Emergency right colectomy: is there a role for minimally invasive surgery?—A systematic review and meta-analysis of short-term clinical outcomes
Introduction
With the advances in surgical skills and technology, laparoscopic surgery has gained wide acceptance as a safe and feasible alternative surgical strategy to open surgery (OS) in the management of benign and malignant colorectal disease (1,2).
Retrospective cohort studies have reported that laparoscopic colorectal resections in emergency settings are safe, and clinical benefits are well established such as in elective surgery. Lesser pain, shorter postoperative ileus and length of hospital stay and better quality of life have been recognized in many retrospective trials (3,4).
However, emergency laparoscopic colectomy is not widely practiced, as complicated colorectal diseases have been thought to be a contraindication to minimally invasive approach in many early reports. The reasons for such a difference in management strategies between elective and emergency cases are that patients with obstructing colorectal cancer or bowel perforation typically present systemically unwell and with often complicated intra-abdominal disease, and because of the substantial risk of injuring the distended bowel which potentially makes laparoscopy more challenging (5).
Furthermore, the need for emergency colorectal surgery is more frequent in patients aged more than 75 years, and elderly patients are generally considered frail due to the high rate of comorbidity.
All these issues could make laparoscopic surgery in emergency setting technically more challenging.
However, during the last years, successful emergency laparoscopic colectomies have been described, also in right-sided large bowel obstruction, and the use of laparoscopic approach in emergency settings rapidly increased during the last decade (6).
The guidelines of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) stated that “the open approach is required if the laparoscopic approach will not result in an oncologically sound resection” and “the decision to proceed laparoscopically should take into account the patient’s condition, including hemodynamic stability, extent of abdominal distension, the resectability of the carcinoma, and the surgeon’s ability to perform a curative resection in this setting” (7).
Traditionally, the most adopted treatment for colonic obstruction was emergency surgery without preoperative decompression. However, emergency surgery for acute bowel obstruction caused by colorectal cancer is related to morbidity rates of 40–60% and mortality of 3–11% (8). Thus, when patients are admitted for obstructing colonic disease, colorectal self-expanding metallic stents (SEMS) have been used successfully as a mean to bridge the need for emergent surgery to elective one. SEMS can increase the surgical safety by reducing the colonic distension and represents a helpful treatment for subsequent elective laparoscopic colectomy and one-stage anastomosis with fewer anastomotic leakages and less permanent ileostomies (9).
The study by Li et al. demonstrated that in selected emergency settings, laparoscopic-assisted (LA) right colectomy can be safely performed with comparable results to elective right colectomy in terms of intra-operative blood loss, postoperative complication and length of recovery (10).
However, research is still lacking in regards to whether laparoscopy can safely replace the traditional open technique for patients needing emergency right colectomy.
This systematic review and meta-analysis aims to present an evidence-based assessment of the clinical short-term outcomes of the laparoscopic versus open approaches in right colectomy performed in emergency settings, by analyzing clinical outcomes of safety and feasibility of the two techniques. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/ales-20-57).
Methods
The present systematic review and pooled-analysis was conducted according to the recommendations of the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) guidelines, the meta-analysis of observational studies in epidemiology checklist (MOOSE), and the Cochrane handbook for systematic reviews of interventions (11-13).
All stages of study search, selection, data extraction, methodological quality assessment and risk of bias analysis were carried out independently by two reviewers (M Podda and A Pisanu). Inconsistencies were resolved by mutual discussion, and based on the assessment by a third reviewer (S Di Saverio).
Ethics approval was not necessary for this study, as it did not involve single patient data.
Study identification
The following databases were searched: MEDLINE (via PubMed), Cochrane, Scopus, Web of Science and EMBASE. The search strategy combined the following MeSH terms and text words (Boolean searches) related to laparoscopic and open colectomy for the treatment of right colon emergencies: “Colon Cancer”, “Right Colectomy”, “Laparoscopy”, “Emergency”, “Intestinal Obstruction”, “Diverticulitis”. Reference lists of identified studies were searched manually, and the “related articles” function in PubMed was used. No restrictions were imposed on manuscript language or publication date.
The literature search was completed in February 2020.
Study selection
All titles and abstracts of the identified studies were assessed in order to analyze the results of non-randomized controlled trials (n-RCTs) and randomized controlled trials (RCTs) comparing LA and OS right colectomy for right colon emergencies (including obstructing or bleeding colon cancer and complicated cecal diverticulitis) to be included in the present meta-analysis. Where there was an overlap in patients’ cohorts of 2 studies or overlapping study periods were found, only the most recent and largest study was included in the pooled analysis.
All studies eligible for inclusion had to report clear definitions of the indications to perform emergency right colectomy, the description of the anastomosis techniques, and the description of at least one of the clinical outcomes.
