
Laparoscopic cholecystectomy: semi-top-down technique
Introduction
Gallbladder disease is one of the most common reasons patients are referred to a general surgeon. It is estimated that around 20 million people in the United States have gallstones corresponding to roughly 700,000 cholecystectomy procedures performed each year (1-5). The laparoscopic approach to this procedure has been the mainstay since the 1990s (6). Laparoscopy has dramatically improved postoperative recovery, and rates of bile duct injuries are low (0.5%) (7). However, a 0.5% injury rate corresponds to 3,500 bile duct injuries a year and almost half of all surgeons will experience a bile duct injury during their career (4). In addition, bile duct injuries result in significant morbidity and mortality. Specifically, bile duct injuries are associated with almost a three times higher risk of mortality (8). Despite decades of laparoscopic experience, evidence suggests that the rate of bile duct injury for laparoscopic cholecystectomy continues to be double that of an open procedure (7).
Error traps
Strasberg et al. (9) described four types of error traps when performing a cholecystectomy:
- Infundibular view error trap;
- Fundus-down error trap;
- Failure to perceive an aberrant right hepatic duct on cholangiography;
- Parallel union of the cystic duct.
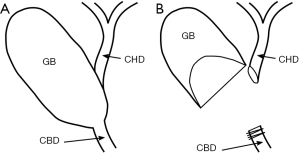
Infundibular view error trap
The infundibular view error trap is new since the development of laparoscopy. It typically occurs in the setting of inflammation and/or scarring and results in difficultly visualizing the structures within the hepatocystic triangle (9). When the hepatocystic triangle is contracted the wall of the gallbladder can fuse with the common hepatic duct. In these settings the infundibular-first technique can result in circumferential dissection of the common bile duct instead of the cystic duct (Figure 1A). When the common bile duct is mistaken for the cystic duct, it results in ligation of the common bile duct and transection of the common hepatic duct as the gallbladder neck is being dissected off of the liver bed (Figure 1B).
Fundus-down error trap
The fundus-down error trap typically occurs when a difficult gallbladder is converted to open. Injuries occur because the gallbladder fuses with the portal structures and the proximal portion of the gallbladder can be difficult to delineate. When the portal structures are confused for the gallbladder wall it results in serious biliary and vascular injuries (9). This is particularly important to note because the worst injuries often occur after conversion to an open procedure (4).
Failure to perceive aberrant anatomy on cholangiography
Aberrant right or right posterior hepatic ducts (RPHD) can also lead to error traps that are particularly prone to injury during an infundibular-first approach. In particular, RPHD that drain into the cystic duct, gallbladder neck, or common hepatic duct are problematic (Figure 2). These anatomic variants can occur in up to 3% of patients (10,11). They can be difficult to identify and injury may be unavoidable with the infundibular-first approach. In addition, the failure to identify an aberrant right hepatic duct on cholangiogram is an error trap. In some cases the absence of aberrant anatomy can be difficult for both surgeons and radiologist to identify. Failure to identify an injury on cholangiogram results in a delay in recognition and negatively effects patient outcomes (12).

Parallel union cystic duct
The final error trap is the parallel union cystic duct. There are three common configurations as that the cystic duct joins the common bile duct: 75% enter at an angle, 20% run parallel, and 5% spiral around the common bile duct (9). In both open and laparoscopic cholecystectomy the parallel union of the cystic duct is prone to electrocautery injury to the wall of the common bile duct.
There are many techniques available to aid surgeons in avoiding unwanted injuries and can be split into identification techniques and operative dissection techniques.
Identification techniques
There are four main identification techniques that can be used to help identify structures:
- Intraoperative cholangiogram (IOC);
- Critical view of safety;
- Fluorescent imaging;
- Intraoperative ultrasound.
Intraoperative cholangiogram
IOC can be a useful tool to identify anatomy as well as early recognition of an injury. However, there is still no clear answer as to whether routine IOC is beneficial or cost effective (4). Part of this debate stems from the fact that IOC is dependent on appropriate technique and interpretation.
Critical view of safety
The critical view of safety is typically paired with the fundus-first approach to avoid injury. To obtain a critical view of safety, the proximal 1/3 of the gallbladder must be dissected off the liver, the hepatocystic triangle must be widely cleared, and only two structures remain heading to the gallbladder (13,14). Even though the critical view of safety is an effective tool, retrospective studies have shown that surgeons meet the criteria in a minority of cases (15,16).
Fluorescent imaging
Fluorescent intraoperative cholangiography has been available since 2009 and has benefits when compared to IOC. Fluorescence has a lower setup time and eliminates radiation exposure to both the patient and staff (17). In addition, fluorescence does not require the placement of a cholangiocatheter and thus can avoid a catheter related bile duct injury (18). Although, studies have demonstrated that fluorescent imaging is safe and has promise, studies have not been large enough to show reduction in biliary injury (5).
