is important to note that most of the cases were reported prior to the 2000s. It is possible that data observing more recent LH repairs would reflect a higher use of mesh in patients without incarceration/strangulation or perforation.
The management of routine umbilical hernias largely relies on mesh to significantly reduce recurrence. Various techniques have been described for placement of mesh in ventral hernia repairs (32). Recent literature largely favors a pre-peritoneal approach to mesh placement versus an intra-peritoneal onlay approach due to increased cost-effectiveness, decreased post-operative complications and decreased recurrence (33,34). It is possible that this approach can be employed in cases of LH without significant adhesions or other technical factors prohibiting this. Due to the complexities of this case including the suspicion for malignancy, partial bowel resection and adhesions affecting the peritoneal planes, mesh was not utilized in the repair. Although the risk of hernia recurrence is higher without mesh, any potential complications of mesh placement were avoided.
Conclusions
In this case report, we identified a LH at the time of surgery for an elective umbilical hernia repair. Intra-operatively, the contents of the hernia sac included a small bowel mass of unknown etiology. It was resected along with a portion of bowel and subsequently returned as a MD on pathology. Less than 10 reports of umbilical LH exist within the literature. Presentation is non-specific and pre-operative diagnosis is thus difficult as in this case. The unknown etiology of the mass in this patient as well as the presence of adhesions and bowel resection prohibited the use of mesh in the umbilical hernia repair, although it is understood that this likely elevates the patient’s risk for hernia recurrence. This unique case report presents the effective management of an incidentally discovered umbilical LH without the use of mesh. Follow-up will dictate further management as it pertains to hernia recurrence.
The patient was overall happy with the treatment they received. He reported gratitude for being able to get back to his normal routine without the discomfort associated with a symptomatic LH.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-22-45/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-22-45/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-22-45/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Méndez-García C, Suárez-Grau JM, Rubio-Chaves C, et al. Surgical pathology associated with Meckel’s diverticulum in a tertiary hospital: 12 year review. Rev Esp Enferm Dig 2011;103:250-4. [Crossref] [PubMed]
- Kuru S, Kismet K. Meckel's diverticulum: clinical features, diagnosis and management. Rev Esp Enferm Dig 2018;110:726-32. [Crossref] [PubMed]
- Schizas D, Katsaros I, Tsapralis D, et al. Littre's hernia: a systematic review of the literature. Hernia 2019;23:125-30. [Crossref] [PubMed]
- Ariyoshi Y, Suto T, Umemura A, et al. Two-stage laparoscopic surgery for incarcerated umbilical Littre's hernia in severely obese patient: a case report. Surg Case Rep 2020;6:245. [Crossref] [PubMed]
- Cikman O, Kiraz HA, Ozkan OF, et al. An extremely rare complication of Meckel's diverticulum: enterocutaneous fistulization of umbilical hernia. Arq Bras Cir Dig 2015;28:152-3. [Crossref] [PubMed]
- Naveed F, Passeri D, Ilano A. Incidental finding of Meckel’s diverticulum in an umbilical hernia in a 60-year-old man. Open Access Surg 2012;5:39-41. [Crossref]
- Kibil W, Pach R, Szura M, et al. Adherent umbilical hernia containing Meckel's diverticulum resected due to intraoperative injury. Przegl Lek 2012;69:197-200. [PubMed]
- Kurnicki J, Wrzesińska N, Kabala P. Meckel's diverticulum incarcerated in an umbilical hernia--case report. Pol Przegl Chir 2011;83:386-8. [Crossref] [PubMed]
- Sengul I, Sengul D, Avcu S, et al. Gangrenous meckel's diverticulum in a strangulated umbilical hernia in a 42 year-old woman: a case report. Cases J 2010;3:10. [Crossref] [PubMed]
- Tiu A, Lee D. An unusual manifestation of Meckel's diverticulum: strangulated paraumbilical hernia. N Z Med J 2006;119:U2034. [PubMed]