All single-cohort studies and those studies in which data were not related only to right colectomy performed in emergency setting were excluded. Further exclusion criteria were: studies not specifying the patients selection criteria, studies not reporting data on the selected outcomes of interest or articles in which the outcomes of interest could not be calculated, studies that included other kind of colorectal resections other than right colectomies, case reports, editorials and review articles without original data.
Quality of evidence and risk of bias assessment
The grading of recommendations assessment, development and evaluation (GRADE) methodology was implemented for assessing the quality of evidence (14).
Furthermore, the risk of bias for the studies included in the systematic review and meta-analysis was assessed using the Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analyses, as only n-RCTs on this topic were expected (15).
Outcomes measures
The following primary outcomes were reviewed with the aim to assess safety and feasibility of LA and OS for emergency right colectomy: intra-operative blood loss, postoperative mortality, postoperative complications, anastomotic leakage, and surgical site infection.
Further secondary clinical outcomes were analyzed to assess other potential advantages and drawbacks of LA and OS in terms of: duration of operation, mean number of retrieved lymph nodes, radical R0 resection in case of cancer, time to flatus, time to bowel movements, time out from bed after surgery and length of postoperative hospital stay.
Data extraction
Data analyzed for each included article comprised the following predefined variables: study identifier (1st author, year of publication), study period, study location, study design, general characteristics of the study (inclusion criteria, exclusion criteria, surgical indications to right colectomy), anastomosis technique description, treatment arms (LA or OS) and number of enrolled patients, baseline characteristics of the patients (age, sex, BMI, previous operations, obstruction duration, tumor size, rate of T4 tumors) and the clinical short-term outcomes.
Statistical analysis
Variables for the meta-analysis were considered if they were reported by at least two studies. Meta-analysis was carried out using Reviewer Manager software (Review Manager-RevMan-version 5.3.5, 2014, The Nordic Cochrane Centre, Cochrane Collaboration, www.cochrane-handb ook.org). The odds ratio (OR) with 95% confidence interval (95% CI) was calculated for dichotomous variables, and the standardized mean difference (SMD) or the weighted mean difference (WMD) with 95% CI: for continuous variables.
A P value <0.05 was considered statistically significant.
When continuous data were presented as median and range, the method of Hozo et al. was applied to evaluate respective mean and standard deviations (16). Clinical and methodological heterogeneity across studies (variability in study design and risk of bias, variability in the participants, interventions and outcomes studied) was assessed using the Higgins’ I2 and Chi-Square tests. A P value of Chi-square test <0.10 with an I2 value >50% were considered as indicative of substantial heterogeneity. Fixed-effects model (Mantel-Haenszel) was applied if significant heterogeneity was absent. Conversely, a random-effects model was implemented if significant heterogeneity was found, in accordance with the method of DerSimonian and Laird (17).
Results
Study characteristics
A total of 79 references were identified through MEDLINE, Cochrane, Web of Science and EMBASE databases searching. Five more references were identified by searching reference lists of retrieved studies (Figure 1).
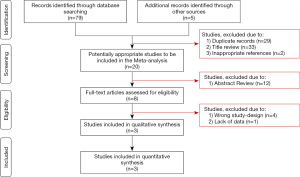
After removing 29 duplicates, two inappropriate references, and 33 more studies after title review, 20 studies had their abstracts evaluated to be included in the systematic review. After abstract review, 12 more studies were excluded, resulting in eight full-text articles assessed for eligibility. Four studies were then excluded due to wrong design, and one more due to lack of data.
Three n-RCTs comparing LA and OS were included for qualitative and quantitative synthesis (Table 1).
Table 1
| Author | Year of publication | Study type | Study period | Study location | Inclusion criteria | Exclusion criteria | Obstructing colon cancer, N [%] | Anastomosis technique | Follow-up | Newcastle-Ottawa scale quality assessment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lap | Open | Selection | Comparability | Outcome | |||||||||
| Li Z | 2015 | RCS | Jan 2011–Jun 2013 | Nanchang, China | All the patients had undergone a preoperative CT scan through which an occupying and obstructing lesion on the right colon from the cecum to the proximal transverse colon was diagnosed | Patients for whom a right hemicolectomy was performed but colon cancer was not confirmed by pathology after surgery; patients who had peritonitis, pericolic abscess or sepsis; patients with metastatic disease on preoperative work-up; patients with synchronous tumors or polyps that necessitated multivisceral resection and those for whom only segmental resection was performed | 10 [100] | 25 [100] | Side-to-side extracorporeal stapled anastomosis | NR | **** | ** | * |
| Li JCM£ | 2009 | RCS | Sep 2001–Jun 2006 | Hong Kong, China | Patients with an intra-operative diagnosis of complicated cecal diverticulitis who underwent emergency right hemicolectomy | NR | - | - | The ileocolic anastomosis is performed extracorporeally either hand-sewn or with two linear staplers (functional end-to-end anastomosis) | NR | **** | ** | * |
| Ng SSM | 2008 | RCS | Jul 2003–Jul 2006 | Hong Kong, China | Patients with obstructing right-sided colonic carcinoma who underwent emergency right hemicolectomy | Patients with peritonitis | 14 [100] | 29 [100] | The ileocolic anastomosis is performed extracorporeally either hand-sewn or with two linear staplers (functional end-to-end anastomosis) | NR | *** | ** | * |
£, all 18 patients were diagnosed with acute appendicitis preoperatively. RCS, retrospective cohort study; NR, not reported.
