Which hiatal hernia’s need to be fixed? Large, small or none?
Introduction
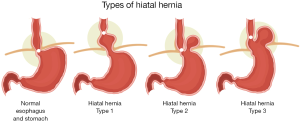
A hiatal hernia refers to herniation of intra-abdominal contents through the esophageal hiatus of the diaphragm. Theories on the etiology of hiatal hernia range from esophageal shortening due to progressive acid exposure, weakness in the crural diaphragm due to aging, and longstanding increased intra-abdominal pressure from obesity or chronic lifting and straining. The prevalence of hiatal hernia varies in the literature from 15–20% in western populations (1-3). Hiatal hernias can be classified by the position of the gastroesophageal junction (GEJ) and the extent of stomach that is herniated. A type I hiatal hernia occurs when there is intermittent migration of the GEJ into the mediastinum. These are often colloquially called “sliding hiatal hernias”. Type I hiatal hernias make up more than 95% of hiatal hernias (Figure 1) (4). They are most often asymptomatic. When symptomatic, patients will commonly present with symptoms of gastroesophageal reflux disease (GERD) (5).
Type II-IV hiatal hernias are commonly grouped together and called para-esophageal hernias (PEH) (Figure 1). They are estimated to make up only 5–10% of all diagnosed hiatal hernias (6). Type II hiatal hernias occur when the fundus of the stomach herniates through the esophageal hiatus. The GEJ remains normally positioned below the diaphragm. A type III hiatal hernia is a combination of a type I and type II hiatal hernia in that both the GEJ and fundus of the stomach herniate through the esophageal hiatus. A type IV hiatal hernia occurs when there is displacement of organs other than the stomach into the mediastinum. Type II–IV hernias can be asymptomatic or symptomatic. It has been estimated that roughly 50% of patients with type II-IV hiatal hernias are asymptomatic (7).
When symptomatic, symptoms can be linked to gastroesophageal reflux and its complications, mechanical obstruction due to partial volvulus, or pressure-related symptoms caused by the herniation of organs into the posterior mediastinum. These can include regurgitation, dysphagia, early satiety, chest pain, and shortness of breath. Large paraesophageal hernias (PEHs) predispose to gastric volvulus with potential necrosis of the stomach secondary to impaired blood flow in gastric vessels (6). The potential life-threatening nature of this complication underscores the importance of determining which patients require surgery.
The surgical management of hiatal hernia has evolved from open (transthoracic, transabdominal) procedures to laparoscopic procedures. Laparoscopy is now favored for its reduced morbidity, shorter hospital stay, and decreased pain medication requirements (8). Regardless of the approach, the aim of surgery is reduction of the hernia sac and tension-free closure of the hiatal defect, paired with an anti-reflux procedure.
Surgery is recommended for all acute symptomatic presentations of PEHs (obstruction or incarceration/strangulation). Management in the non-acute and asymptomatic setting is less clear. Type I hiatal hernias are not typically surgically repaired if they are asymptomatic, given their low overall morbidity. The management of type II-IV hiatal hernia is less clear. Influential studies published more than 40 years ago led to recommendations that surgeons prophylactically repair all PEHs in order to avoid the potential development of volvulus and/or gastric ischemia. These studies estimated a 30% or greater risk of developing acute symptoms and complications in “observation only” patients (9,10). In recent years, however, some studies have found that the risk of catastrophic complications is much lower than these initial estimates. This has reignited the debate on the need to operate on asymptomatic or minimally symptomatic paraesophageal hernias (11).
Few studies have looked at the natural history of paraesophageal hernias without surgical intervention, making it difficult to assess the risks of watchful waiting. In order to fully identify the benefit of surgical intervention, it is necessary to assess outcomes following surgery with regards to symptomology, quality of life, and rates of hernia recurrence. The question of whether a patient should receive surgery is further complicated by the patient’s age and medical comorbidities. It is also essential to identify special populations of patients that might have consistently worse outcomes so that they can be counseled on risks prior to surgery. We attempt to address these topics in our review of which hiatal hernias necessitate an operation.
In order to answer the question “which hiatal hernias need fixing,” a literature search was performed using the PubMed database. Search terms included: hiatal hernia, paraesophageal hernia, diaphragmatic hernia, surgery. Abstracts were reviewed for relevancy to the topic. Studies were only included if they were published within the last 20 years, were in English, and the full text was available. In addition to the database search, references from each paper included were searched for eligible studies.
Management of type I hiatal hernia
Asymptomatic
Although there are rare reports of type I hiatal hernias leading to complications, official guidelines recommend that asymptomatic type I hiatal hernias should be observed only (12). This is because the vast majority of type I hiatal hernias do not progress to the need for emergent operation without first becoming symptomatic. It stands to reason that if such patients have regular follow-up, they will have an elective repair before they develop indications for emergency surgery. There remains of course, the unresolved question of the natural history of type I hiatal hernias and whether they eventually become type III or IV hernias.
O’Donnell et al. observed the incidence of type I-IV hiatal hernias in active component members of the US. Army, Navy, Air Force, and Marine Corps who served between January 2005 and December 2014 (2). Individuals were identified using records of inpatient and outpatient health care documented in the Defense Medical Surveillance System. In total, 27,276 individuals were diagnosed with a hiatal hernia during this time period, with an overall incidence of 19.7 per 10,000 person-years. Of the 27,276 service members with a diagnosis of hiatal hernia, only 235 (0.86%). had any surgical repair during the surveillance period, and only 47 (0.17%) cases were emergent. This study concluded that an overwhelming majority of diagnosed cases of diaphragmatic hiatal hernia never require surgery. The true incidence of hiatal hernia in this population was likely higher, given the fact that there was no routine screening in this study. Unfortunately, the study did not report the distribution of different hiatal hernia types in emergent and non-emergent surgeries.
