
Adjustable gastric banding
Introduction
Obesity is an important social health problems of today. In addition, the increase in the incidence in the world is remarkable. Obesity not only reduces the quality of life but also shortens the duration of life with the complications it brings. It is one of the most important causes of under-40 years deaths in developed countries. Inadequate success in the treatment with diet, exercise and medical methods has directed researchers to different searches, and hormones and mediators that are thought to be the source of obesity with surgical interventions have become the focus of current research. Although various surgical methods have been compared for many years in terms of their advantages and disadvantages, no single method that can be accepted as the gold standard treatment option has yet been developed. Due to the fact that it is a reversible surgery, ease of application and early results, the adjustable gastric band (AGB) operation has become common practice for the last 20 years. However, its long-term results, inadequate weight loss and increased complications, caused to a rise in the popularity of other restrictive and malabsorptive procedures and the avoidance of AGB operations. Especially, the interest in sleeve gastrectomy (SG), another restrictive procedure, caused a significant reduction in the number of gastric bands.
History of gastric banding
Gastric banding is based on the principle of forming a small volume pouch near the stomach by wrapping the fundus with various synthetic grafts and limiting the passage to the distal part of the stomach. The main purpose is to limit oral intake. For this purpose, Wilkinson performed the first study on this subject using a Marlex graft wrapped around the stomach in 1976 (1). The device, which is nowadays described as the Swedish Adjustable Gastric Band (SAGB), was first described by two Swedish surgeons called Hallberg and Forsell in 1985 (2). In the same period, clinical use of a silicone-based (which is previously used in many parts of the human body for a variety of purposes and is easily accepted by the organism with minimal inflammatory effect) inflatable band originally known as “the American Lap-Band” (LB) is reported by the Lubomyr Kuzmak, a Ukrainian surgeon working in the USA (3). SAGB and Lap-Band systems both had a port under the skin that is connected to the band with a separate channel in which the gastric band opening could be resized by injecting/aspirating saline from this port. In 1986, Kuzmak reported that this new band had better weight loss (WL) and less complication rates than the unadjustable silicone band, which he was introduced in 1983 (4).
Belachew et al. reported that laparoscopic application of AGB was successfully performed in animals for the first time (5). Subsequently, by the Broadbent et al. have been reported for the first time that the laparoscopic adjustable gastric banding (LAGB) procedure was found to have significantly fewer complications and had similar effects on weight loss parallel to the open method (6). All these advantages of LAGB have replaced vertical banded gastroplasty (VBG), which was the main restrictive procedure for the treatment at that time, and subsequently began to be the most commonly used bariatric surgery for the obesity (7).
The procedure has a short learning curve, short operation time and hospital stay and it is also can be performed as daily operations in many places, it is reversible and does not changes the anatomy, the amount of restriction in food intake can be adjusted according to the amount of the liquid injected into the patient's band, and it has successful early postoperative results (8). Because of all these reasons mentioned, LAGB has found itself a widespread application field and has become one of the most applied surgical procedure worldwide (9).
However, since its peak in 2009, the amount of LAGB being performed has decreased over time due to prolonged complications such as weight gain, obstructive symptoms, dysphagia, band slippage, esophageal dilatation, esophagitis, gastric erosion and port site infections and correlated to this in 2017, only 6,300 new procedures (3% of all bariatric surgeries) were performed as LAGB (10).
LAGB technique
The band placement procedure which is called the “perigastric technique”, was first described in 1993 by a Belgian surgeon, Dr. Belachew (5). One of the main complications of this technique was the gastric band slippage and pouch dilatation (11). After a while, Dr. Forsell and Hallbers introduced a new method called: “The Pars Flaccida Technique” (12). After several randomized controlled studies (RCT) on this subject, they reported that the pars flaccida technique significantly reduces the rates of slippage (13,14). This technique includes a minimal dissection near the stomach and lesser sac to place the band a higher position. In addition, this smaller gastric pouch above the band, which contains virtually no fundus, contributed to the reduction of pouch dilatation, which is theoretically responsible for failure in WL and weight regain, as well as chronic reflux (11).