The articles included in the systematic review and pooled-analysis were published in China between 2008 and 2015. They were all retrospective cohort studies (RCS). In total, 96 patients were allocated to either LA (n=30) and OS (n=66). General characteristics of the patients included in the studies are shown in Table 2.
Table 2
| Author, year | N. of patients, (%) | Age (years), mean ± SD | Sex (male/female) | BMI (kg/m2), mean ± SD | Previous operations | Obstruction duration (days), mean ± SD | Tumor size (cm), mean ± SD | T4 tumors | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | ||||||||
| Li Z, 2015 | 10 (28.6) | 25 (71.4) | 64.5±9.7 | 62.3±10.2 | 6:4 | 14:11 | 22.2±3.4 | 22.3±4.1 | 1 (10) | 3 (12) | 3±1.2 | 3±1.8 | 4±1.7 | 4±1.9 | NR | NR | |||||||
| Li JCM, 2009£ | 6 (33.3) | 12 (66.7) | 52.7±16.4 | 45.2±15.0 | 4:2 | 6:6 | NR | NR | 1 (16.7) | 2 (16.7) | NA | NA | NA | NA | NA | NA | |||||||
| Ng SSM, 2008 | 14 (32.5) | 29 (67.5) | 65.5±10.0 | 70.0±12.5 | 6:8 | 14:15 | 24.1±4.9 | 21.5±2.6 | 3 (21.4) | 3 (10.3) | 3.2±1.4 | 4.2±2.2 | 4.7±2.0 | 6.0±3.0 | 2 (14.3) | 11 (37.9) | |||||||
£, all 18 patients were diagnosed with acute appendicitis preoperatively. NR, not reported; NA, not applicable.
Heterogeneity was found among the included studies with regards to the inclusion and exclusion criteria. The study by Li et al., which did not specify the exclusion criteria, enrolled patients with an intra-operative diagnosis of complicated cecal diverticulitis undergoing emergency right colectomy (18). Conversely, the studies by Li et al. and Ng et al. enrolled patients with both a pre-operative and intra-operative diagnosis of obstructing right colon carcinoma (19,20).
Within the LA group, an extracorporeal ileocolic anastomosis was performed in 100% of cases, either side-to-side or end-to-end, hand-sewn or with two linear staplers (Table 1).
Patients characteristics
Patients undergoing LA and OS did not differ in age (sample size: 96; WMD −0.51; 95% CI: −5.28–4.25; P=0.83; I2=28%), male sex (sample size: 96; OR 1.09; 95% CI: 0.46–2.60; P=0.85; I2=0%), BMI (sample size: 78; WMD 1.21; 95% CI: −0.70–3.11; P=0.21; I2=48%), previous operations (sample size: 96; OR 1.43; 95% CI: 0.43–4.82; P=0.56; I2=0%), obstruction duration (sample size: 78; SMD −0.28; 95% CI: −0.76–0.21; P=0.26; I2=0%) and tumor size (sample size: 78; SMD −0.26; 95% CI: −0.75–0.22; P=0.29; I2=0%). Finally, only the study by Ng et al. reported any information concerning the rate of T4 tumors between the two groups. Therefore, we had insufficient data to perform a pooled analysis on this baseline characteristic (19).
Clinical outcomes
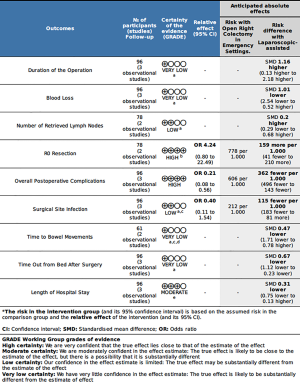
Results of the meta-analyses of clinical outcomes are reported in Table 3 and Figure 2. Forrest plots of clinical outcomes are shown in Figures 3-5. LA was associated with a longer duration of the operation compared to OS (sample size: 96; SMD 1.16; 95% CI: 0.13–2.18; P=0.03; I2=77%). Overall, LA and OS showed equivalent results in terms of mean estimated intra-operative blood loss (sample size: 96; SMD −1.01; 95% CI: −2.54–0.52; P=0.19; I2=89%), mean number of retrieved lymph nodes (sample size: 78; SMD 0.20; 95% CI: −0.29–0.68; P=0.42; I2=18%) and rate of R0 resections (Table 3, no meta-analysis was performed).