Further research has examined the natural history of specifically type I hiatal hernias. A single institution retrospective review conducted by Ahmed et al. in 2018 evaluated the natural history of type I hiatal hernias less than 5 cm (13). Patients were diagnosed following endoscopy performed as part of the workup for GERD, dysphagia, chest pain, abdominal pain, or follow-up of Barrett’s esophagus. All living patients were sent a questionnaire regarding their GERD-related symptoms. Though many patients had persistent symptoms at 10 years of follow-up, researchers discovered that only 1.5% of patients ultimately underwent elective surgery for their hiatal hernia. Two patients received an operation due to the development of refractory GERD. One patient had progressive enlargement of the hiatal hernia and underwent elective repair secondary to the development of iron deficiency anemia. No emergency surgeries were documented over the 10-year study period. Given the low rate of progression to surgery, authors concluded that observation of asymptomatic small to medium sized type I (roman numeral) hernias is safe.
Symptomatic
There has been extensive physiologic research observing the association between sliding hiatal hernia and gastroesophageal reflux. Scheffer et al. performed high resolution manometry and pH studies on 20 patients with a history of GERD and 20 normal volunteers during and after a standardized meal (14). They also compared the volume of the intraabdominal stomach using ultrasound. Researchers noted that patients with GERD symptoms had a higher proportion of time in the fasting state where they had two definitive high-pressure zones on manometry consistent with the profile of a hiatal hernia (32.9±4.9 min h) (53.2%) compared to controls (8.7±3.3 min h) (14.5%) (P<0.001). Researchers also observed that when the stomach was herniated, there was a higher rate of reflux recorded on pH testing (2.1±0.6 and 3.8±0.9 per hour; P<0.05).
Furthermore, there is evidence that elective repair of type I hiatal hernia is associated with lower rates of intra and post-operative complications as well as decreased complication-related reoperation rates compared to PEHs (15). The causal association between GERD and type I hiatal hernia, plus the relatively low complication rates provide compelling evidence for elective repair of these symptomatic hernias.
Management of type II-IV PEH
Symptomatic
An ideal research study to compare the risks and benefits of repair versus observation of symptomatic PEH would be a randomized controlled trial. However, this data is lacking given that symptomatic hernias are already routinely repaired by most surgeons. Sihvo et al. conducted one of the few studies that addresses disease-specific mortality of symptomatic PEHs (11). Researchers identified 563 patients that underwent surgical treatment and 67 patients that underwent in-hospital conservative management of PEHs from 1987–2001. They found a 2.7% perioperative mortality rate in patients who underwent surgical treatment. In patients that were hospitalized for PEH but ultimately treated without surgery, the mortality rate was 16.4%. This is likely an overestimate of mortality given that many patients with PEH may have never been hospitalized and thus would not be captured in the “watchful waiting” group of this study. Upon reviewing records for the patients that died during conservative treatment, the authors estimated that 13% of the deaths could have been prevented with surgical intervention. The results of this study highlight the poor outcomes of watchful waiting for symptomatic PEH.
In addition to this mortality benefit, there are several well-documented symptomatic benefits to repair of PEH. Patients often report relief of their GERD symptoms: dysphagia, bloating, regurgitation and early satiety (16-18).
Additional consideration should also be given to improvements in cardiac and pulmonary function. Carrott et al. conducted a retrospective review comparing pre and post-operative pulmonary function tests (PFTs) in patients who underwent repair of either symptomatic or asymptomatic PEHs (19). The surgery group demonstrated a statistically significant improvement in PFT values (P<0.01). Furthermore, multivariate regression models demonstrated a correlation between the degree of PFT improvement and the amount of intrathoracic stomach.
The results of this retrospective study were further corroborated in a recent prospective study of 570 patients conducted by Wirsching et al. (20). They found an improvement in spirometry values in 80% of patients. The degree of improvement after repair was greatest when the percentage of intrathoracic stomach was >75% (P=0.001). Low and Simchuk also found similar improvements in spirometry values (21).
In addition to improvements in respiratory function there is also research demonstrating improvements in cardiac physiology following PEH repair (22). Cardiac MRI performed before and after a meal noted that the size of the PEH increased significantly after eating, and that this increase in size led to a concurrent decrease in left ventricular stroke volume (P=0.012) and ejection fraction (P=0.010). Post-surgical MRI showed significant improvements in left atrial and left ventricular size and EF. Pulmonary function testing was also performed and showed improvements in FEV1 and FVC after surgery. Finally, patient reported cardiorespiratory symptoms improved after surgery compared to pre-operative values (P<0.01). Together, these studies show that the improvement after PEH repair is not limited solely to gastrointestinal and GERD-related pathology.
Outcomes of elective repair
Current surgical techniques for elective PEH repair have documented low postoperative morbidity/mortality and favorable long-term symptomatic outcomes. Targarona et al. reported an 11% morbidity for short-term complications in their study of 46 patients with type II, III, and IV PEH receiving laparoscopic repair +/− mesh reinforcement and Nissen fundoplication (23). Patients were followed for a median of 24 months. This study assessed quality of life using various surveys: Short Form – 36 (SF-36), Glasgow Dyspepsia Severity Score (GDSS), and Gastrointestinal Quality of Life Index (GIQLI). Quality of life according to the GIQLI was similar between the entire cohort and a standard comparison population. This study found a 20% recurrence rate over a median follow-up of 24 months using barium swallow to make the diagnosis. The majority of recurrences were found to be asymptomatic or minimally symptomatic sliding hiatal hernias. There was no significant difference in patient reported quality of life between groups of patients that had recurrence versus those that did not, suggesting that recurrence can be symptomatically inconsequential.
