Peroral endoscopic myotomy for achalasia—a review
Introduction
Achalasia is a relatively rare cause of dysphagia manifest by esophageal aperistalsis and failure of relaxation of a hypertensive lower esophageal sphincter (LES). For many decades treatment has been directed towards facilitating reduction in sphincter pressure. While mechanical stretching methods with esophageal dilators and muscle relaxation with botulinum toxin injection have been commonly used as treatment modalities, the associated recidivism rates of the disease make them less than ideal options (1).
Guidelines suggest that the current gold standard treatment of achalasia is division of the LES mechanism (1). This myotomy aims to divide the circular muscle fibers of the LES while preserving the underlying esophageal mucosa intact. While initial approaches to myotomy were transthoracic, today a laparoscopic approach is far more common. To prevent gastroesophageal reflux after myotomy a concomitant fundoplication is recommended (1).
First reported by Inoue in 2010 (2), an endoscopic tunneled approach to myotomy, termed “peroral endoscopic myotomy” (POEM), is rapidly gaining popularity. The total number of POEM procedures performed worldwide is in the thousands, though exact numbers are difficult to determine as no centralized registry exists. The largest numbers are probably from Asia, with more than 1,300 having been performed in China (3) and more than 1,000 in Japan (4).
Proposed benefits of this approach include the ability to perform a longer myotomy, less disruption of the angle of His anatomy that may obviate the need for a concomitant fundoplication, a less morbid procedure, a better cosmetic result, and possibly a quicker recovery. In addition, POEM has been performed in patients with recurrent dysphagia after prior surgical myotomy where the ability to perform the endoscopic procedure through virginal tissue planes is beneficial.
Indications for POEM
Most initial reports of POEM were for the indication of symptomatic achalasia with progressive dysphagia or weight loss. The vast majority of these were for POEM as a primary therapy of achalasia and this indication forms the focus of this manuscript. However, with increasing experience the indications have broadened (5). POEM has been applied as a revisional procedure after prior medical therapy, dilatation (6), or surgical myotomy (7,8). By permitting myotomy on any aspect of the esophagus and particularly posteriorly, POEM allows a virginal tissue plane to be developed away from a previous myotomy (9).
As compared to transabdominal or transthoracic myotomy, the myotomy performed during POEM is easier to extend into both the chest and the abdomen, allowing for a longer myotomy. This feature has made POEM an option for the treatment of distal esophageal spasm (10-12) and esophageal hypercontractility (“Jackhammer esophagus”, including hypertensive “nutcracker esophagus”) (13-16). Resolution of chest pain associated with jackhammer esophagus or distal esophageal spasm has been reported in case studies to occur in over 90% of patients (17). The indications for the natural orifice endoluminal approach of POEM has been expanded to the treatment of gastroparesis with an endoscopic tunneled pyloromyotomy, so-called G-POEM (18).
Patient preparation for the procedure
The diagnosis of achalasia or other indication must be confirmed with esophageal manometry, and other investigations as required. According to surveys of experienced POEM practitioners, certain comorbidities should be considered as contraindications for POEM, including prior mediastinal irradiation, severe pulmonary disease, coagulopathy, or portal hypertension even without evidence of esophageal varices (5). Some physicians prescribe antibiotics or antifungal medications preoperatively (19). The procedure is performed under general anesthesia with endotracheal intubation. This protects the airway and allows positive pressure ventilation, which reduces the risk and extent of mediastinal emphysema. The upper abdomen may be prepared with antiseptic to allow access for needle decompression to prevent significant abdominal distention during the procedure that might lead to abdominal compartment syndrome.