Table 3
| Author, year | Duration of operation (min), mean SD | Blood loss (mL), mean SD | Conversion to laparotomy, N. (%) | Number of retrieved lymph nodes, mean SD | R0 resection, N. (%) | Postoperative mortality, N. (%) | Overall postoperative complication, N. (%) | Anastomotic leakage, N. (%) | Surgical site infection, N. (%) | Time to flatus (days), mean SD | Time to bowel movements (days), mean SD | Time out from bed after surgery (days), mean SD | Length of hospital stay (days), mean SD | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | Lap | Open | |||||||||||||
| Li Z, 2015 | 186.518.4 | 14220.8 | 3015.2 | 9029.4 | – | NA | 15.35.6 | 166.3 | 10 (100) | 25 (100) | – | – | 2 (20) | 9 (36) | – | 1 (4) | 1 (10) | 3 (12) | 51.2 | 51.8 | NR | NR | 2.50.8 | 3.20.9 | 72.5 | 93.6 | ||||||||||||
| Li JCM, 2009 | 171.220.2 | 163.753.4 | 7054.8 | 167.595.2 | 7 (53.8) | NA | NA | NA | NR | NR | – | – | 2 (33.3) | 9 (75) | – | – | 2 (33.3) | 6 (50) | NR | NR | 3.70.6 | 5.21.4 | 3.71.4 | 4.71.7 | 7.01.1 | 9.02.9 | ||||||||||||
| Ng SSM, 2008 | 207.770.4 | 14546.2 | 135144.3 | 100175 | – | NA | 19.57.8 | 1511 | 12 (85.7) | 17 (58.6) | 1 (7.1) | 3 (10.3) | 4 (28.6) | 22 (75.9) | – | – | - | 5 (17.2) | NR | NR | 5.21.4 | 5.02.2 | 51.7 | 61.5 | 9.53.4 | 98.5 | ||||||||||||
£, all 18 patients were diagnosed with acute appendicitis preoperatively. NR, not reported; NA, not applicable.
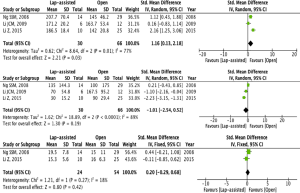

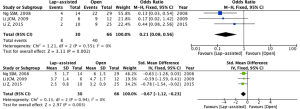
Meta-analyses of postoperative outcomes showed equivalent results between the two groups in terms of surgical site infection (SSI) (sample size: 96; OR 0.40; 95% CI: 0.11–1.54; P=0.18; I2=0%), time to bowel movements (sample size: 96; SMD −0.47; 95% CI: −1.71–0.78; P=0.46; I2=75%), and length of hospital stay (sample size: 96; SMD −0.31; 95% CI: −0.75–0.13; P=0.16; I2=24%). Conversely, LA was associated with a lower rate of postoperative complications compared to OS (sample size: 96; OR 0.21; 95% CI: 0.08–0.56; P=0.002; I2=0%), and resulted in shorter mean time out from bed after surgery (sample size: 96; SMD −0.67; 95% CI: −1.12–0.23; P=0.003; I2=0%).
Quality of evidence and risk of bias assessment
The overall quality of evidence according to the GRADE criteria, was very low for blood loss, duration of the operation, time to bowel movements and time out from bed after surgery. It was low for surgical site infection and number of retrieved lymph nodes, and moderate for length of hospital stay. Conversely, certainty of the evidence for overall postoperative complication and R0 resection rates had a high quality of evidence (Figure 2).
The risk of bias of the three included n-RCTs was assessed using the items suggested by the Newcastle–Ottawa quality assessment tool (14). According to this scale, the maximum quality score could be nine points, representing the highest methodological quality. Two studies achieved seven stars, and one study achieved six stars (18-20). The follow-up length was unclear in all included studies (Table 1).
Discussion
Between 10% and 30% of patients with colorectal cancer have complete or partial intestinal obstruction at diagnosis, and approximately 40% of these patients are diagnosed with obstructing tumors found in the right side of the colon, proximal to the splenic flexure (21-23).
Minimally invasive colectomy has been increasingly implemented to treat colonic disease, including colorectal cancer. Laparoscopic and robotic-assisted techniques are associated with a faster return to normal daily activity, shorter length of hospital stay, less pain, reduced ileus and lower rates of postoperative surgical and respiratory complications and mortality as compared to the traditional open technique (24,25).
The 2016 English National Bowel Cancer Audit reported that postoperative morbidity and mortality after emergency colorectal cancer resection is significantly higher than those following elective surgery (26).
Despite that, and although the role of laparoscopic resections for obstructing colorectal cancer is still controversial, also in emergency setting the use of laparoscopy in colorectal resection for cancer has been associated with a shorter length of hospital stay and decreased postoperative complications and mortality (27).