Sorial et al. conducted a retrospective review of all PEH hernia cases over a 7-year period, with specific attention to identifying risk factors for recurrence (24). At a median follow-up time of 6 months, the overall symptomatic recurrence rate was 9.9%. They examined patient demographics, hernia size, technical aspects of the operation, and surgical experience. On multivariate analysis, experience of the operating surgeon was the only factor significantly affecting the rate of recurrence.
Mehta et al. performed a pooled analysis of 20 retrospective studies. They found a pooled 5.3% intraoperative morbidity, and a 12.7% rate of postoperative complications among 1,387 patients undergoing laparoscopic PEH repair. Their analysis found a 16.9% recurrence rate over an adjusted mean follow-up time of 16.5 months. The recurrences were 47% type I sliding hernias, 23% wrap disruption, and 30% true PEH recurrence. The 20 studies included in their analysis had highly variable individual recurrence rates ranging from 0–44%. The authors attribute this variation in part to a heterogeneous definition of recurrence (25). Other studies have found similar favorable results (8,23,26-29).
These studies argue that elective surgery is safe and has favorable symptomatic outcomes. They also argue that risk of recurrence is not minimal but can be symptomatically and clinically inconsequential.
Outcomes of emergency repair
In order to determine the risk versus benefits of elective repair versus emergency surgery, a thorough understanding of the outcomes associated with emergency repair is also necessary. One such study, done by Jassim et al., performed a prospective review using the Nationwide Inpatient Sample (NIS) database between 2006–2008 to study 41,723 patients undergoing PEH repair in the United States (30). Emergent repair was associated with a significantly higher rate of morbidity (33.4% vs. 16.5% elective, P<0.001) and mortality (3.2% vs. 0.37%, P<0.001) than elective repair. These differences, in part, can be explained by differing characteristics between the two groups. Patients undergoing emergent repair were significantly more likely to be older, male, and to have medical comorbidities (alcohol abuse, iron deficiency anemia, electrolyte disorders, renal failure, and weight loss/malnutrition). Patients undergoing emergent repair were also significantly less likely to receive laparoscopic surgery. After controlling for these characteristics using multivariate analysis, emergency repair was associated with higher mortality. These results suggest that non-elective surgery leads to poor outcomes in terms of morbidity and mortality, attributable to increased age and comorbid conditions.
Multiple other studies have shown similar results. Tam et al. used propensity score matching for gender, age, BMI, Charlson Comorbidity Index, tobacco use, pre-operative symptoms, hernia size, hospital, and surgeon differences between elective and emergent patients and found that the odds of post-operative complications and mortality are consistently 2–3 times greater for emergent repair versus elective repair (31).
Ballian et al. found that emergent presentation was associated with significant mortality even after holding other predictive variables constant. They found that individuals undergoing emergency PEH repair were more likely to be male, older than 70, underweight or normal body weight, to have larger hernias, and increased comorbidities (32). In this study, mortality was 1.1% after elective surgery versus 8.0% after non-elective surgery (P<0.01).
Polomsky et al. performed a population-based study of admissions for PEH in the state of New York (9). Fifty-three percent of the PEH hospitalizations in their study were emergent. Interestingly, 66% of these were discharged before any surgical intervention. Emergency admissions had higher mortality (2.7% vs. 1.2%, P<0.001), longer length of stay (7.3d vs. 4.9d, P<0.001), and higher cost ($28,484 vs. $24,069, P<0.001) than elective surgery admissions (9). Emergent presentation had statistical significance associated with mortality, length of stay, and cost in multivariable regression models including age and type of operative intervention.
Other studies have drawn a different conclusion: that the variance in mortality between elective and emergency repair is entirely accounted for by comorbidities. Shea et al. performed a retrospective review of PEH patients at one institution. They compared patients undergoing emergency versus elective PEH repair, using both propensity scores and multivariate logistic regression to control for significant differences in age, sex, body mass index (BMI), American Society of Anesthesiology (ASA) class, tobacco use, and comorbidities such as diabetes, hypertension, chronic obstructive pulmonary disease, hyperlipidemia, coronary artery disease, and GERD. Their study identified a total of 229 patients that underwent PEH repair, with 199 undergoing elective repair (86.9%) and 30 (13.1%) undergoing emergent repair. Emergent cases were more likely to be older individuals with larger and more complex hernias. They were also more likely to have a longer hospital stay (6.63 vs. 2.79 days, P=0.002), more postoperative complications (44.8% vs. 19.4%, P=0.002), and a higher proportion of severe complications. There was no statistically significant difference in readmission rates between the two groups (3.7% vs. 3.5%, P=0.22). These differences in cohorts were no longer significant when comparing propensity matched groups. This suggests that the complications experienced by the emergent group are attributable to their comorbidities and not the emergent nature of their operation.
Augustin et al. used NSQIP data to study 3,598 patients undergoing elective or emergent (5%) PEH repair from 2009–2011. They similarly found that emergent surgery is not associated with mortality after adjusting for comorbidities (33). They found, instead, that frailty and preoperative sepsis increased the odds of mortality and that laparoscopic (versus open) repair and BMI ≥25 (versus BMI <18.5) were significantly protective of mortality.