- Castleden WM. Meckel's diverticulum in an umbilical hernia. Br J Surg 1970;57:932-4. [Crossref] [PubMed]
- Krishnaswamy P, Krawitz R. Littre hernia: rare presentation of computed tomography-diagnosed strangulated umbilical Littres hernia repaired with mesh. ANZ J Surg 2021;91:1927-8. [Crossref] [PubMed]
- Kehagias D, Iliopoulos E, Maroulis I, et al. Strangulated femoral hernia without intestinal obstruction? Be aware of Meckel's diverticulum: a case report of a Littre's hernia. BMJ Case Rep 2021;14:e243840. [Crossref] [PubMed]
- Evola G, Piazzese E, Bonanno S, et al. Complicated Littre's umbilical hernia with normal Meckel's diverticulum: A case report and review of the literature. Int J Surg Case Rep 2021;84:106126. [Crossref] [PubMed]
- Usman A, Rashid MH, Ghaffar U, et al. Littré's Hernia: A Rare Intraoperative Finding. Cureus 2020;12:e11065. [PubMed]
- Feriani N, Ghezala HB. Littre's hernia in a Tunisian emergency department: a rare image. Pan Afr Med J 2020;37:164. [Crossref] [PubMed]
- Erdoğan A, Bostanoğlu A. A rarely encountered case: A neuroendocrine tumor in strangulated Littre's hernia. Ulus Travma Acil Cerrahi Derg 2020;26:632-4. [PubMed]
- Bains HK, Agostinho N, Hamilton AE, et al. What is in the sac? Littré hernia. ANZ J Surg 2020;90:896-8. [Crossref] [PubMed]
- Pinto J, Viana CM, Pereira A, et al. Littré's hernia. BMJ Case Rep 2019;12:e228784. [Crossref] [PubMed]
- Paasch C, De Santo G, Look P, et al. Laparoscopic Treatment of an Incarcerated Meckel's Diverticulum in a Femoral Hernia. Case Rep Surg 2019;2019:3140706. [Crossref] [PubMed]
- Curmi A, Dimech AP, Dalli R, et al. A Rare Case of Acquired Transthoracic Littre's Hernia. Surg J (N Y) 2019;5:e150-e153. [Crossref] [PubMed]
- Kosmidis C, Mantalovas S, Sapalidis K, et al. Rare Co-Existence of Amyand's and Littre's Hernia Treated with Appendectomy and Bowel Resection Followed by Polypropylene Mesh Application. Am J Case Rep 2018;19:1422-4. [Crossref] [PubMed]
- Bouhout T, Serji B, Egyir EU, et al. An unusual complication of Meckel’s diverticulum: Littre’s hernia. Pan Afr Med J 2018;31:243. [Crossref] [PubMed]
- Skandalakis PN, Zoras O, Skandalakis JE, et al. Littre hernia: surgical anatomy, embryology, and technique of repair. Am Surg 2006;72:238-43. [Crossref] [PubMed]
- Park JJ, Wolff BG, Tollefson MK, et al. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg 2005;241:529-33. [Crossref] [PubMed]
- Lauschke H, Kaminski M, Stratmann H, et al. Littré's hernia--clinical aspects and review of the history. Chirurg 1999;70:953-6. [Crossref] [PubMed]
- Mishalany HG, Pereyra R, Longerbean JK. Littre's hernia in infancy presenting as undescended testicle. J Pediatr Surg 1982;17:67-9. [Crossref] [PubMed]
- Pampal A, Aksakal ED. Littre hernia in childhood: a case report with a brief review of the literature. Afr J Paediatr Surg 2011;8:221-4. [Crossref] [PubMed]
- Cullen JJ, Kelly KA, Moir CR, et al. Surgical management of Meckel's diverticulum. An epidemiologic, population-based study. Ann Surg 1994;220:564-8; discussion 568-9. [Crossref] [PubMed]
- Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med 2006;99:501-5. Erratum in: J R Soc Med 2007;100:69. [Crossref] [PubMed]
- Lüdtke FE, Mende V, Köhler H, et al. Incidence and frequency or complications and management of Meckel's diverticulum. Surg Gynecol Obstet 1989;169:537-42. [PubMed]
- Skolimowska-Rzewuska M, Romańczuk M, Mitura B, et al. Laparoscopic transabdominal preperitoneal repair (umbilical TAPP) versus open ventral patch repair for medium size umbilical hernias in overweight and obese patients. Wideochir Inne Tech Maloinwazyjne 2022;17:170-8. [Crossref] [PubMed]
- Prasad P, Tantia O, Patle NM, et al. Laparoscopic ventral hernia repair: a comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. J Laparoendosc Adv Surg Tech A 2011;21:477-83. [Crossref] [PubMed]
- Sarli L, Pietra N, Choua O, et al. Laparoscopic hernia repair: a prospective comparison of TAPP and IPOM techniques. Surg Laparosc Endosc 1997;7:472-6. [Crossref] [PubMed]
Cite this article as: Ghorishi A, Levin N, Rajalingam K, Sanchez D. Littre’s hernia: a case report of a rare intraoperative finding. Ann Laparosc Endosc Surg 2023;8:13.