
Twenty years experience of laparoscopic adrenal surgery in the west of Scotland
Introduction
The benefits of laparoscopic surgery are well known. Advantages such as reduced hospital stay, less post-operative pain and bleeding have led to laparoscopic adrenalectomy becoming the gold standard for the management of adrenal tumours (1-4). Most authors agree that benign, small or functional tumours can be managed laparoscopically but the evidence for the management of large, malignant tumours is lacking and most of the guidelines concerning the latter are based on consensus opinion (5).
Incidentalomas of the adrenal gland are found in 4–6% of patients undergoing cross sectional imaging and the increasing incidence has accounted for more patients undergoing surgery (6,7). Given the relative rarity of adrenal pathology requiring surgery, centralisation of endocrinology services can lead to better outcomes for patients but also increases the technical expertise of adrenal surgeons. The British Association of Endocrine and Thyroid Surgeons (BAETS) recommends that adrenal surgeons should perform a minimum of 6 adrenalectomies per year in order to maintain competencies and centralisation of services ensures that this is attainable (8).
The aim of the present study is to describe the experience of adrenal surgery in a tertiary referral centre in the west of Scotland with a particular emphasis on the feasibility of the laparoscopic approach, complication rates and to describe the trends over this time period.
Methods
Patients undergoing surgery for suspected adrenal tumours in a tertiary referral centre in the west of Scotland were retrospectively analysed from 1999–2018. The main indications for surgery were functionality, suspected malignancy based on radiological investigations or biopsy (primary adrenal cancers or metastases) or indeterminate lesions.
Demographic data collected included age, gender and date of operation. The characteristics of the tumour were also analysed. These included the size of the tumour, functionality and type of imaging used to detect the adrenal tumour. Tumour size was based on imaging rather than histology. Histology specimens were reviewed and the pathological diagnosis was recorded. For patients with metastatic disease to the adrenal gland, the site of the original primary tumour was also recorded.
Functionality was assessed using biochemical investigations. Evidence of catecholamine excess was assessed by measuring urinary and plasma metanephrines and normetanephrines. Low dose overnight dexamethasone suppression tests and 24 hr urinary cortisol were used to assess evidence of cortisol excess with plasma adrenocorticotrophic hormone (ACTH) measured to confirm/rule out Cushing’s disease. Plasma aldosterone and rennin were measured if aldosterone excess was suspected. Imaging techniques included computed tomography (CT), magnetic resonance imaging (MRI), adrenal vein sampling (AVS), positron emission tomography (PET) for patients with suspected metastatic disease and metaiodobenzylguanidine (MIBG) for patients with suspected extra-adrenal phaeochromocytomas/paragangliomas.
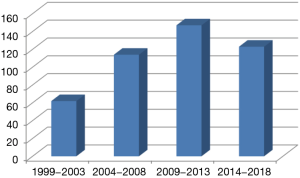
The surgical approach was also recorded—laparoscopic, converted or open. All laparoscopic procedures were transperitoneal using a standard 4 port technique. The study period was subdivided into 5-year blocks to observe the trend in the number of adrenalectomies performed. Intra and post-operative complications were recorded using the Clavien-Dindo classification system. All statistical analyses were performed using SPSS PASW version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Four hundred and forty-six patients were included in our analysis with 264 females and 182 males. Thirty-two patients had bilateral adrenalectomies with the remaining patients having unilateral adrenalectomies. The median age in this cohort was 55 (range, 15–77) years. The histological diagnoses are shown in Table 1. The indication for bilateral adrenalectomies is shown in Table 2.