Many of the above studies have suggested that PEH repair in older patients is associated with greater morbidity and mortality. Poulose et al. specifically examined the elderly patient population (34). They used the 2005 Nationwide Inpatient Sample database to investigate octogenarians receiving elective and non-elective surgery for PEH. Non-elective surgery was performed in 43%. Non-elective patients had higher mortality (16% vs. 2.5%) and length of stay (14.3 vs. 7 days) than their elective counterparts. This mortality is double of that presented in research without octogenarians (32). This study reported a much higher length of stay than other studies, in part because the population consisted only of octogenarians and because this study included all forms of PEH repair while other studies focus on laparoscopic approaches (35). Prolonged length of stay places patients at increased risk of pulmonary complications, UTI, worsening disability, and cognitive impairment in the elderly (36-39).
Together, the weight of evidence suggests that although part of the increased morbidity and mortality of emergency repair is explained by differences in comorbidities, there is also an independent risk associated with emergency repair.
Asymptomatic PEHs: elective repair versus watchful waiting
As the literature indicates, preventing emergency surgery for the individual patient is ideal. However, it is still unclear the best time to intervene electively. Modern outcomes for emergency surgery have improved, with some studies reporting mortality rates as low as 0–2% (27,30). With this improvement came a revisiting of the original question. Which types of hiatal hernias in which situations can effectively be observed? What is the best management strategy to apply to the asymptomatic PEH population as a whole?
Modern population-based studies examining the disease progression of PEHs are largely lacking. In lieu of sufficient epidemiological comparisons of watchful waiting and elective paraesophageal hiatal hernia repair, research teams have turned to computer modeling to answer this question. Stylopoulos et al. investigated whether the risks of undergoing elective surgery to repair type II and type III hiatal hernias outweighed the risks of eventual progression necessitating operation, or eventual further progression necessitating emergency surgery. The research team created a Monte Carlo simulation based on a review of 1,035 patients obtained from healthcare cost and utilization project data in 2002 (40). The primary outcome was quality adjusted life expectancy (QALE) in the two groups. At all time points, watchful waiting led to a greater overall increase in QALE then elective surgery. The benefit of watchful waiting was more pronounced as age at presentation increased. This is because researchers found that the risk of progression to severe symptoms decreased as the age of the patient increased. Furthermore, a sensitivity analysis was conducted. The model was only sensitive to alterations in the mortality rates of elective and emergency operations. Given the large amount of data utilized to create the Monte Carlo simulation and the results of the sensitivity analysis, it seemed that the risks of elective PEH repair outweighed the benefits.
Sixteen years later, this study was repeated by Morrow et al. using updated outcome numbers including costs (41). A Markov decision model was developed to again compare watchful waiting and elective hernia repair for minimally symptomatic PEH. The model included the potential states of immediate postoperative state, PEH recurrence, symptomatic versus asymptomatic after surgery, and death. The model was constructed based on aggregation of outcomes data from a systematic review of the literature. This was therefore a more comprehensive model than the previous study. Elective laparoscopic hernia repair was overall more expensive. The average cost for a patient who received elective surgery was $11,771. For the watchful waiting arm, it was only $2,207. Patients who received elective hernia repair had an average of 1.3 additional quality adjusted life years (14.3 vs. 13.0). The cost was therefore $7,303.00 per quality adjusted life year. The authors note that most patients when surveyed believe that one quality adjusted life year should be worth $50,000 to $100,000. As such, the authors conclude that cost of initial elective surgery justified the overall improvement in quality of life.
One of the major reasons why the 2018 study differed so strikingly from the 2002 study was that mortality of elective PEH repair has continued to decrease. The 2002 study found that the mortality associated with elective repair was around 1%, which was the same as mortality for emergency surgery in the data they used. This repeat study in 2018 used mortality of around 5% for emergency surgery and 0.65% for elective surgery. Thus, just as the sensitivity analysis in the original 2002 study predicted that changes in mortality could affect the results of the study, these new statistics altered the best decision course to again favor elective repair.
Given this evidence, it appeared that routine operative intervention for asymptomatic PEHs would again be recommended. However, an additional simulation study published by Jung et al. later in 2018 drew different conclusions (42). A Markov model was created based on data collected from a systematic review of studies on type 2 and 3 hiatal hernias. Researchers discovered a difference in QALE of 5 months favoring watchful waiting over elective hernia repair. Eighty-four percent of their simulations showed a more favorable outcome if patients were initially assigned to watchful waiting. This effect did not change in a sensitivity analysis that increased the maximum age a patient could undergo surgery to 95 years. The same analysis also decreased the amount of years the patient was at risk for recurrence to 5 years and changed the type of closure method from mesh repair to suture only.
It is surprising that two studies with very similar methodology yielded such strikingly different outcomes. Although these studies are simulations and cannot account for every variable as in a randomized controlled trial, they used the same current body of literature and statistical methodology yet arrived at very different conclusions. This appears to be due to differences in risk percentages used in the simulations. The Jung et al. study (which favored watchful waiting) set the risk of postoperative complication after emergency hiatal hernia repair to be 11.9%. In the study by Morrow et al., the risk was set at 21%. A lower emergency complication rate decreases the risk of needing emergency surgery, favoring watchful waiting. There were also important differences in the proportion of patients who progressed to a symptomatic hernia (7.4% watchful waiting study, 13.87% elective repair study). Finally, the Jung et al. watchful waiting study allowed for the possibility of a second elective hernia repair, whereas the study favoring elective repair did not. If there was a potential for multiple repairs, this would negatively impact quality of life compared to a model which didn’t have this potential factored in.