The increased risk of postoperative complications due to the high-risk patient profile, the electrolyte imbalance and dehydration associated with bowel obstruction and, above all, the technical challenges due to the insufficient working space caused by the distended and vulnerable bowel loops, discouraged surgeons to perform laparoscopic right colectomy in emergency scenarios.
For these reasons, some authors have suggested the adoption of SEMS for right-sided colonic obstruction due to carcinoma before laparoscopic colectomy in order to recover general conditions, facilitate bowel decompression and allow one-stage surgical resections (28,29).
It is generally recognized that for obstructing right-sided colon cancer, right colectomy with primary anastomosis should be performed as treatment of choice (30,31).
Results from recent non-randomized comparative studies and case series on short-term outcomes suggested that laparoscopy is also safe and feasible as a primary approach in case of obstructing right-sided colon cancer (19,20). However, these are single-center analyses limited by small cohorts of patients, and tend to be performed at hospitals where surgeons have relatively high volumes of laparoscopic colorectal resections. The results of these studies may therefore present a lack of generalizability to other low volume hospitals that face with emergency colorectal procedures in the daily surgical practice.
Emergency colectomies for obstructive colorectal cancer are associated with increased mortality and morbidity rates, especially in the elderly and frail patients.
Recent reports from multicenter national cohort studies investigating the status of laparoscopy for patients presenting at the emergency department with acute abdomen in Italy showed that only a small percentage of patients underwent laparoscopy for large bowel resection (32-34). In the same way, results from a recently published systematic review demonstrated that in developed countries less than 17% of emergency colorectal resections for any cause and less than 5% for tumor are performed by laparoscopy (35). So that, despite laparoscopic colorectal surgery could achieve equivalent oncological outcomes compared with OS, and it shows potential advantages such as less blood loss, less pain, faster postoperative recovery and less postoperative complications, its use in emergency is not widespread.
The key to successfully performing laparoscopic right colectomy in emergency for obstructing colorectal cancer or perforated diverticular disease is to provide enough intra-abdominal space for the laparoscopic intervention. SEMS placement for colorectal obstruction has been generally adopted for left-sided colon cancer with a technical success rate >90% (36,37). However, SEMS placement for right-sided obstructing colon cancer can be challenging because of poor site accessibility. Yao et al. published a series of 81 proximal colonic obstruction patients treated by SEMS placement with a success rate >96%. In the same study, 88.9% of the patients subsequently received 1-stage surgical resection, with low morbidity and mortality rates (38).
Recently, the study by Arai et al. demonstrated the safety and feasibility of SEMS insertion followed by laparoscopic resection as a minimally-invasive approach for the management of acute right-sided colonic obstruction due to cancer. As higher morbidity and mortality rates for urgent surgery than for elective surgery have been reported for obstructing right-sided colorectal cancer, the therapeutic option of SEMS placement combined with 1-stage laparoscopic resection should be taken into account as an alternative procedure to urgent surgery (28).
Our systematic review and meta-analysis demonstrated that LA right colectomy resulted in shorter mean time out from bed after surgery as compared to the open technique. Surprisingly, the two techniques showed equivalent results in terms of mean estimated intra-operative blood loss, surgical site infection, time to bowel movements and length of hospital stay.
The reasons for these outcomes must be sought in several characteristics of the studies included in the pooled analysis.
The restoration of bowel continuity after laparoscopic right colectomy can be performed in either an extracorporeal or intracorporeal manner. Despite side-to-side ileocolic anastomosis is the most frequently adopted technique by laparoscopic approach as well as by OS, there is still debate about how to perform the anastomosis following right colectomy.
All three studies included in our meta-analysis reported the routine adoption of an extracorporeal ileocolic anastomosis. Extracorporeal anastomosis has been related to longer postoperative hospital stay, prolonged ileus, and higher risk of surgical site infection and incisional hernia. On the other hand, although intracorporeal anastomosis is associated with better short-term outcomes (which are mainly related to lower bowel manipulation and stretching, such as shorter extraction site incisions, earlier bowel recovery, fewer complications, and lower rates of conversion, anastomotic leakage, surgical site infection, and incisional hernia), it is still considered a demanding procedure (39-41).
Recently, a large international prospective study analyzed the outcomes of 3288 patients undergoing elective colorectal resection. The results showed that 301 patients included in the analysis (9.2%) were discharged before the return of bowel function and there were no statistically significant differences in rates of readmission between patients discharged before and after return of bowel function. Moreover, incidence of postoperative complications was also similar in patients discharged before versus after return of bowel function (42).
Although the mean length of hospital stay for patients with obstructing colorectal cancer approached with laparoscopy can be predefined in different ward protocols at each study center, it may possibly be shortened in further daily clinical practice as this practice appears to be safe in appropriately selected patients.