POEM technique
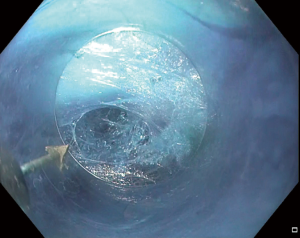
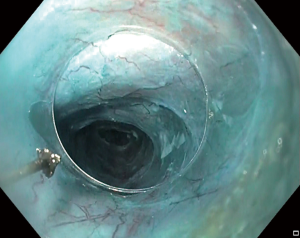
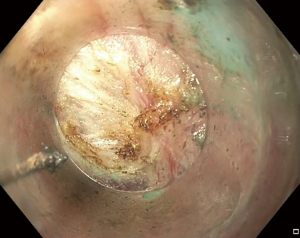
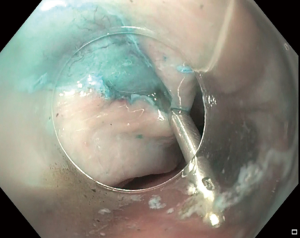
Inoue initially described an 8 cm myotomy (2 cm below the gastroesophageal junction and 6 cm above), though this has been extended to greater than 12 cm in some studies (19) and also reduced in others (20). At the commencement of the procedure, endoscopic evaluation of the esophagus and the stomach is performed and the landmarks of the LES and of the planned location of mucosotomy are identified. Carbon dioxide insufflation is used; air insufflation is contraindicated (20,21) due to a higher risk of complications such as pneumothorax. A high-definition forward-viewing gastroscope with a plastic cap is used (5). The esophageal mucosa is breached more proximally via a longitudinal mucosotomy to allow introduction of the endoscope into the submucosal space (Figure 1). Whether the mucosotomy is made in the anterior or the posterior aspect of the esophagus is at the discretion of the physician (5,22), though performance of the procedure through virginal tissue planes seems reasonable; after failed anterior Heller myotomy (HM), a posterior esophageal POEM is effective (3,23). The submucosal tunnel (Figure 2) is extended beyond the LES onto the gastric wall. This is confirmed by retroflex view in the stomach confirming submucosal staining of the gastric mucosa with injectate. Various solutions have been used for the injectate, including indigo carmine, methylene blue and patent blue V. The circular esophageal muscle layer is then divided by electrocautery under vision starting either proximally or distally (Figure 3). Though the longitudinal esophageal muscle layer does not require division, if divided there appears to be no adverse effect on outcome (24). The proximal extent of the myotomy should be 2 cm distal to the distal point of the mucosotomy to allow a flap closure of the mucosa and presumed decrease in postoperative esophageal leak. After the myotomy is completed, the mucosotomy is closed using either endoscopic clips or suturing devices (Figure 4). Some physicians irrigate the submucosal tunnel with saline or antibiotic solution prior to closure.
A postprocedure gastroscopy is performed to confirm mucosal integrity. Postoperative contrast radiology, either a contrast esophagram or a CT (25), is often performed to confirm passage of contrast through the gastroesophageal junction without extravasation. These tests are very sensitive in detecting radiological leaks but the rate of clinically significant leaks is lower and investigation may not always be required (26).
Outcomes
Systematic review of the POEM literature is limited by marked heterogeneity of patient populations, techniques, reported outcomes and timepoints, making evaluation of effects difficult. Rather than making firm conclusions, a narrative description of comparative effects is all that may be usefully produced.
Safety of the procedure
The safety of POEM is well established and perioperative morbidity is comparable to that seen after LHM. The existing literature demonstrates a low incidence of complications after POEM in both adults and children (19,27-38). A pooled analysis found a 0.3% incidence of leak after POEM (39); early in one particular series the leak rate was 6% (17) suggesting a learning curve effect. The overall serious adverse event rate in one of the largest single center series (n=500) was 3.2%; all were managed conservatively with no perioperative mortality (40,41). Mucosal perforation rates vary between 0 and 25% is reported series, but are usually less than 10% (40). Comparative studies show near equivalence or perforation rates between POEM and LHM (42-49). The vast majority can be repaired endoscopically (50), and the effect of these perforations is usually minimal.
Rates of complications including leak are comparable to LHM (38,51) and surrogate measures of these leaks, such as unexpected Intensive Care Unit admissions, show no difference in comparative studies (43,45,48,49). Reported POEM-related complications include the development of subcutaneous emphysema, mediastinal emphysema, mediastinitis, pleural effusion, pneumothorax, pneumoperitoneum, peritonitis, delayed hemorrhage, and atrial fibrillation (21,52-54). While the majority of these complications can also occur after a surgical myotomy, complications unique to POEM such as retention of the endoscopic submucosal dissection cap, gas-related complications and dehiscence of the mucosotomy closure leading to food retention have also been reported (52,55-57).