All told, these studies highlight how interpretation of the literature and how changing the input data can dramatically affect the results of a Markov model. Even a sensitivity analysis will miss important differences unless every variable is examined. Therefore, without level one evidence, it is difficult to confidently derive conclusions about watchful waiting versus routine repair of asymptomatic PEHs. As such, we agree with the 2013 SAGES guidelines that decision-making for the asymptomatic patient should be conducted on a case-by-case basis after discussion of the risks and benefits with the patient (12).
Assessing the risk for elective surgery
Despite the low modern rates of morbidity and mortality, surgical intervention is not without complications. PEH surgery complications can include visceral injury, vagal nerve injury, pneumothorax, and mediastinal hemorrhage, among others (28). When considering the routine repair of an asymptomatic hernia, it is important to identify important risk factors of the patient. This is both for optimization and for the informed consent discussion.
As was previously mentioned, Jassim et al. found that overall risk of complication during and following elective and non-elective PEH repair was associated with chronic lung disease, electrolyte disorders, and weight loss/malnutrition. Lower rates of complication were significantly associated with female sex, elective and laparoscopic procedures (30). Increasing age was also associated with an increased overall risk of complication and mortality following elective and non-elective PEH repair.
Augustin et al. found an inverse relationship between BMI and mortality. Their study found that BMI 25-50 and BMI ≥30 (vs. BMI <18.5) were significantly protective of mortality (33). Frailty and preoperative sepsis increased the odds of mortality.
The finding from Jassim et al. for the risk associated with chronic lung disease was also identified by other studies. Ballian et al. used stepwise logistic regression to identify variables predictive of postoperative mortality and morbidity (32). They found peri-operative mortality was best predicted by history of congestive heart failure, history of pulmonary disease, age at operation (≥80 vs. <80) and urgency of operation (elective vs. emergency).
Management of recurrent hiatal hernia
Management of the recurrent hiatal hernia is also important, given the high overall recurrence rates. Lidor et al. prospectively evaluated 101 patients who underwent elective laparoscopic PEH repair with bioprosthetic mesh. They noticed that those patients who had a return of their symptoms (dysphagia, early satiety, bloating, postprandial chest pain and shortness of breath) tended to have a recurrent hiatal hernia greater than 2 cm based on upper gastrointestinal barium contrast exam (43). Lidor et al. therefore determined that hiatal hernias less than or equal to 2 cm were not clinically significant and should not count as a recurrence. They advocated for repair of all symptomatic recurrent hernias greater than 2 cm.
Jones et al. conducted a retrospective analysis of all patients who underwent PEH repair with mesh over a 9-year period (44). Seventy-nine percent of these patients had upper GI studies post operatively to screen for radiologic recurrence. These studies were repeated annually until the patients were lost to follow-up. The resultant mean follow-up period was 25 months. The median size of recurrence during this follow-up was 4 cm. There was no significant difference in post-operative symptoms between patients with or without radiological occurrence.
White et al. followed 31 patients for 11.3 years and found a statistically significant reduction in symptoms of dysphagia, heartburn, chest pain, and regurgitation after surgery. Patients were assessed with barium swallow, and 32% of the patients were found to have recurrent hiatal hernia. Eighty percent of these recurrences were sliding hiatal hernias. The authors argue that despite the relatively high rate of recurrence of hernia overall, patients benefit symptomatically following PEH surgery, and that recurrences in the form of type I hiatal hernia do not put the patient at increased risk for volvulus (17).
Hiatal hernia repair in special populations
Hiatal hernia repair in the elderly
Gangopadhyay et al. compared outcomes between different age groups following laparoscopic PEH repair (35). Researchers found that older patients had a significantly higher ASA class, and required significantly longer post-operative length of stays. Older patients ultimately had similar long-term outcomes in terms of post-operative symptomology, recurrence and reoperation. These results suggest that older patients are more vulnerable in the perioperative period, but that they are likely to have similar long-term outcomes. Spaniolas et al. similarly concluded that while perioperative morbidity was higher in older patients, mortality did not differ between older and comparatively younger patients (45).
Interestingly, Gupta et al. made the argument that age and comorbidities alone should not determine whether or not a patient received PEH repair (46). They compared outcomes between patients undergoing PEH repair and surgery for GERD to find that differences in mortality are better explained by perioperative pulmonary complications, venous thromboembolic events, and hemorrhage, then they are by age and comorbidities. They made the argument that greater focus should be spent on pulmonary optimization and prophylaxis for thromboembolic events.
El Lakis et al. evaluated 263 patients age 70 or greater and compared them with 261 younger patients. They found that patients aged 80 years or older had more comorbidities, larger hernias, increased proportion of type IV PEH, and were more likely to present emergently (47). Within this older cohort, there was a statistically significant increase in postoperative complications [45 (45%) vs. 61 (23%), P<0.001]. The majority of complications were low grade and did contribute to a longer length of stay in this elderly population. Hernia recurrence was no different in this group compared with the rest of the population. Importantly, after adjustment for comorbidities, age was not a significant factor in predicting severe complications, readmission within 30 days, or early recurrence.
Staerkle et al. similarly aggregated data on 360 octogenarians and found no increased rates of intraoperative or postoperative complications, or complication-related reoperations compared with younger patients (48). Similar studies have also been conducted with smaller cohorts and found similar results (49,50). Because these studies have all found excellent or comparable outcomes associated with PEH repair in elderly patients, we believe that age in of itself is not a contraindication for elective surgery. Patients should be evaluated on a case by case basis with optimization of modifiable risk factors.