Although limited by the high risk of imprecision due to the small sample size, superiority in terms of overall morbidity of the LA approach compared to the open technique, as reported in our meta-analysis, confirms the aspects of safety of minimally invasive emergency right colectomy.
On the other hand, equivalency in terms of mean number of harvested lymph nodes and rate of R0 resections confirms the aspects of oncological adequacy of LA right colectomy.
As reported by Athanasiou et al., laparoscopic right colectomy has a lower wound-infection rate compared with the traditional open approach, and shorter length of hospital stay (43).
Moreover, in the systematic review and meta-analysis by Cirocchi et al. investigating the outcomes of laparoscopic versus open right colectomy for obstructing colon cancer, blood loss, time to mobilization after surgery, postoperative complication rate and length of hospital stay were significantly shorter in the laparoscopic group, while the difference in the operative time was in favor of the open group (44).
In our study, the LA technique was associated with a statistically significant lower rate of postoperative complications compared to the traditional open technique.
Clearly, laparoscopic approach cannot be applied to every patient who requires emergency right colectomy. Patients with diffuse peritonitis from colonic perforation, extensive adhesions, high-grade obstruction, large cancers, patients with a grossly distended abdomen and dilated bowel loops, and those with severe intra-abdominal sepsis are generally not good candidates for laparoscopic colorectal resections because of poor visibility and a high risk of bowel injury. Conversely, patients with a small stenotic tumor and mild dilatation of small bowel loops are most suitable for the laparoscopic approach.
As the therapeutic approach to colorectal cancer is multidisciplinary, one of the most important outcomes of minimally invasive oncologic colorectal resections is the lower proportion of patients who have a delay in receiving adjuvant chemotherapy compared to patients treated with OS. Although our systematic review and meta-analysis showed no significant difference between the AL and OS groups in terms of hospital stay, the lower risk of postoperative complications can be related to improved recovery following surgery and can reduce the delay in initiating adjuvant chemotherapy, ultimately leading to improved progression-free survival rates for patients undergoing laparoscopic colectomy compared to open resection.
Furthermore, the reduction in time out of bed after surgery and the lower rate of postoperative complication following minimally invasive colorectal resection result in overall better resource utilization. As demonstrated by Keller et al., outcomes following laparoscopic colectomy in emergency setting resulted in reduced length of hospitalization, lower complication rates, and lower costs (45).
Key limitations of the present meta-analysis were the small number of comparative studies that have reported on this field of research, as well as the absence of RCTs published to date.
The extended period of time through which the enrolled studies were published can represent a further source of selection bias.
Another potential limitation of the present study derives from the scarcity of data coming from patients submitted to laparoscopic right colectomy with intracorporeal ileocolic anastomosis. This issue may affect the clinical results concerning the potential role of laparoscopic right colectomy in the contemporary era, where intracorporeal anastomosis is now incorporated into clinical practice in many settings (46-48). In a recent multicenter prospective study, a side-to-side isoperistaltic stapled intracorporeal anastomosis with hand-sewn enterotomy closure was the most frequently adopted technique to perform ileocolic anastomosis after any indications for elective laparoscopic right colectomy (40).
Moreover, according to the GRADE criteria, the overall quality of evidence for each of the clinical outcome measures was very low to moderate, and statistical heterogeneity was high for important outcomes, such as intraoperative blood loss, operative time and time to bowel movements after surgery. Thus, all the results that advocate any type of superiority of the laparoscopic technique over the traditional open technique should be interpreted with extreme caution. This, together with the lack of cost-effectiveness results, and the paucity of data available to us today on long-term oncological outcomes do not allow for definitive conclusions to be drawn.
Conclusions
Although limited by the risk of imprecision due to the small sample size and the low level of evidence of the reported outcomes, this systematic review and meta-analysis demonstrated that LA right colectomy has the same safety profiles compared to the traditional open technique, as shown by equivalent results in terms of mean estimated intra-operative blood loss, surgical site infection, length of hospital stay, and mean number of retrieved lymph nodes. Possible advantages of laparoscopy in right colectomy are related to lower rates of postoperative complications and shorter mean time out from bed after surgery.