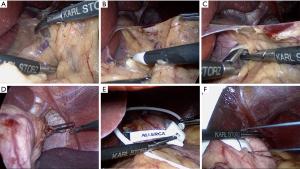
Typically, in a standard LAGB procedure, the following steps are followed (Figure 1): After creating pneumoperitonium with sufficient intraabdominal pressure, trocars and liver retractor are placed. The dissection starts from the greater curvature and continues towards the diaphragm, and at this stage, the left paraesophageal ligament dissection is completed and the left crus is exposed. The calibration tube is placed into the stomach by the anesthetist and the balloon at the end of the calibration tube is inflated with approximately 15–20 mL of fluid and pulled back towards the esophagus. Thus, the position where the band will be placed is determined. Then, the pars flacida is opened to enter the lesser sac level, and a retrogastric tunnel is created by dissection made from the lesser curvature close to the stomach, just below the calibration balloon. A long atraumatic instrument is advanced through this tunnel, the appropriate end of the gastric band is attached to this instrument, and the gastric band is pulled back from this tunnel and the position of the band is adjusted according to the calibration tube placed before, and then the lock mechanism of the band is closed. To prevent band migration following placement of the band, it is fixed with ventro-ventral sutures with two or three stitches that made from the anterior and lateral surfaces of the stomach. The tube of the band is taken out of the abdomen through the appropriate trocar site to be connected with the injection port and connected with each other. If the stoma is too large, weight loss will be insufficient, but if it is too narrow, there is a risk of postoperative food intolerance. Once the stoma width is adjusted, the port is placed over the anterior rectus sheath and secured with sutures. To prevent vomiting in the early postoperative period, most surgeons postpone their fluid injection to the band until the first visit.
Results and outcomes of the adjustable gastric banding
Adjustable gastric band operations have been frequently done in surgical practice for reasons such as requiring relatively less technical skills and laparoscopic applicability. Many studies have shown that the effectiveness of LAGB has comparable results with other procedures in providing weight loss (15).
In 2008, Cunneen et al. published the results of two separate band systems, SAGB and LB applications, in a meta-analysis which includes 28,980 patients. In this meta-analysis they reported the 3-year mean SAGB and LB excess weight loss was (56.36%/50.20%, and it was statistically significant as was the resolution of diabetes (61.45%/60.29%), and hypertension (62.95%/43.58%) (16). In the meta-analysis published by O’Brien et al. in 2019 which is comparing long-term follow-up results of LAGB, RYGB, LSG and biliopancreatic diversion (BPD) procedures for 10 years or more; reported EWL rates as 45.9% for LAGB, 56.7% for RYGB, 58.3% for LSG and 74.1% for BPD. This systematic review confirmed that LAGB showed similar results with other methods in achieving long-term weight loss (17). Chapman et al. (9) reported that LAGB achieved less WL in the first 2 years after surgery compared to RYGB, but there was no significant difference between these two procedures in terms of WL between the 2nd and 4th years.
O'Brien et al. has revealed similar results in their systematic review published in 2006 and showed that BPD is the most effective procedure for WL by providing an average of 74.4% EWL in the mid-term. Although RYGB provided more weight loss than LAGB in the first two years, it reported that there was no significant difference between the two techniques in weight loss in the mid-term (3–10 years) (18).
In contrast, in the meta-analysis published by Golzarand et al. in 2017; they reported that the EWL rate for LAGB was 47.4% in the long term over the 10-year period, while this rate was 63.5% for RYGB, and that RYGB was superior to LAGB in terms of WL in the long term (19). Again, these results were similar to those of O’Brien et al. In 2019.
There are very few studies comparing LAGB with LSG. In the randomized controlled trial of Himpens et al. containing 40 patients for LAGB and LSG, they reported that there was a significant difference for the LSG group in the 1st and 3rd years in terms of weight loss, decreased BMI and decreased EWL (57.7% and 48%) when compared to LAGB (20).
Li et al. reported similar results in their meta-analysis in 2019. In this meta-analysis, they revealed that there was no difference in terms of % EWL between LSG and LAGB groups in the first 3 months, but in the period between 6 months and 3 years, the % EWL rates and diabetes remission rates in the LSG group were statistically better than the LAGB group. In addition, they reported that there was no significant difference in their effects on hypertension (21).