Bleeding can occur during the POEM procedure or postoperatively into the submucosal tunnel. This can be severe, causing hematemesis, retrosternal pain or hemorrhagic shock (40). The incidence of severe bleeding is approximately 1.1% in a large metanalysis (39). Delayed postoperative bleeding occurs in less than 1% of procedures (32,41,58). Procedure-related deaths are very rare and similar to rates after LHM (45).
Based on non-randomized cohort studies, it appears that POEM has a shorter operating time with less perioperative blood loss than LHM (38,43,47,59-64).
In regards to requirements for postoperative analgesia, one study reported similar postoperative pain scores and analgesic requirements between POEM and LHM (35,43), while others found patients had less pain after POEM (47). A systematic review of the available evidence has not demonstrated a significant difference in postoperative pain scores (65). Hospital length of stay and time to return to normal diet are similar between POEM and LHM (59,65).
Dysphagia
As a key outcome measure, the resolution of dysphagia after POEM is achieved in up to 95% (32,56) of patients in the short-term. POEM has been demonstrated to consistently reduce LES pressure (28,66), increase gastroesophageal junction diameter (67), and promote esophageal emptying (68,69). Long-term relief of dysphagia is lower (70) and has been reported to be 80% at 2 years (71).
Early dysphagia after POEM has been shown to be lower compared to LHM, possibly due to the lesser manipulation and subsequent inflammation and edema at the gastroesophageal junction after POEM (38). On the other hand, noncomparative studies have suggested Eckhart dysphagia scores to be equivalent between the two procedures at 6 months, with both procedures improving dysphagia in more than 95% of patients. This is likely a direct result of similar decreases in lower esophageal sphincter pressure observed after both procedures. One study reported that postmyotomy LES resting pressures but not LES relaxation pressures were higher after POEM than after LHM (38), without effect on dysphagia rates.
Comparative studies strongly support equivalence in improvement of dysphagia symptoms for POEM and LHM (38,44,49,59,64,72) with this finding supported by other systematic reviews (35,65), though with a possible greater efficacy of POEM at least in the short-term (59,60,73,74). Also, there are equivalent improvements in the integrated relaxation pressure of the lower esophageal sphincter (61,66).
Few comparative studies have examined Eckhardt dysphagia scores for POEM vs. HM (48,64), but results seem similar with equivalent Eckhardt scores are seen at 1 year post-procedure.
There is also some evidence supporting the benefit of POEM over pneumatic dilatation in the improvement of dysphagia (75,76).
Much has been written about the presumed benefit of POEM over HM in the treatment of achalasia subtype III due to the fact that it is easier to extend the myotomy proximally in the endoscopic procedure. However, there is a marked paucity of data to support a recommendation in this respect, and some data to the contrary (77).
With both efficacy and safety having been demonstrated as equivalent, the major outcomes of interest in deciding upon POEM versus LHM for the treatment of achalasia are long-term rates of gastro-esophageal reflux (GER) and long-term quality of life (QOL) scores. Additionally, as most HM operations are accompanied by a partial fundoplication, a comparison of fundoplication-related side-effects must be considered, including bloating, rectal flatulence and the ability to belch. These outcomes have been evaluated to varying degrees in the body of literature currently available.
Gastroesophageal reflux
Fundoplication is strongly recommended to be performed at the time of LHM (78,79), as without it many patients will develop evidence of reflux. It has been argued that the lack of mobilization of the esophagus at the diaphragmatic hiatus during POEM may decrease postoperative reflux and therefore make a fundoplication unnecessary after this procedure, and prevent potential fundoplication associated functional side-effects such as gas bloat. Nevertheless, GER is common after POEM and studies have documented abnormal distal esophageal acid exposure in one-third to one-half of patients following POEM (17,32,38,80).
Gastroesophageal reflux results from increased distensibility of the lower esophageal sphincter zone and it has been postulated—as POEM results in higher distensibility index of this area as compared to HM with fundoplication (74)—that POEM may result in higher rates of GER. However, evidence for this is lacking and a major limitation of the literature is a marked absence of prospectively collected comparative postoperative pH data for POEM and other procedures. It is possible that the postoperative distensibility index, as measured by EndoFLIP (EndoFLIP, Medtronic, USA), may be more of a predictor for long-term GER rather than the procedure itself (74,81).