Multicentric, well-designed and adequately powered clinical trials comparing laparoscopic and open right colectomy in emergency settings are still required to validate these preliminary observations.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Milone and Ugo Elmore) for the series “Right Colectomy 2.0” published in Annals of Translational Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/ales-20-57
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-57). SDS serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Apr 2018–Mar 2020. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Podda M, Saba A, Porru F, et al. Systematic review with meta-analysis of studies comparing single-incision laparoscopic colectomy and multiport laparoscopic colectomy. Surg Endosc 2016;30:4697-720. [Crossref] [PubMed]
- Pellino G, Podda M, Wheeler J, et al. Laparoscopy and resection with primary anastomosis for perforated diverticulitis: challenging old dogmas. Updates Surg 2020;72:21-8. [Crossref] [PubMed]
- Odermatt M, Miskovic D, Siddiqi N, et al. Short- and long-term outcomes after laparoscopic versus open emergency resection for colon cancer: an observational propensity score-matched study. World J Surg 2013;37:2458-67. [Crossref] [PubMed]
- Delaney CP, Marcello PW, Sonoda T, et al. Gastrointestinal recovery after laparoscopic colectomy: results of a prospective, observational, multicenter study. Surg Endosc 2010;24:653-61. [Crossref] [PubMed]
- Leung KL, Meng WC, Lee JF, et al. Laparoscopic-assisted resection of right-sided colonic carcinoma: a case-control study. J Surg Oncol 1999;71:97-100. [Crossref] [PubMed]
- Di Saverio S, Segalini E, Birindelli A, et al. Laparoscopic extended right and transverse colectomy with completely intracorporeal ileo-descending anastomosis for obstructing colon carcinoma - a video vignette. Colorectal Dis 2018;20:80-2. [Crossref] [PubMed]
- Zerey M, Hawver LM, Awad Z, et al. SAGES evidence-based guidelines for the laparoscopic resection of curable colon and rectal cancer. Surg Endosc 2013;27:1-10. [Crossref] [PubMed]
- Martinez-Santos C, Lobato RF, Fradejas JM, et al. Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum 2002;45:401-6. [Crossref] [PubMed]
- Rho SY, Bae SU, Baek SJ, et al. Feasibility and safety of laparoscopic resection following stent insertion for obstructing left-sided colon cancer. J Korean Surg Soc 2013;85:290-5. [Crossref] [PubMed]
- Li JC, Hon SS, Ng SS, et al. Emergency laparoscopic-assisted right hemicolectomy: can we achieve outcomes similar to elective operation? J Laparoendosc Adv Surg Tech A 2011;21:701-4. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100 [Crossref] [PubMed]
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [Crossref] [PubMed]
- Higgins JPT, Green S. editors. Cochrane handbook for systematic reviews of interventions version 5.3.5. The cochrane collaboration, 2019. Available from: www.handbook.cochrane.org. Accessed February 2020.
- Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401-6. [Crossref] [PubMed]
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses, 2012. Available online: http://wwwohrica/programs/clinical_epidemiology/oxfordasp. Accessed February 2020.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [Crossref] [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Li JC, Ng SS, Lee JF, et al. Emergency laparoscopic-assisted versus open right hemicolectomy for complicated cecal diverticulitis: a comparative study. J Laparoendosc Adv Surg Tech A 2009;19:479-83. [Crossref] [PubMed]
- Ng SS, Lee JF, Yiu RY, et al. Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg 2008;32:454-8. [Crossref] [PubMed]
- Li Z, Li D, Jie Z, et al. Comparative Study on Therapeutic Efficacy Between Hand-Assisted Laparoscopic Surgery and Conventional Laparotomy for Acute Obstructive Right-Sided Colon Cancer. J Laparoendosc Adv Surg Tech A 2015;25:548-54. [Crossref] [PubMed]
- Carraro PG, Segala M, Cesana BM, et al. Obstructing colonic cancer: failure and survival patterns over a ten-year follow-up after one-stage curative surgery. Dis Colon Rectum 2001;44:243-50. [Crossref] [PubMed]
- Deans GT, Patterson CC, Parks TG, et al. Colorectal carcinoma: importance of clinical and pathological factors in survival. Ann R Coll Surg Engl 1994;76:59-64. [PubMed]
- Ohman U. Prognosis in patients with obstructing colorectal carcinoma. Am J Surg 1982;143:742-7. [Crossref] [PubMed]
- Papageorge CM, Zhao Q, Foley EF, et al. Short-term outcomes of minimally invasive versus open colectomy for colon cancer. J Surg Res 2016;204:83-93. [Crossref] [PubMed]
- Park JS, Kang H, Park SY, et al. Long-term oncologic after robotic versus laparoscopic right colectomy: a prospective randomized study. Surg Endosc 2019;33:2975-81. [Crossref] [PubMed]
- English National Bowel Cancer Audit Report 2016 [published 16 December 2016, accessed 14 february 2020]. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/national-bowel-cancer-audit/national-bowel-cancer-audit-report-2016.