In contrast, in a study conducted in our own clinic, we also reported that, at the end of the first year, while the EWL rate was 60.3% in the LSG group, it was 45.3% in the LAGB group and that the LSG group was superior in comparison to LAGB in effective weight loss (22).
One of the most important criticisms of LAGB was its long-term band removal rates and its failure to achieve adequate WL. However, O'Brien et al. published their long-term results after LAGB in 2019, and overturned many of these claims (17). The authors reported an average of 45.9% EWL for all LAGB patients over a 10-year follow-up or later, as well as a significant reduction in reoperation rates associated with improved band design and better quality of patient education due to with improved understanding of how the band works.
Furbetta et al. published the 20-year long-term results that included 3,566 LAGB patients in 2018 and reported that EWL rates were 49%, 52.6% and 59.2%, and pouch dilatation and erosion rates were 5.8% and 2.5% in 10, 15 and 20 years (23).
Complications of gastric banding
After LAGB surgeries, various complications can occur related to the band or the port (Table 1). Early studies have shown that short term complications after LAGB are particularly low when compared to the other complicated procedures (24). Even compared to RYGB and LSG, short-term results of LAGB have been shown to be significantly superior (25). As long-term results began to appear, it was observed that serious complications that overshadowed successful results in the early period began to emerge, and in fact, early results did not reflect the effectiveness of LAGB. In their study of 12-year long-term follow-up results of Himpens et al., reported that 22% of LAGB patients had minor complications and 39% major complications including 28% band erosion (26). In addition, O'Brien et al. have also reported nearly 20 years of long-term LAGB experiences (17). In this study, they reported that the need for reoperation was the weakness of the LAGB procedure and that the need for revision was over 50% in the LAP-Band 10 cm era, but with the development of techniques and the use of LAP-Band AP, this rate decreased sharply below to 10%.
Table 1
| Minor complications |
| Acute stomal obstruction |
| Minor bleeding |
| Minor port infection |
| Delayed gastric emptying |
| Major complications |
| Gastric/oesophagial perforation |
| Hemorrhage |
| Band erosion |
| Band slippage/prolapse |
| Port/tubing malfunction |
| Port/tube leakage |
| Oesophagial dilatation |
Another important parameter after bariatric surgery is morbidity and mortality. In a meta-analysis conducted by Chang et al., they reported that complication rates after RYGB were 21%, whereas complication rates after LAGB were 13% and LAGB had the lowest complication rate (27). The number of randomized controlled trials comparing morbidity and mortality rates of bariatric surgery types is very limited. In a study of Angrisani et al. published the 10-year RCT results of RYGB and LAGB procedures and the authors found that patients in the RYGB group had a higher early complication rate (8.3% vs. 0%) and long-term complication rate (herniation and obstruction rate 4.7%) when compared to the LAGB group (28). In a study published on mortality rates after bariatric surgery, Buchwald et al. (29) showed that mortality rates were twice the LAGB group in the first month after RYGB (0.1% vs. 0.2%). Similar results were obtained by Chang et al. and according to this meta-analysis, the perioperative and postoperative mortality rates after LAGB were 0.07% and 0.21%, while the same rates after RYGB were reported as 0.38% and 0.72%, respectively (27). For all these reasons, LAGB can be considered as a safer bariatric procedure in terms of perioperative and postoperative mortality in the early period.