Systematic reviews have concluded that both short- and long-term GER symptoms (as opposed to objective evidence for reflux) are comparable between POEM and HM (73), based on some comparative data (38). There is a poor correlation between elevated distal esophageal acid exposure post-POEM and symptoms of reflux (82). Indeed, in patient populations reviewed after previous antireflux surgery, the use of PPI medications was actually poorly correlated associated with objective evidence of recurrent and it seems reasonable to expect the situation to not be dissimilar post POEM procedure (82).
Some noncomparative studies have reported heartburn or esophagitis in approximately 25% of patients after POEM (32) but severe esophagitis and reflux strictures have also been reported (71). Strictures can result in late recurrence of dysphagia and have led some to recommend routine post-POEM use of proton pump inhibitor medication (71).
There is little in the way of comparative data of GER rates between POEM and HM. That which exists supports near equivalence of GER, at least in the short-term (38,45,49,83), though with a probable trend towards higher long-term rates post POEM (61,84).
Quality of life
Disease-specific and general QOL scores have both been reported to improve after POEM, with improvements in SF-36 scores, emotional wellbeing, social functioning and general health evident at 6 months after the procedure (33,47,85). Comparison with HM shows similar improvements in postoperative global quality of life scores (63).
Post-fundoplication symptoms
No comparative studies exist comparing bloating after HM and POEM. Further investigation with longer term GER outcomes after POEM is needed. This area of study is particularly important as the putative cause of bloating—the fundoplication—is routinely performed after HM but not after POEM or pneumatic dilatation (notwithstanding the availability of some techniques of endoscopic fundoplication).
Learning curve
POEM requires a demanding skill set that involves both advanced endoscopic skills and knowledge of surgical anatomy and complication management.
Proctoring is necessary for the first few cases to ensure good outcomes. The number of proctored cases should be based on the endoscopic skills of the surgeon and how quickly they learn the technique (5,86,87). Improvements in operating time and ease of performing the procedure have been reported to occur between 20 and 60 cases (88-91).
Cost
Very little comparative data exists between POEM and alternative procedures. One identified study suggested a cost-saving of great than USD $3,000 ($17,782 vs. $14,481) for the POEM procedure over robotic HM (62) when performed in a major United States medical center. Others, also based in the United States have found similarities in cost between standard HM and POEM (92), perhaps favoring POEM in the long-term but with a large degree of uncertainty in the actuarial analysis (93).
Direction for further study
Some major questions still exist regarding comparative outcomes between POEM, LHM and esophageal pneumatic dilatation:
- Which procedure has the lowest rate of long-term GERD as determined by objective criteria of positive pH studies or reflux esophagitis?
- Does the absence of a fundoplication with the POEM procedure improve the incidence of postoperative bloating and improve quality of life as compared to HM?
These questions will only be answered by further comparative studies. Encouragingly, randomized controlled trials are currently ongoing comparing POEM with LHM (NCT01601678) and POEM vs. pneumatic dilation (NCT01793922) and are expected to report their results within the next few years.
Summary
With large number of POEM procedures now having been performed world-wide, the procedure has been demonstrated to be safe and effective in the management of achalasia. The procedure has certainly moved beyond the experimental phase into an era of ongoing outcomes surveillance. Furthermore, POEM has shown utility for use in revisional surgery.
Questions remain about the objectively-diagnosed incidence and implications of GER after the POEM procedure. Questions also remain regarding the prevalence and effect of postoperative bloating, rectal flatulence and inability to belch in POEM as compared to LHM with fundoplication. These two areas should be the focus of future comparative trials.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Muhammed Ashraf Memon and Abe Fingerhut) for the series “Laparoendoscopic Surgery for Benign Oesophagogastric Conditions” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.08.11). The series “Laparoendoscopic Surgery for Benign Oesophagogastric Conditions” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stefanidis D, Richardson W, Farrell TM, et al. SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 2012;26:296-311. [Crossref] [PubMed]
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. [Crossref] [PubMed]
- Li QL, Zhou PH. Perspective on peroral endoscopic myotomy for achalasia: Zhongshan experience. Gut Liver 2015;9:152-8. [Crossref] [PubMed]
- Bechara R, Onimaru M, Ikeda H, et al. Per-oral endoscopic myotomy, 1000 cases later: pearls, pitfalls, and practical considerations. Gastrointest Endosc 2016;84:330-8. [Crossref] [PubMed]
- Stavropoulos SN, Desilets DJ, Fuchs KH, et al. Per-oral endoscopic myotomy white paper summary. Surg Endosc 2014;28:2005-19. [Crossref] [PubMed]
- Ling T, Guo H, Zou X. Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospective case-control study. J Gastroenterol Hepatol 2014;29:1609-13. [Crossref] [PubMed]
- Fernandez-Ananin S, Fernandez AF, Balague C, et al. What to do when Heller's myotomy fails? Pneumatic dilatation, laparoscopic remyotomy or peroral endoscopic myotomy: A systematic review. J Minim Access Surg 2018;14:177-84. [Crossref] [PubMed]
- Nabi Z, Ramchandani M, Chavan R, et al. Peroral endoscopic myotomy in treatment-naive achalasia patients versus prior treatment failure cases. Endoscopy 2018;50:358-70. [Crossref] [PubMed]
- Vigneswaran Y, Yetasook AK, Zhao JC, et al. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 2014;18:1071-6. [Crossref] [PubMed]
- Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy 2014;46 Suppl 1 UCTN:E79-81.