Concurrent bariatric surgery and hiatal hernia repair
Hefler et al. used the metabolic and bariatric surgery quality improvement database to identify 42,732 patients who had bariatric procedures with concurrent PEH repair (51). This cohort underwent propensity score matching in a one to one ratio to compare with patients who did not have concurrent hiatal hernia repair. Patients were excluded if they had a BMI <35. Revisional surgeries were also excluded. Overall, researchers found no statistically significant difference in 30-day major complications or mortality between the two groups. Readmission rates were higher after concurrent PEH repair (4.0 vs. 3.6%, P=0.002). There were no specific increased risks with PEH repair when subdividing the bariatric surgery into sleeve gastrectomy versus Roux-en-Y gastric bypass. Researchers concluded that concurrent PEH repair incurred minimal additional risk to patients and was feasible.
Should all hiatal hernias be repaired regardless, once in the OR?
Once in the operating room, should all hiatal hernias be repaired regardless of size or symptoms? To answer this question, a closer look at the pathophysiology of reflux is necessary. There has been a longstanding debate over the relative contribution to the anti-reflux mechanism by the diaphragmatic crura and the lower esophageal sphincter (LES). In the days of Dr. Nissen, a hiatal hernia was believed to be a side-effect related to an incompetent LES. A theory emerged, where prolonged esophageal exposure to acidic refluxate resulted in esophageal shortening. Dr. Nissen believed that once the stomach was reduced back into the abdomen, a fundoplication would prevent future acid exposure and esophageal shortening. In this pathophysiologic theory of GERD, the hiatal hernia repair was not an important component of the anti-reflux operation. Here, the diaphragm was a bystander only, and did not contribute to the GERD barrier.
An alternative viewpoint is that dysfunction of the diaphragmatic crura actively contributes to GERD, in concert with dysfunction of the LES. Both high resolution manometry and three-dimensional computer modeling point towards the diaphragmatic crura and the LES contributing equally to the anti-reflux barrier (52,53). Additionally, studies have shown that microscopic alterations in the cyto-architecture of the diaphragmatic crura are present in those patients with GERD symptoms (54). Animal studies have shown that disruption of the diaphragm alone causes increased esophageal acid exposure (55). Finally, a study of healthy asymptomatic patients with small hiatal hernias still had intrasphincteric reflux and lengthening of the cardiac mucosa based on high resolution pH monitoring and biopsy (56).
It therefore stands to reason that if there are certain patients with a proclivity for the development of hiatal hernia, and if the crura is an important component of the reflux barrier, then if a hiatal hernia is identified intra-operatively, it should be repaired, regardless of its size. This contrasts with the aforementioned evidence that patients with clinically small hiatal hernias identified on video esophagram can be safely observed (43). Although this is true and the presence of the hernia does not necessarily indicate an immediate need for operation, there is an argument that once the patient reaches the operating room, a repair should be done, given the crura’s important contribution to protect against GERD. This was demonstrated in a retrospective study comparing minimal dissection during placement of a LINX® device, and a mandatory more extensive hiatal dissection and repair (57). In the mandatory group, a hiatal dissection and posterior cruroplasty was performed in all patients, regardless of whether a hiatal hernia was present. At an average follow-up time of 298 days, the minimal dissection group had a higher incidence of hiatal hernia recurrence necessitating repair (6.6% vs. 0%, P=0.02). Interestingly, the obligatory dissection group had a larger mean hiatal hernia size identified intraoperatively (3.95 vs. 0.77 cm). Nevertheless, these patients fared better than their counterparts who had not received the cruroplasty.
Conclusions
Although the literature is complex and occasionally conflicting, there are trends which emerge when the entire picture is viewed from a broad perspective. Because type I hiatal hernias are very rarely associated with emergency complications, the literature supports only repairing those hernias which are symptomatic. For type II-IV hiatal hernias, the literature also supports repair of those hernias which are symptomatic. For hernias which are asymptomatic, the literature is conflicting. As such, the best course of action is a carefully held discussion between patient and surgeon on the risks and benefits of elective repair versus watchful waiting. Patients should be optimized for surgery with careful attention to their modifiable risk factors. Age is not a contraindication to surgery. Concurrent hiatal hernia repair and bariatric surgery appears feasible, but a higher level of evidence should be pursued. Finally, additional population-based studies are required to determine the true incidence and ideal management of asymptomatic hiatal hernias of all types.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee L Swanstrom and Steven G. Leeds) for the series “Hiatal Hernia” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2020.04.02). The series “Hiatal Hernia” was commissioned by the editorial office without any funding or sponsorship. JCL and NAB report personal fees from Ethicon, manufacturer of LINX device, outside the submitted work. The authors have no other of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stål P, Lindberg G, Ost A, et al. Gastroesophageal reflux in healthy subjects. Significance of endoscopic findings, histology, age, and sex. Scand J Gastroenterol 1999;34:121-8. [Crossref] [PubMed]
- O'Donnell FL, Taubman SB. Incidence of hiatal hernia in service members, active component, U.S. Armed Forces, 2005-2014. MSMR 2016;23:11-5. [PubMed]
- Gordon C, Kang JY, Neild PJ, et al. The role of the hiatus hernia in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2004;20:719-32. [Crossref] [PubMed]
- Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut Liver 2011;5:267-77. [Crossref] [PubMed]
- Schieman C, Grondin SC. Paraesophageal hernia: clinical presentation, evaluation, and management controversies. Thorac Surg Clin 2009;19:473-84. [Crossref] [PubMed]
- Dellaportas D, Papaconstantinou I, Nastos C, et al. Large Paraesophageal Hiatus Hernia: Is Surgery Mandatory? Chirurgia (Bucur) 2018;113:765-71. [Crossref] [PubMed]
- Carrott PW, Hong J, Kuppusamy M, et al. Clinical ramifications of giant paraesophageal hernias are underappreciated: making the case for routine surgical repair. Ann Thorac Surg 2012;94:421-6; discussion 426-8. [Crossref] [PubMed]
- Diaz S, Brunt LM, Klingensmith ME, et al. Laparoscopic paraesophageal hernia repair, a challenging operation: medium-term outcome of 116 patients. J Gastrointest Surg 2003;7:59-67. [Crossref] [PubMed]
- Polomsky M, Hu R, Sepesi B, et al. A population-based analysis of emergent vs. elective hospital admissions for an intrathoracic stomach. Surg Endosc 2010;24:1250-5. [Crossref] [PubMed]
- Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg 1967;53:33-54. [Crossref] [PubMed]
- Sihvo EI, Salo JA, Räsänen JV, et al. Fatal complications of adult paraesophageal hernia: a population-based study. J Thorac Cardiovasc Surg 2009;137:419-24. [Crossref] [PubMed]
- Kohn GP, Price RR, DeMeester SR, et al. Guidelines for the management of hiatal hernia. Surg Endosc 2013;27:4409-28. [Crossref] [PubMed]
- Ahmed SK, Bright T, Watson DI. Natural history of endoscopically detected hiatus herniae at late follow-up. ANZ J Surg 2018;88:E544-7. [Crossref] [PubMed]
- Scheffer RC, Bredenoord AJ, Hebbard GS, et al. Effect of proximal gastric volume on hiatal hernia. Neurogastroenterol Motil 2010;22:552-6, e120.