Current status for AGB
With the advent of the AGB procedure, an important progress has been made in the development of bariatric surgery. With the adaptation of laparoscopic techniques to AGB surgery, there has been a serious increase in the popularity of such surgeries. As a restrictive method, LAGB, became very popular in the late 1990s as an alternative to open surgery and frequently applied LRYGB. LAGB has become the most popular obesity surgery in the USA because of its less complicated technique that can be applied faster, its early results on weight loss, morbidity and mortality, as well as its reversibility (30). However, while the international popularity of LAGB was around 42% in 2008, it decreased to around 18% in the period until 2011. The most important factors contributing to this downward trend in LAGB practice are due to the emergence of evidence questioning the long-term safety of the band, causing more serious late complications such as band erosion, slippage and gastric pouch dilatation in the long term (31). This is also in line with important evidence confirming the superiority of LRYGB and LSG over LAGB and that LAGB has a higher failure rate in achieving weight loss compared to other procedures (27,32). Some studies have shown that complication rates are as high as 40–50% in the long term, and reoperation rates are as high as 30% (18). As a result, the rate of revisional operations after LAGB is rapidly increasing today and many surgeons prefer to convert it to another bariatric procedure, such as RYGB or LSG, for revision surgery in patients with band removed after LAGB (33,34). Successful results in weight loss have been reported after both LSG and LRYGB. However, it has been reported that complication rates after revision surgeries are higher than primary surgeries (35). Revealing the consequences of long-term complications and revision surgeries after LAGB has a key role in understanding and reevaluating its role in the treatment of obesity.
Conclusion
LAGB is a remarkable procedure with its features such as requiring less technical skills, having a short learning curve, less early complications, successful short-term weight loss results, short hospital stay, maintaining normal anatomy and being completely reversible compared to other bariatric operations. With its remarkable early results, LAGB has found a wide range of applications for a period of time, and has reached a number of applications that will compete with other bariatric surgical procedures in its popular period. However, as long-term results began to emerge, such as failure in weight loss, increased weight regain and long-term complication rates, interest in the procedure disappeared. Other bariatric surgical procedures such as LSG, RYGB, OAGB, and SADS attract attention because of their long-term success in weight loss rates and improvement in metabolic diseases and relatively successful long-term complication rates (36).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mehmet Mahir Ozmen) for the series “Bariatric and Metabolic Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-2019-bms-06). The series “Bariatric and Metabolic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wilkinson LH, Peloso OA. Gastric (reservoir) reduction for morbid obesity. Arch Surg 1981;116:602-5. [Crossref] [PubMed]
- Hallberg D, Forsell I. ’. Ballongband vid behandling av massiv overvikt (Balloon band for the treatment of massive obesity). Svensk Kirwgi 1985;43:106.
- Kuzmak LI. Silicone gastric banding: a simple and effective operation for morbid obesity. Contemp Surg 1986;28:13-8.
- Kuzmak L I.. A preliminary-report on a silicone gastric banding for obesity. Clinical Nutrition 1986;5:73-7.
- Belachew M, Legrand M, Vincinti V, et al. Laparoscopic placement of adjustable silicone gastric band in the treatment of morbid obesity: how to do it. Obes Surg 1995;5:66-70. [Crossref] [PubMed]
- Broadbent R, Tracy M, Harrington P. Laparoscopic gastric banding: a preliminary report. Obes Surg 1993;3:63-7. [Crossref] [PubMed]
- Mason EE. Development and future of gastroplasties for morbid obesity. Arch Surg 2003;138:361-6. [Crossref] [PubMed]
- Chang SH, Stoll CRT, Song J, et al. The effectiveness and risks of bariatric surgery. An updated systematic review and meta-analysis 2003-2012. JAMA Surg 2014;149:275-87. [Crossref] [PubMed]
- Chapman AE, Kiroff G, Game P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery 2004;135:326-51. [Crossref] [PubMed]
- English WJ, DeMaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 2018;14:259-63. [Crossref] [PubMed]