- Hoppo T, Thakkar SJ, Schumacher LY, et al. A utility of peroral endoscopic myotomy (POEM) across the spectrum of esophageal motility disorders. Surg Endosc 2016;30:233-44. [Crossref] [PubMed]
- Shiwaku H, Inoue H, Beppu R, et al. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc 2013;77:149-50. [Crossref] [PubMed]
- Kandulski A, Fuchs KH, Weigt J, et al. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM). Dis Esophagus 2016;29:695-6. [Crossref] [PubMed]
- Khashab MA, Saxena P, Kumbhari V, et al. Peroral endoscopic myotomy as a platform for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc 2014;79:136-9. [Crossref] [PubMed]
- Ko WJ, Lee BM, Park WY, et al. Jackhammer esophagus treated by a peroral endoscopic myotomy. Korean J Gastroenterol 2014;64:370-4. [Crossref] [PubMed]
- Kristensen HØ, Bjerregaard NC, Rask P, et al. Peroral endoscopic myotomy (POEM) for nutcracker esophagus. Three cases with 12 months follow-up. Scand J Gastroenterol 2014;49:1285-9. [Crossref] [PubMed]
- Sharata AM, Dunst CM, Pescarus R, et al. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 2015;19:161-70; discussion 70. [Crossref] [PubMed]
- Gonzalez JM, Vanbiervliet G, Vitton V, et al. First European human gastric peroral endoscopic myotomy, for treatment of refractory gastroparesis. Endoscopy 2015;47:E135-6. [Crossref] [PubMed]
- Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg 2011;213:751-6. [Crossref] [PubMed]
- Wang J, Tan N, Xiao Y, et al. Safety and efficacy of the modified peroral endoscopic myotomy with shorter myotomy for achalasia patients: a prospective study. Dis Esophagus 2015;28:720-7. [Crossref] [PubMed]
- Cai MY, Zhou PH, Yao LQ, et al. Thoracic CT after peroral endoscopic myotomy for the treatment of achalasia. Gastrointest Endosc 2014;80:1046-55. [Crossref] [PubMed]
- Zhang XC, Li QL, Huang Y, et al. Peroral endoscopic myotomy using the posterior approach in an 11-month-old girl with achalasia, severe malnutrition, and recurrent pneumonia. Endoscopy 2015;47 Suppl 1 UCTN:E480-2.