- Vallance AE, Keller DS, Hill J, et al. Role of Emergency Laparoscopic Colectomy for Colorectal Cancer: A Population-based Study in England. Ann Surg 2019;270:172-9. [Crossref] [PubMed]
- Arai T, Sakon M, Fujii T, et al. Efficacy of self-expanding metallic stent for right-sided colonic obstruction due to carcinoma before 1-stage laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 2014;24:537-41. [PubMed]
- Lee GJ, Kim HJ, Baek JH, et al. Comparison of short-term outcomes after elective surgery following endoscopic stent insertion and emergency surgery for obstructive colorectal cancer. Int J Surg 2013;11:442-6. [Crossref] [PubMed]
- Ormando VM, Palma R, Fugazza A, et al. Colonic stents for malignant bowel obstruction: current status and future prospects. Expert Rev Med Devices 2019;16:1053-61. [Crossref] [PubMed]
- De Salvo GL, Gava C, Pucciarelli S, et al. Curative surgery for obstruction from primary left colorectal carcinoma: primary or staged resection? Cochrane Database Syst Rev 2004;CD002101 [PubMed]
- Agresta F, Campanile FC, Podda M, et al. Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc 2017;31:1785-95. [Crossref] [PubMed]
- Costa G, Fransvea P, Podda M, et al. The use of emergency laparoscopy for acute abdomen in the elderly: the FRAILESEL Italian Multicenter Prospective Cohort Study. Updates Surg 2020;72:513-25. [Crossref] [PubMed]
- Antoniou SA, Antoniou GA, Koch OO, et al. Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc 2015;29:322-33. [Crossref] [PubMed]
- Harji DP, Griffiths B, Burke D, et al. Systematic review of emergency laparoscopic colorectal resection. Br J Surg 2014;101:e126-33. [Crossref] [PubMed]
- Meisner S, González-Huix F, Vandervoort JG, et al. Self-expandable metal stents for relieving malignant colorectal obstruction: short-term safety and efficacy within 30 days of stent procedure in 447 patients. Gastrointest Endosc 2011;74:876-84. [Crossref] [PubMed]
- Meisner S, González-Huix F, Vandervoort JG, et al. Self-Expanding Metal Stenting for Palliation of Patients with Malignant Colonic Obstruction: Effectiveness and Efficacy on 255 Patients with 12-Month’s Follow-up. Gastroenterol Res Pract 2012;2012:296347 [Crossref] [PubMed]
- Yao LQ, Zhong YS, Xu MD, et al. Self-expanding metallic stents drainage for acute proximal colon obstruction. World J Gastroenterol 2011;17:3342-6. [Crossref] [PubMed]
- Emile SH, Elfeki H, Shalaby M, et al. Intracorporeal versus extracorporeal anastomosis in minimally invasive right colectomy: an updated systematic review and meta-analysis. Tech Coloproctol 2019;23:1023-35. [Crossref] [PubMed]
- Anania G, Agresta F, Artioli E, et al. Laparoscopic right hemicolectomy: the SICE (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie) network prospective trial on 1225 cases comparing intra corporeal versus extra corporeal ileo-colic side-to-side anastomosis. Surg Endosc 2019; [Epub ahead of print]. [PubMed]
- van Oostendorp S, Elfrink A, Borstlap W, et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 2017;31:64-77. [Crossref] [PubMed]
- EuroSurg Collaborative. Safety of hospital discharge before return of bowel function after elective colorectal surgery. Br J Surg 2020;107:552-9. [Crossref] [PubMed]
- Athanasiou CD, Markides GA, Kotb A, et al. Open compared with laparoscopic complete mesocolic excision with central lymphadenectomy for colon cancer: a systematic review and meta-analysis. Colorectal Dis 2016;18:O224-35. [Crossref] [PubMed]
- Cirocchi R, Campanile CF, Di Saverio S, et al. Laparoscopic versus open colectomy for obstructing right colon cancer: A systematic review and meta-analysis. J Visc Surg 2017;154:387-99. [Crossref] [PubMed]
- Keller DS, Pedraza R, Flores-Gonzalez JR, et al. The current status of emergent laparoscopic colectomy: a population-based study of clinical and financial outcomes. Surg Endosc 2016;30:3321-6. [Crossref] [PubMed]
- Aiolfi A, Bona D, Guerrazzi G, et al. Intracorporeal Versus Extracorporeal Anastomosis in Laparoscopic Right Colectomy: An Updated Systematic Review and Cumulative Meta-Analysis. J Laparoendosc Adv Surg Tech A 2020;30:402-2. [Crossref] [PubMed]
- Bollo J, Turrado V, Rabal A, et al. Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg 2020;107:364-372. [Crossref] [PubMed]
- Cleary RK, Kassir A, Johnson CS, et al. Intracorporeal versus extracorporeal anastomosis for minimally invasive right colectomy: A multi-center propensity score-matched comparison of outcomes. PLoS One 2018;13:e0206277 [Crossref] [PubMed]
Cite this article as: Podda M, Pisanu A, Segalini E, Birindelli A, Pellino G, Marino MV, Gomes CA, Kumar J, Di Saverio S. Emergency right colectomy: is there a role for minimally invasive surgery?—A systematic review and meta-analysis of short-term clinical outcomes. Ann Laparosc Endosc Surg 2020;5:40.