Table 1
| Diagnosis | N=446 |
|---|---|
| Non-functioning adenoma | 80 |
| Phaeochromocytomas and paragangliomas | 126 |
| Conn’s syndrome | 57 |
| Cushing’s syndrome | 76 |
| Adrenocortical cancers | 31 |
| Metastases | 53 |
| Oncocytoma | 4 |
| Ganglioneuromas/Schwannomas | 7 |
| Miscellaneous (lymphoma/epithelial) | 12 |
Table 2
| Diagnosis | N=32 |
|---|---|
| Neuroblastoma | 1 |
| Phaeochromocytomas | 5 |
| Cushing’s disease/bilateral nodular hyperplasia | 20 |
| Adenomas | 3 |
| Paragangliomas | 1 |
| Metastases | 2 |
Overall, 91% (n=406) of patients had a laparoscopic adrenalectomy. Fifteen patients had an open approach and 25 patients (6%) were converted from a laparoscopic to an open approach. The main reasons for conversion were bleeding that could not be controlled laparoscopically or the need for multivisceral resection in patients with suspected locally invasive malignancies. Two patients required synchronous nephrectomies.
Of the 31 patients with adrenocortical cancers (ACC), 64% (n=20) were resected laparoscopically. The median size of the tumour was 80 [10–195] mm. Three patients had an open approach (2 tumours were large (180 and 105 mm), and the third patient had a locally invasive ACC. The remaining patients were converted from laparoscopic to open based on the size of the tumour and possible local invasion.
For patients with benign adenomas undergoing surgery, 96% (n=77) underwent a laparoscopic adrenalectomy with 2 patients requiring conversion due to bleeding. 98% of patients undergoing surgery for Cushing’s disease had a laparoscopic adrenalectomy with a median size of 45 [5–115] mm. All patients with a diagnosis of Conn’s syndrome were managed laparoscopically. The median size of an aldosterone producing adenoma was 20 [4–80] mm. With respect to phaeochromocytomas/paragangliomas, 87% (n=110) of patients had a laparoscopic resection with 4 patients requiring an open resection and 12 patients converted from laparoscopic to open. The median size of the adrenal phaeochromocytomas was 50 [5–450] mm.
Outcomes of metastatic adrenal tumours were previously published from the current database. An analysis was done of 42 patients with metastatic disease to the adrenal gland (database currently has 53 patients). Thirty-eight patients (91%) had a complete laparoscopic resection of their metastatic deposit with 3 patients requiring conversion to open. The most common pathology encountered was metastases from renal cell cancers followed by lung, skin (malignant melanoma) and breast cancers. The median survival in the overall cohort was 56 months.
The number of adrenalectomies performed over the 20-year period were recorded. There was a trend toward increasing number of adrenalectomies performed over this period with a significant increase occurring after 2005 (Figure 1).
Data concerning complication rates were obtained electronically using patient notes. This was only available after 2009 and therefore complication data was only available for 272 patients. The overall complication rate for this cohort(n=272) was 16% (n=45). Seventy one percent (n=32) of these patients were graded as Clavien-Dindo I and II. 6 patients were graded as Clavien-Dindo III requiring surgical, endoscopic and radiological intervention. Seven patients were graded as Clavien-Dindo IV requiring intensive care support for single organ dysfunction.
Discussion
Adrenal surgery has evolved over the last few decades. Initially reserved for small, benign adrenal tumours, the laparoscopic approach has become the procedure of choice for the majority of patients with varying adrenal pathologies. This large retrospective study has demonstrated the feasibility and safety of laparoscopic adrenal surgery independent of tumour aetiology with low conversion and complication rates. With an increasing incidence of adrenalectomies being performed, it is apparent that centralisation of services will not only improve patient outcomes but also increase the technical expertise of surgeons.
The benefits of laparoscopic surgery are well known. With respect to adrenalectomies, several authors have reported that the laparoscopic approach is associated with less post-operative pain (9,10), less blood loss (11), shorter hospital stay (3,11) and quicker return to normal activities for small, benign tumours. In the present study, it was clear that the laparoscopic approach for both benign functioning and non-functioning tumours was feasible with low conversion rates. Higher conversion rates were seen in patients with phaeochromocytomas in the present study. Phaeochromocytomas tend to be larger functional tumours compared to cortisol and aldosterone producing adenomas and also tend to be more vascular (12). Given the larger size of the phaeochromocytomas and the possibility of malignancy, conversion should be considered for haemostasis control but also oncological clearance.