- Kedia P, Sharaiha R, Kumta NA, et al. Salvage posterior peroral endoscopic myotomy. Gastrointest Endosc 2015;81:220-1. [Crossref] [PubMed]
- Li QL, Chen WF, Zhou PH, et al. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 2013;217:442-51. [Crossref] [PubMed]
- Pannu D, Yang D, Abbitt PL, et al. Prospective evaluation of CT esophagram findings after peroral endoscopic myotomy. Gastrointest Endosc 2016;84:408-15. [Crossref] [PubMed]
- El Khoury R, Teitelbaum EN, Sternbach JM, et al. Evaluation of the need for routine esophagram after peroral endoscopic myotomy (POEM). Surg Endosc 2016;30:2969-74. [Crossref] [PubMed]
- Zhou PH, Cai MY, Yao LQ, et al. Peroral endoscopic myotomy for esophageal achalasia: report of 42 cases. Zhonghua Wei Chang Wai Ke Za Zhi 2011;14:705-8. [PubMed]
- von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 2012;107:411-7. [Crossref] [PubMed]
- Familiari P, Marchese M, Gigante G, et al. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr 2013;57:794-7. [Crossref] [PubMed]
- Lee BH, Shim KY, Hong SJ, et al. Peroral endoscopic myotomy for treatment of achalasia: initial results of a korean study. Clin Endosc 2013;46:161-7. [Crossref] [PubMed]
- Yang D, Wagh MS. Peroral endoscopic myotomy for the treatment of achalasia: an analysis. Diagn Ther Endosc 2013;2013:389596 [Crossref] [PubMed]
- Familiari P, Gigante G, Marchese M, et al. Peroral Endoscopic Myotomy for Esophageal Achalasia: Outcomes of the First 100 Patients With Short-term Follow-up. Ann Surg 2016;263:82-7. [Crossref] [PubMed]
- Ling TS, Guo HM, Yang T, et al. Effectiveness of peroral endoscopic myotomy in the treatment of achalasia: a pilot trial in Chinese Han population with a minimum of one-year follow-up. J Dig Dis 2014;15:352-8. [Crossref] [PubMed]
- Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc 2014;26:43-51. [Crossref] [PubMed]
- Talukdar R, Inoue H, Reddy DN. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc 2015;29:3030-46. [Crossref] [PubMed]
- Chen WF, Li QL, Zhou PH, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc 2015;81:91-100. [Crossref] [PubMed]
- Li C, Tan Y, Wang X, et al. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg 2015;50:201-5. [Crossref] [PubMed]
- Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014;259:1098-103. [Crossref] [PubMed]
- Patel K, Abbassi-Ghadi N, Markar S, et al. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus 2016;29:807-19. [Crossref] [PubMed]
- ASGE Technology Committee , Pannala R, Abu Dayyeh BK, et al. Per-oral endoscopic myotomy (with video). Gastrointest Endosc 2016;83:1051-60. [Crossref] [PubMed]
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 2015;221:256-64. [Crossref] [PubMed]
- Fumagalli U, Rosati R, De Pascale S, et al. Repeated Surgical or Endoscopic Myotomy for Recurrent Dysphagia in Patients After Previous Myotomy for Achalasia. J Gastrointest Surg 2016;20:494-9. [Crossref] [PubMed]
- Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 2013;17:228-35. [Crossref] [PubMed]
- Meng F, Li P, Wang Y, et al. Peroral endoscopic myotomy compared with pneumatic dilation for newly diagnosed achalasia. Surg Endosc 2017;31:4665-72. [Crossref] [PubMed]
- Ramirez M, Zubieta C, Ciotola F, et al. Per oral endoscopic myotomy vs. laparoscopic Heller myotomy, does gastric extension length matter? Surg Endosc 2018;32:282-8. [Crossref] [PubMed]
- Schneider AM, Louie BE, Warren HF, et al. A Matched Comparison of Per Oral Endoscopic Myotomy to Laparoscopic Heller Myotomy in the Treatment of Achalasia. J Gastrointest Surg 2016;20:1789-96. [Crossref] [PubMed]
- Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 2013;154:893-7; discussion 7-900. [Crossref] [PubMed]
- Leeds SG, Burdick JS, Ogola GO, et al. Comparison of outcomes of laparoscopic Heller myotomy versus per-oral endoscopic myotomy for management of achalasia. Proc (Bayl Univ Med Cent) 2017;30:419-23. [Crossref] [PubMed]