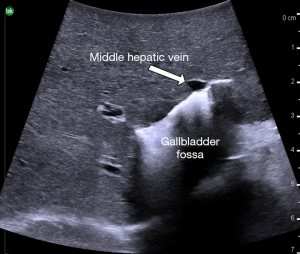
Intraoperative ultrasound
Intraoperative ultrasound is another tool available for both open and laparoscopic cases. Ultrasound can aid in defining anatomy (19,20), identifying common bile duct stones (21,22), and locating the proximity of the middle hepatic vein to the gallbladder (a common cause for massive bleeding during cholecystectomy) (23-25). An intraoperative ultrasound showing a close association of the middle hepatic vein and gallbladder fossa is shown in Figure 3. However, the use of ultrasound can be difficult and has a learning curve to be used effectively (26,27).
Operative dissection techniques
There are two main operative techniques when approaching a cholecystectomy and a third novel technique that will be described in more detail:
- Infundibular-first technique;
- Top-down (fundus-first);
- Semi-top-down technique.
Infundibular-first approach
The infundibular-first technique is the classic approach to a laparoscopic cholecystectomy. A top down approach can be performed laparoscopically but results in a mobile fundus that makes visualization and retraction difficult. This is the main reason the infundibular-first approach gained popularity. Dissection with this technique begins at the infundibulum and relies on upward retraction of the gallbladder fundus and lateral retraction of the infundibulum. The lateral retraction of the infundibulum helps pull the cystic duct closer to a 90° angle to the common bile duct making dissection easier. Although this technique works in the majority of cases it is prone to error trapping in certain circumstances as described above.
Top-down approach
The top-down approach to a cholecystectomy is the most common approach to an open cholecystectomy. Although this approach can be performed laparoscopically, it tends to be difficult due to the fundus of the gallbladder limiting visualization. The top-down approach is safe and can be thought of an exaggerated critical view of safety. However, it is also prone to error traps in severe inflammation as described above.
Proposed technique: the semi-top-down approach (Figure 4)

The patient should be positioned supine with arms out and a foot-board in place if steep reverse Trendelenburg is anticipated. After the patient is prepped and timeout is performed, four trochars are placed depending on surgeon preference for entry and position. A high resolution 30° or 45° scope should be used to aid in visualization. It is important to identify anatomic landmarks prior to starting dissection. This includes Rouviere’s sulcus (where the right posterior portal pedicle is located), the common bile duct, and the gallbladder infundibulum.
In contrast to the infundibular-first approach, the semi-top-down technique starts well above the infundibulum. The peritoneum is scored and dissection is directed laterally and to the side of the gallbladder. Once the lateral peritoneum is open, dissection is carried over-top of the infundibulum and along the medial aspect of the gallbladder. After the peritoneum is circumferentially opened the gallbladder is dissected off of the liver bed with a combination of blunt and electrocautery. Dissection continues until 1/3 to 1/2 of the proximal gallbladder is free from the liver. Unlike a top-down technique, the fundus of the gallbladder is kept attached to the liver to keep it out of the dissection field. The remaining dissection of the hepatocystic triangle mimics that of a top-down technique; approach to the infundibulum/cystic duct junction and the portal structures is with wide exposure and proceeding from the body of the gallbladder toward the porta hepatis. Dissection is carried out until two structures are entering the gallbladder and thus obtaining an exaggerated critical view of safety. The cystic artery and duct are clipped and cut separately. The remaining gallbladder is detached from the liver and removed in an endocatch bag.
Conclusions
The semi-top-down technique to a laparoscopic cholecystectomy has the visual advantages of an infundibular-first approach and the safety advantages of a top-down approach. Thus, it utilizes the advantages while eliminating the disadvantages of both techniques.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.06.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hassler K, Jones M. Laparoscopic Cholecystectomy. StatPearls Publishing; 2019.
- Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep 2005;7:132-40. [Crossref] [PubMed]
- Strosberg DS, Nguyen M, Muscarella P, et al. A retrospective comparison of robotic cholecystectomy versus laparoscopic cholecystectomy: operative outcomes and cost analysis. Surg Endosc 2017;31:1436-41. [Crossref] [PubMed]
- Peitzman AB, Watson G, Marsh J. Acute cholecystitis. J Trauma Acute Care Surg 2015;78:1-12. [Crossref] [PubMed]
- Pesce A, Piccolo G, La Greca G, et al. Utility of fluorescent cholangiography during laparoscopic cholecystectomy: A systematic review. World J Gastroenterol 2015;21:7877-83. [Crossref] [PubMed]
- Kapoor T, Wrenn S, Callas P, et al. Cost Analysis and Supply Utilization of Laparoscopic Cholecystectomy. Minim Invasive Surg 2018;2018:7838103 [Crossref] [PubMed]
- Ausania F, Holmes L, Ausania F, et al. Intraoperative cholangiography in the laparoscopic cholecystectomy era: why are we still debating? Surg Endosc 2012;26:1193-200. [Crossref] [PubMed]
- Flum DR, Cheadle A, Prela C, et al. Bile Duct Injury During Cholecystectomy and Survival in Medicare Beneficiaries. JAMA 2003;290:2168-73. [Crossref] [PubMed]
- Strasberg SM, Brunt LM. Rationale and Use of the Critical View of Safety in Laparoscopic Cholecystectomy. J Am Coll Surg 2010;211:132-8. [Crossref] [PubMed]
- Sofi AA, Alaradi OH, Abouljoud M, et al. Aberrant right hepatic duct draining into the cystic duct: clinical outcomes and management. Gastroenterol Res Pract 2011;2011:458915 [Crossref] [PubMed]
- Sarawagi R, Sundar S, Gupta S, et al. Anatomical Variations of Cystic Ducts in Magnetic Resonance Cholangiopancreatography and Clinical Implications. Radiol Res Pract 2016;2016:3021484 [Crossref] [PubMed]
- Connor S, Garden O. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg 2006;93:158-68. [Crossref] [PubMed]
- Abdalla S, Pierre S, Ellis H. Calot’s triangle. Clin Anat 2013;26:493-501. [Crossref] [PubMed]
- Vettoretto N, Saronni C, Harbi A, et al. Critical view of safety during laparoscopic cholecystectomy. JSLS 2011;15:322-5. [Crossref] [PubMed]
- Yamashita Y, Kimura T, Matsumoto S. A safe laparoscopic cholecystectomy depends upon the establishment of a critical view of safety. Surg Today 2010;40:507-13. [Crossref] [PubMed]
- Nijssen MA, Schreinemakers JM, Meyer Z, et al. Complications After Laparoscopic Cholecystectomy: A Video Evaluation Study of Whether the Critical View of Safety was Reached. World J Surg 2015;39:1798-803. [Crossref] [PubMed]
- Ishizawa T, Bandai Y, Kokudo N. Fluorescent Cholangiography Using Indocyanine Green for Laparoscopic Cholecystectomy: An Initial Experience. Arch Surg 2009;144:381. [Crossref] [PubMed]
- White TT, Hart MJ. Cholangiography and small duct injury. Am J Surg 1985;149:640-3. [Crossref] [PubMed]
- Birth M, Ehlers K, Delinikolas K, et al. Prospective randomized comparison of laparoscopic ultrasonography using a flexible-tip ultrasound probe and intraoperative dynamic cholangiography during laparoscopic cholecystectomy. Surg Endosc 1998;12:30-6. [Crossref] [PubMed]
- Yamashita Y, Kurohiji T, Hayashi J, et al. Intraoperative ultrasonography during laparoscopic cholecystectomy. Surg Laparosc Endosc 1993;3:167-71. [PubMed]
- Catheline J, Rizk N, Champault G. A comparison of laparoscopic ultrasound versus cholangiography in the evaluation of the biliary tree during laparoscopic cholecystectomy. Eur J Ultrasound 1999;10:1-9. [Crossref] [PubMed]
- Machi J, Oishi AJ, Tajiri T, et al. Routine laparoscopic ultrasound can significantly reduce the need for selective intraoperative cholangiography during cholecystectomy. Surg Endosc 2007;21:270-4. [Crossref] [PubMed]
- Ball CG, Maclean AR, Kirkpatrick AW, et al. Hepatic Vein Injury During Laparoscopic Cholecystectomy: The Unappreciated Proximity of the Middle Hepatic Vein to the Gallbladder Bed. J Gastrointest Surg 2006;10:1151-5. [Crossref] [PubMed]
- Shen BY, Li HW, Chen M, et al. Color Doppler ultrasonographic assessment of the risk of injury to major branch of the middle hepatic vein during laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int 2003;2:126-30. [PubMed]
- Misawa T, Koike M, Suzuki K, et al. Ultrasonographic assessment of the risk of injury to branches of the middle hepatic vein during laparoscopic cholecystectomy. Am J Surg 1999;178:418-21. [Crossref] [PubMed]
- Falcone RA Jr, Fegelman EJ, Nussbaum MS, et al. A prospective comparison of laparoscopic ultrasound vs intraoperative cholangiogram during laparoscopic cholecystectomy. Surg Endosc 1999;13:784-8. [Crossref] [PubMed]
- Barteau JA, Castro D, Arregui ME, et al. A comparison of intraoperative ultrasound versus cholangiography in the evaluation of the common bile duct during laparoscopic cholecystectomy. Surg Endosc 1995;9:490-6. [Crossref] [PubMed]
- Handzel RM, Peitzman AB. Laparoscopic semi-top-down cholecystectomy. Asvide 2019;6:181. Available online: http://www.asvide.com/article/view/32375
Cite this article as: Handzel RM, Peitzman AB. Laparoscopic cholecystectomy: semi-top-down technique. Ann Laparosc Endosc Surg 2019;4:60.