The role of laparoscopy for potentially malignant disease is less clear. The European Network for the Study of Adrenal Tumours (ENSAT) and European Society if Endocrine Surgeons (ESES) recommend that the open approach should be the surgical standard of care for confirmed ACC or suspicious tumours >6 cm (5). Despite this, several authors have reported that laparoscopic resection of suspected ACC can be performed once there is no evidence of local invasion and oncologic principles are adhered to (13-15). Two thirds of the patients with ACC in the current study had a laparoscopic adrenalectomy demonstrating the possibility of this approach in this cohort of patients. The initial size of the tumour was not a contraindication to the laparoscopic approach and the largest ACC to be removed laparoscopically was 195 mm with a median tumour size of 80 mm. Conversion to an open approach is warranted in patients with evidence of local invasion or en bloc resection is required in keeping with oncological principles.
There is a lack of evidence with regard to the surgical management of isolated metastases to the adrenal gland. Several authors have reported that laparoscopic adrenalectomy for isolated metastases was significantly associated with shorter hospital stay, less intra-operative blood loss and shorter recovery compared to the open approach, however there was no difference in resection margin or overall survival compared with open resection (16,17). The laparoscopic approach was achievable in the majority of patients with isolated metastases in the present cohort with acceptable survival outcomes (18). Although not offering a survival benefit compared to the open approach the short term benefits of laparoscopy makes it desirable in patients with isolated disease.
There has been a significant increase in the number of adrenalectomies being performed and with the centralisation of services, this had led to an improvement in outcomes for patients and low rates of complications but also increased the learning curve for surgeons. In our institution, the majority of adrenalectomies were performed or supervised by a single surgeon. With over 400 operations performed, this has led to high volume training of surgeons with a special interest in adrenal surgery. The learning curve for adrenal surgery is estimated at 20–40 cases (19-21) with the BAETS recommending a minimum of 6 cases per year to maintain competencies (8). Furthermore, Lindeman et al has reported that high volume adrenal surgeons, irrespective of specialty have lower complication rates and lower mortality compared to low volume surgeons (22). The low complication rates and lack of serious complications in the present study is testament to the experience and high volume at out institution.
Conclusions
Laparoscopic surgery is a feasible and safe approach for patients with adrenal tumour irrespective of the pathological diagnosis. It is associated with low conversion and complication rates. It requires a high level of expertise and should be performed by high volume surgeons in tertiary referral centres to improve outcomes and increase technical expertise.
Acknowledgments
The authors would like to acknowledge Professor O'Dwyer and his team at the Western Infirmary Glasgow whose series of adrenalectomies was the basis for this study. He has mentored many surgeons in this field passing on his knowledge and technical skills to ensure a high quality of care is delivered. We would also like to acknowledge the dedicated, hard-working staff of the Queen Elizabeth University Hospital for their commitment to the care of patients under their care.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.06.11). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). IRB and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Conzo G, Gambardella C, Candela G, et al. Single center experience with laparoscopic adrenalectomy on a large clinical series. BMC Surg 2018;18:2. [Crossref] [PubMed]