- Köckerling F, Trommer Y, Zarras K, et al. What are the differences in the outcome of laparoscopic axial (I) versus paraesophageal (II-IV) hiatal hernia repair? Surg Endosc 2017;31:5327-41. [Crossref] [PubMed]
- Lidor AO, Steele KE, Stem M, et al. Long-term quality of life and risk factors for recurrence after laparoscopic repair of paraesophageal hernia. JAMA Surg 2015;150:424-31. [Crossref] [PubMed]
- White BC, Jeansonne LO, Morgenthal CB, et al. Do recurrences after paraesophageal hernia repair matter?: Ten-year follow-up after laparoscopic repair. Surg Endosc 2008;22:1107-11. [Crossref] [PubMed]
- Rathore MA, Andrabi SI, Bhatti MI, et al. Metaanalysis of recurrence after laparoscopic repair of paraesophageal hernia. JSLS 2007;11:456-60. [PubMed]
- Carrott PW, Hong J, Kuppusamy M, et al. Repair of giant paraesophageal hernias routinely produces improvement in respiratory function. J Thorac Cardiovasc Surg 2012;143:398-404. [Crossref] [PubMed]
- Wirsching A, Klevebro F, Boshier PR, et al. The other explanation for dyspnea: giant paraesophageal hiatal hernia repair routinely improves pulmonary function. Dis Esophagus 2019; [Crossref] [PubMed]
- Low DE, Simchuk EJ. Effect of paraesophageal hernia repair on pulmonary function. Ann Thorac Surg 2002;74:333-7; discussion 337. [Crossref] [PubMed]
- Milito P, Lombardi M, Asti E, et al. Influence of large hiatus hernia on cardiac volumes. A prospective observational cohort study by cardiovascular magnetic resonance. Int J Cardiol 2018;268:241-4. [Crossref] [PubMed]
- Targarona EM, Novell J, Vela S, et al. Mid term analysis of safety and quality of life after the laparoscopic repair of paraesophageal hiatal hernia. Surg Endosc 2004;18:1045-50. [Crossref] [PubMed]
- Sorial RK, Ali M, Kaneva P, et al. Modern era surgical outcomes of elective and emergency giant paraesophageal hernia repair at a high-volume referral center. Surg Endosc 2020;34:284-9. [Crossref] [PubMed]
- Mehta S, Boddy A, Rhodes M. Review of outcome after laparoscopic paraesophageal hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 2006;16:301-6. [Crossref] [PubMed]
- Velanovich V, Karmy-Jones R. Surgical management of paraesophageal hernias: outcome and quality of life analysis. Dig Surg 2001;18:432-7; discussion 437-8. [Crossref] [PubMed]
- Pierre AF, Luketich JD, Fernando HC, et al. Results of laparoscopic repair of giant paraesophageal hernias: 200 consecutive patients. Ann Thorac Surg 2002;74:1909-15; discussion 1915-6.