- Fielding GA, Ren CJ. Laparoscopic adjustable gastric band. Surg Clin North Am 2005;85:129-40. [Crossref] [PubMed]
- Forsell P, Hallberg D, Hellers G. Gastric banding for morbid obesity: initial experience with a new adjustable band. Obes Surg 1993;3:369-74. [Crossref] [PubMed]
- O’Brien PE, Dixon JB, Laurie C, et al. A prospective randomized trial of placement of the laparoscopic adjustable gastric band: comparison of the perigastric and pars flaccida pathways. Obes Surg 2005;15:820-6. [Crossref] [PubMed]
- Di Lorenzo N, Furbetta F, Favretti F, et al. Laparoscopic adjustable gastric banding via pars flaccida versus perigastric positioning: technique, complications, and results in 2,549 patients. Surg Endosc 2010;24:1519-23. [Crossref] [PubMed]
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and metaanalysis. JAMA 2004;292:1724-37. [Crossref] [PubMed]
- Cunneen S A., Phillips E, Fielding G, et al. Studies of Swedish adjustable gastric band and Lap-Band: systematic review and meta-analysis. Surg Obes Relat Dis 2008;4:174-85. [Crossref] [PubMed]
- O'Brien PE, Hindle A, Brennan L, et al. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg 2019;29:3-14. [Crossref] [PubMed]
- O’Brien PE, McPhail T, Chaston TB, et al. Systematic review of medium-term weight loss after bariatric operations. Obes Surg 2006;16:1032-40. [Crossref] [PubMed]
- Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc 2017;31:4331-45. [Crossref] [PubMed]
- Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg 2006;16:1450-6. [Crossref] [PubMed]
- Li L, Yu H, Liang J, et al. Meta-analysis of the effectiveness of laparoscopic adjustable gastric banding versus laparoscopic sleeve gastrectomy for obesity. Medicine (Baltimore) 2019;98:e14735 [Crossref] [PubMed]
- Gündoğdu E, Bilgiç Cİ, Moran M, et al. Evaluation of the effects of laparoscopic adjustable gastric banding versus laparoscopic sleeve gastrectomy on weight loss. Eur Res J 2019;6:36-42.
- Furbetta N, Gragnani F, Flauti G, et al. Laparoscopic adjustable gastric banding on 3566 patients up to 20-year follow-up: Long-term results of a standardized technique. Surg Obes Relat Dis 2019;15:409-16. [Crossref] [PubMed]
- Taşkin M, Apaydin BB, Zengin K, et al. Stoma adjustable silicone gastric banding versus vertical banded gastroplasty for the treatment of morbid obesity. Obes Surg 1997;7:424-8. [Crossref] [PubMed]
- Chakravarty PD, McLaughlin E, Whittaker D, et al. Comparison of laparoscopic adjustable gastric banding (LAGB) with other bariatric procedures; a systematic review of the randomised controlled trials. Surgeon 2012;10:172-82. [Crossref] [PubMed]
- Himpens J, Cadie`re G-B, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg 2011;146:802-7. [Crossref] [PubMed]
- Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 2014;149:275-87. [Crossref] [PubMed]
- Angrisani L, Cutolo PP, Formisano G, et al. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 10-year results of a prospective, randomized trial. Surg Obes Relat Dis 2013;9:405-13. [Crossref] [PubMed]
- Buchwald H, Estok R, Fahrbach K, et al. Trends in mortality in bariatric surgery: a systematic review and metaanalysis. Surgery 2007;142:621-32. [Crossref] [PubMed]
- Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg 2009;19:1605-11. [Crossref] [PubMed]
- Chevallier JM, Zinzindohoué F, Blanche J, et al. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1,000 patients over 7 years. Obes Surg 2004;14:407-14. [Crossref] [PubMed]
- Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality inSwedish obese subjects. N Engl J Med 2007;357:741-52. [Crossref] [PubMed]
- Weber M, Müller MK, Michel JM, et al. Laparoscopic Roux-en-Y gastric bypass, but not rebanding, should be proposed as rescue procedure for patients with failed laparoscopic gastric banding. Ann Surg 2003;238:827-33. [Crossref] [PubMed]
- Dapri G, Cadière GB, Himpens J. Feasibility and technique of laparoscopic conversion of adjustable gastric banding to sleeve gastrectomy. Surg Obes Relat Dis 2009;5:72-6. [Crossref] [PubMed]
- Angrisani L, Vitiello A, Santonicola A, et al. Roux-en-Y gastric bypass versus sleeve gastrectomy as revisional procedures after adjustable gastric band: 5-year outcomes. Obes Surg 2017;27:1430-7. [Crossref] [PubMed]
- Campos GM, Khoraki J, Browning MG, et al. Changes in utilization of bariatric surgery in the United States from 1993 to 2016. Ann Surg 2020;271:201-9. [Crossref] [PubMed]
Cite this article as: Gundogdu E, Moran M. Adjustable gastric banding. Ann Laparosc Endosc Surg 2021;6:47.