- Jacobs JK, Goldstein RE, Geer RJ. Laparoscopic adrenalectomy. A new standard of care. Ann Surg 1997;225:495-501. [Crossref] [PubMed]
- Lee J, El-Tamer M, Schifftner T, et al. Open and laparoscopic adrenalectomy: analysis of the National Surgical Quality Improvement Program. J Am Coll Surg 2008;206:953-9; discussion 959-61. [Crossref] [PubMed]
- Gagner M, Pomp A, Heniford BT, et al. Laparoscopic adrenalectomy: lessons learned from 100 consecutive procedures. Ann Surg 1997;226:238-46; discussion 246-7. [Crossref] [PubMed]
- Gaujoux S, Mihai R. European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg 2017;104:358-76. [Crossref] [PubMed]
- Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest. 2006;29:298-302. [Crossref] [PubMed]
- Song JH, Chaudry FS, Mayo-Smith WW. The incidental adrenal mass on CT: prevalence of adrenal disease in 1049 consecutive adrenal masses in patients with no known malignancy. AJR AM J Roentgenol 2008;190:1163-8. [Crossref] [PubMed]
- Palazzo F, Dickinson A, Phillips B, et al. Adrenal Surgery Practice Guidance for the UK. British Association of Endocrine and Thyroid Surgeons. 2016
- Wu CT, Chiang YJ, Chou CC. t al. Comparative study of laparoscopic and open adrenalectomy. Chang Gung Med J 2006;29:468-73. [PubMed]
- Barreca M, Presenti L, Renzi C, et al. Expectations and outcomes when moving from open to laparoscopic adrenalectomy: multivariate analysis. World J Surg 2003;27:223-8. [PubMed]
- Kwan TL, Lam CM, Yuen AW, et al. Adrenalectomy in Hong Kong: a critical review of adoption of laparoscopic approach. Am J Surg 2007;194:153-8. [Crossref] [PubMed]
- Kim AW, Quiros RM, Maxhimer JB, et al. Outcome of laparoscopic adrenalectomy for pheochromocytomas vs aldosteronomas. Arch Surg 2004;139:526-9; discussion 529-31. [Crossref] [PubMed]
- Nocca D, Aggarwal R, Mathieu A, et al. Laparoscopic surgery and corticoadrenalomas. Surg Endosc 2007;21:1373-6. [Crossref] [PubMed]
- Porpiglia F, Miller BS, Manfredi M, et al. A debate on laparoscopic versus open adrenalectomy for adrenocortical carcinoma. Horm Cancer 2011;2:372-7. [Crossref] [PubMed]
- Brix D, Allolio B, Fenske W, et al. Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: Surgical and oncologic outcome in 152 patients. Eur Urol 2010;58:609-15. [Crossref] [PubMed]
- Strong VE, D'Angelica M, Tang L, et al. Laparoscopic adrenalectomy for isolated adrenal metastasis. Ann. Surg. Oncol 2007;14:3392-400. [Crossref] [PubMed]
- Adler JT, Mack E, Chen H. Equal oncologic results for laparoscopic and open resection of adrenal metastases. J Surg Res 2007;140:159-64. [Crossref] [PubMed]
- Ramsingh J, O’Dwyer PJ, Watson CM. Survival outcomes following adrenalectomy for isolated metastases to the adrenal gland. Eur J Surg Oncol 2019;45:631-4. [Crossref] [PubMed]
- Henry JF, Defechereux T, Raffaelli M, et al. Complications of laparoscopic adrenalectomy: results of 169 consecutive procedures. World J Surg 2000;24:1342-6. [Crossref] [PubMed]
- Goitein D, Mintz Y, Gross D, et al. Laparoscopic adrenalectomy: ascending the learning curve. Surg Endosc 2004;18:771-3. [Crossref] [PubMed]
- Barczyński M, Konturek A, Gołkowski F, et al. Posterior retroperitoneoscopic adrenalectomy: a comparison between the initial experience in the invention phase and introductory phase of the new surgical technique. World J Surg 2007;31:65-71. [Crossref] [PubMed]
- Lindeman B, Hashimoto DA, Bababekov YJ, et al. Fifteen years of adrenalectomies: impact of specialty training and operative volume. Surgery 2018;163:150-6. [Crossref] [PubMed]
Cite this article as: Ramsingh J, Casey H, Watson C. Twenty years experience of laparoscopic adrenal surgery in the west of Scotland. Ann Laparosc Endosc Surg 2019;4:64.