- Caldaro T, Familiari P, Romeo EF, et al. Treatment of esophageal achalasia in children: Today and tomorrow. J Pediatr Surg 2015;50:726-30. [Crossref] [PubMed]
- Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol 2015;12:410-26. [Crossref] [PubMed]
- Wei M, Yang T, Yang X, et al. Peroral esophageal myotomy versus laparoscopic Heller's myotomy for achalasia: a meta-analysis. J Laparoendosc Adv Surg Tech A 2015;25:123-9. [Crossref] [PubMed]
- Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 2012;26:3267-72. [Crossref] [PubMed]
- Li QL, Zhou PH, Yao LQ, et al. Early diagnosis and management of delayed bleeding in the submucosal tunnel after peroral endoscopic myotomy for achalasia (with video). Gastrointest Endosc 2013;78:370-4. [Crossref] [PubMed]
- Saleem AM, Hennessey H, von Renteln D, et al. Atrial fibrillation as an unexpected complication after peroral endoscopic myotomy (POEM): a case report. Surg Laparosc Endosc Percutan Tech 2014;24:e196-9. [Crossref] [PubMed]
- Baldaque-Silva F, Marques M, Ramalho R, et al. Case description of cap retention in the submucosal tunnel during peroral endoscopic myotomy. Am J Gastroenterol 2012;107:1586. author reply. [Crossref] [PubMed]
- Costamagna G, Marchese M, Familiari P, et al. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis 2012;44:827-32. [Crossref] [PubMed]
- Wang X, Tan Y, Zhang J, et al. Risk factors for gas-related complications of peroral endoscopic myotomy in achalasia. Neth J Med 2015;73:76-81. [Crossref] [PubMed]
- Ramchandani M, Nageshwar Reddy D, Darisetty S, et al. Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc 2016;28:19-26. [Crossref] [PubMed]
- Chan SM, Wu JC, Teoh AY, et al. Comparison of early outcomes and quality of life after laparoscopic Heller's cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig Endosc 2016;28:27-32. [Crossref] [PubMed]
- Kumbhari V, Tieu AH, Onimaru M, et al. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open 2015;3:E195-201. [Crossref] [PubMed]
- de Pascale S, Repici A, Puccetti F, et al. Peroral endoscopic myotomy versus surgical myotomy for primary achalasia: single-center, retrospective analysis of 74 patients. Dis Esophagus 2017;30:1-7. [Crossref] [PubMed]
- Khashab MA, Kumbhari V, Tieu AH, et al. Peroral endoscopic myotomy achieves similar clinical response but incurs lesser charges compared to robotic heller myotomy. Saudi J Gastroenterol 2017;23:91-6. [PubMed]
- Peng L, Tian S, Du C, et al. Outcome of Peroral Endoscopic Myotomy (POEM) for Treating Achalasia Compared With Laparoscopic Heller Myotomy (LHM). Surg Laparosc Endosc Percutan Tech 2017;27:60-4. [PubMed]
- Ward MA, Gitelis M, Patel L, et al. Outcomes in patients with over 1-year follow-up after peroral endoscopic myotomy (POEM). Surg Endosc 2017;31:1550-7. [Crossref] [PubMed]
- Marano L, Pallabazzer G, Solito B, et al. Surgery or Peroral Esophageal Myotomy for Achalasia: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 2016;95:e3001 [Crossref] [PubMed]
- Sanaka MR, Hayat U, Thota PN, et al. Efficacy of peroral endoscopic myotomy vs other achalasia treatments in improving esophageal function. World J Gastroenterol 2016;22:4918-25. [Crossref] [PubMed]
- Familiari P, Gigante G, Marchese M, et al. EndoFLIP system for the intraoperative evaluation of peroral endoscopic myotomy. United European Gastroenterol J 2014;2:77-83. [Crossref] [PubMed]
- Chen X, Li QP, Ji GZ, et al. Two-year follow-up for 45 patients with achalasia who underwent peroral endoscopic myotomy. Eur J Cardiothorac Surg 2015;47:890-6. [Crossref] [PubMed]
- Vigneswaran Y, Tanaka R, Gitelis M, et al. Quality of life assessment after peroral endoscopic myotomy. Surg Endosc 2015;29:1198-202. [Crossref] [PubMed]
- Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 2013;145:309-11.e1-3.