- Andujar JJ, Papasavas PK, Birdas T, et al. Laparoscopic repair of large paraesophageal hernia is associated with a low incidence of recurrence and reoperation. Surg Endosc 2004;18:444-7. [Crossref] [PubMed]
- Targarona EM, Grisales S, Uyanik O, et al. Long-term outcome and quality of life after laparoscopic treatment of large paraesophageal hernia. World J Surg 2013;37:1878-82. [Crossref] [PubMed]
- Jassim H, Seligman JT, Frelich M, et al. A population-based analysis of emergent versus elective paraesophageal hernia repair using the Nationwide Inpatient Sample. Surg Endosc 2014;28:3473-8. [Crossref] [PubMed]
- Tam V, Luketich JD, Winger DG, et al. Non-Elective Paraesophageal Hernia Repair Portends Worse Outcomes in Comparable Patients: a Propensity-Adjusted Analysis. J Gastrointest Surg 2017;21:137-45. [Crossref] [PubMed]
- Ballian N, Luketich JD, Levy RM, et al. A clinical prediction rule for perioperative mortality and major morbidity after laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg 2013;145:721-9. [Crossref] [PubMed]
- Augustin T, Schneider E, Alaedeen D, et al. Emergent Surgery Does Not Independently Predict 30-Day Mortality After Paraesophageal Hernia Repair: Results from the ACS NSQIP Database. J Gastrointest Surg 2015;19:2097-104. [Crossref] [PubMed]
- Poulose BK, Gosen C, Marks JM, et al. Inpatient mortality analysis of paraesophageal hernia repair in octogenarians. J Gastrointest Surg 2008;12:1888-92. [Crossref] [PubMed]
- Gangopadhyay N, Perrone JM, Soper NJ, et al. Outcomes of laparoscopic paraesophageal hernia repair in elderly and high-risk patients. Surgery 2006;140:491-8; discussion 498-9. [Crossref] [PubMed]
- Kheterpal S, Tremper KK, Heung M, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology 2009;110:505-15. [Crossref] [PubMed]
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006;144:581-95. [Crossref] [PubMed]
- Paredes S, Cortinez L, Contreras V, et al. Post-operative cognitive dysfunction at 3 months in adults after non-cardiac surgery: a qualitative systematic review. Acta Anaesthesiol Scand 2016;60:1043-58. [Crossref] [PubMed]
- Witlox J, Eurelings LS, de Jonghe JF, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 2010;304:443-51. [Crossref] [PubMed]
- Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal Hernias: Operation or Observation? Annals of Surgery 2002;236:492-500. [Crossref] [PubMed]
- Morrow EH, Chen J, Patel R, et al. Watchful waiting versus elective repair for asymptomatic and minimally symptomatic paraesophageal hernias: A cost-effectiveness analysis. Am J Surg 2018;216:760-3. [Crossref] [PubMed]
- Jung JJ, Naimark DM, Behman R, et al. Approach to asymptomatic paraesophageal hernia: watchful waiting or elective laparoscopic hernia repair? Surg Endosc 2018;32:864-71. [Crossref] [PubMed]
- Lidor AO, Kawaji Q, Stem M, et al. Defining recurrence after paraesophageal hernia repair: correlating symptoms and radiographic findings. Surgery 2013;154:171-8. [Crossref] [PubMed]
- Jones R, Simorov A, Lomelin D, et al. Long-term outcomes of radiologic recurrence after paraesophageal hernia repair with mesh. Surg Endosc 2015;29:425-30. [Crossref] [PubMed]
- Spaniolas K, Laycock WS, Adrales GL, et al. Laparoscopic paraesophageal hernia repair: advanced age is associated with minor but not major morbidity or mortality. J Am Coll Surg 2014;218:1187-92. [Crossref] [PubMed]
- Gupta A, Chang D, Steele KE, et al. Looking beyond age and co-morbidities as predictors of outcomes in paraesophageal hernia repair. J Gastrointest Surg 2008;12:2119-24. [Crossref] [PubMed]
- El Lakis MA, Kaplan SJ, Hubka M, et al. The Importance of Age on Short-Term Outcomes Associated With Repair of Giant Paraesophageal Hernias. Ann Thorac Surg 2017;103:1700-9. [Crossref] [PubMed]
- Staerkle RF, Rosenblum I, Köckerling F, et al. Outcome of laparoscopic paraesophageal hernia repair in octogenarians: a registry-based, propensity score-matched comparison of 360 patients. Surg Endosc 2019;33:3291-9. [Crossref] [PubMed]
- Khoma O, Mugino M, Falk GL. Is repairing giant hiatal hernia in patients over 80 worth the risk? Surgeon 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Hazebroek EJ, Gananadha S, Koak Y, et al. Laparoscopic paraesophageal hernia repair: quality of life outcomes in the elderly. Dis Esophagus 2008;21:737-41. [Crossref] [PubMed]
- Hefler J, Dang J, Mocanu V, et al. Concurrent bariatric surgery and paraesophageal hernia repair: an analysis of the Metabolic and Bariatric Surgery Association Quality Improvement Program (MBSAQIP) database. Surg Obes Relat Dis 2019;15:1746-54. [Crossref] [PubMed]
- Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102:1056-63. [Crossref] [PubMed]
- Yassi R, Cheng LK, Rajagopal V, et al. Modeling of the mechanical function of the human gastroesophageal junction using an anatomically realistic three-dimensional model. J Biomech 2009;42:1604-9. [Crossref] [PubMed]
- Zifan A, Kumar D, Cheng LK, et al. Three-Dimensional Myoarchitecture of the Lower Esophageal Sphincter and Esophageal Hiatus Using Optical Sectioning Microscopy. Sci Rep 2017;7:13188. [Crossref] [PubMed]
- Mittal RK, Sivri B, Schirmer BD, et al. Effect of crural myotomy on the incidence and mechanism of gastroesophageal reflux in cats. Gastroenterology 1993;105:740-7. [Crossref] [PubMed]
- Robertson EV, Derakhshan MH, Wirz AA, et al. Hiatus hernia in healthy volunteers is associated with intrasphincteric reflux and cardiac mucosal lengthening without traditional reflux. Gut 2017;66:1208-15. [Crossref] [PubMed]
- Tatum JM, Alicuben E, Bildzukewicz N, et al. Minimal versus obligatory dissection of the diaphragmatic hiatus during magnetic sphincter augmentation surgery. Surg Endosc 2019;33:782-8. [Crossref] [PubMed]
Cite this article as: Dunn CP, Patel TA, Bildzukewicz NA, Henning JR, Lipham JC. Which hiatal hernia’s need to be fixed? Large, small or none? Ann Laparosc Endosc Surg 2020;5:29.