- Werner YB, Costamagna G, Swanstrom LL, et al. Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 2016;65:899-906. [Crossref] [PubMed]
- Hanna AN, Datta J, Ginzberg S, et al. Laparoscopic Heller Myotomy vs Per Oral Endoscopic Myotomy: Patient-Reported Outcomes at a Single Institution. J Am Coll Surg 2018;226:465-72.e1. [Crossref] [PubMed]
- Awaiz A, Yunus RM, Khan S, et al. Systematic Review and Meta-Analysis of Perioperative Outcomes of Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) for Achalasia. Surg Laparosc Endosc Percutan Tech 2017;27:123-31. [Crossref] [PubMed]
- Teitelbaum EN, Soper NJ, Pandolfino JE, et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 2015;29:522-8. [Crossref] [PubMed]
- Zheng Z, Zhao C, Su S, et al. Peroral endoscopic myotomy versus pneumatic dilation - result from a retrospective study with 1-year follow-up. Z Gastroenterol 2019;57:304-11. [Crossref] [PubMed]
- Kim GH, Jung KW, Jung HY, et al. Superior clinical outcomes of peroral endoscopic myotomy compared with balloon dilation in all achalasia subtypes. J Gastroenterol Hepatol 2019;34:659-65. [Crossref] [PubMed]
- Greene CL, Chang EJ, Oh DS, et al. High resolution manometry sub-classification of Achalasia: does it really matter? Does Achalasia sub-classification matter? Surg Endosc 2015;29:1363-7. [Crossref] [PubMed]
- Stefanidis D, Hope WW, Kohn GP, et al. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 2010;24:2647-69. [Crossref] [PubMed]
- Di Corpo M, Farrell TM, Patti MG. Laparoscopic Heller Myotomy: A Fundoplication Is Necessary to Control Gastroesophageal Reflux. J Laparoendosc Adv Surg Tech A 2019;29:721-5. [Crossref] [PubMed]
- Kumbhari V, Khashab MA. Peroral endoscopic myotomy. World J Gastrointest Endosc 2015;7:496-509. [Crossref] [PubMed]
- Kim GH. Is EndoFLIP Useful for Predicting Clinical Outcomes after Peroral Endoscopic Myotomy in Patients with Achalasia? Gut Liver 2019;13:3-4. [Crossref] [PubMed]
- Jones EL, Meara MP, Schwartz JS, et al. Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 2016;30:947-52. [Crossref] [PubMed]
- Kumagai K, Tsai JA, Thorell A, et al. Per-oral endoscopic myotomy for achalasia. Are results comparable to laparoscopic Heller myotomy? Scand J Gastroenterol 2015;50:505-12. [Crossref] [PubMed]
- Sanaka MR, Thota PN, Parikh MP, et al. Peroral endoscopic myotomy leads to higher rates of abnormal esophageal acid exposure than laparoscopic Heller myotomy in achalasia. Surg Endosc 2019;33:2284-92. [Crossref] [PubMed]
- Chiu PW, Wu JC, Teoh AY, et al. Peroral endoscopic myotomy for treatment of achalasia: from bench to bedside (with video). Gastrointest Endosc 2013;77:29-38. [Crossref] [PubMed]
- Tantau M, Crisan D. Peroral endoscopic myotomy: Time to change our opinion regarding the treatment of achalasia? World J Gastrointest Endosc 2015;7:237-46. [Crossref] [PubMed]
- Ren Y, Tang X, Zhi F, et al. A stepwise approach for peroral endoscopic myotomy for treating achalasia: from animal models to patients. Scand J Gastroenterol 2015;50:952-8. [Crossref] [PubMed]
- Kurian AA, Dunst CM, Sharata A, et al. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 2013;77:719-25. [Crossref] [PubMed]
- Pescarus R, Shlomovitz E, Swanstrom LL. Per-oral endoscopic myotomy (POEM) for esophageal achalasia. Curr Gastroenterol Rep 2014;16:369. [Crossref] [PubMed]
- Eleftheriadis N, Inoue H, Ikeda H, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag 2012;8:329-42. [Crossref] [PubMed]
- Teitelbaum EN, Soper NJ, Arafat FO, et al. Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 2014;18:92-8; discussion 8-9. [Crossref] [PubMed]
- Miller HJ, Neupane R, Fayezizadeh M, et al. POEM is a cost-effective procedure: cost-utility analysis of endoscopic and surgical treatment options in the management of achalasia. Surg Endosc 2017;31:1636-42. [Crossref] [PubMed]
- Greenleaf EK, Winder JS, Hollenbeak CS, et al. Cost-effectiveness of per oral endoscopic myotomy relative to laparoscopic Heller myotomy for the treatment of achalasia. Surg Endosc 2018;32:39-45. [Crossref] [PubMed]
Cite this article as: Kohn GP. Peroral endoscopic myotomy for achalasia—a review. Ann Laparosc Endosc Surg 2019;4:89.