
What is the added value of intraoperative indocyanine-green in right colectomy for cancer?
Introduction
Indocyanine-green (ICG) fluorescence imaging is an emerging technology utilized for intraoperative decision-making. In the last few years, the use of fluorescence to enhance visualization during open and laparoscopic surgery has been widely investigated in different surgical procedures. When the ICG is injected intravenously, it binds the plasmatic lipoproteins and gives information on the organ’s perfusion and vascular anatomy; when injected directly into the tissue, it follows the lymphatic drainage helping the surgeon to identify the lymphatic pathway. So, the possible use of ICG during right hemicolectomy are different: perfusion control, identification of embryological planes and control of lymphatic drainage.
Perfusion control
Regardless improvement in laparoscopic skills and the surgical techniques, anastomotic leak rate in colorectal surgery might varies between 3% and 20% (1). Several factors might influence the good healing of gastrointestinal anastomosis but, among them, several studies demonstrated that adequate blood supply is essential (2). Although several techniques have been proposed, bowel perfusion is usually done by surgeons’ subjective evaluation of the color of the serosa or the pulsation of marginal arteries (3). Fluorescence angiography, performed by injecting few cc of a well-known fluorophore called ICG allow to perform a real time, intraoperative angiography that confirm or not the perfusion of the segment of bowel to be anastomosed (4).
The operative protocol might vary according to surgeons’ preferences but in general, once completed the colectomy, just before fashioning the anastomosis, intravenous injection of 3 mL diluted ICG at a concentration of 0.2 mg/kg is carried out and, usually after 20–30 seconds (depending form the patient’s blood pressure and cardiac output) switching the camera to a near-infra-red (NIR) light, fluorescent perfusion of the bowel is confirmed and the exact colic margins where a good blood supply is present can be precisely estimated. Although most of the published studies focused on left hemicolectomy and rectal resection all demonstrated the usefulness of this technique with a percentage of change in resection margin around 5–7% as well reduction in the overall leak rate (5,6).
Identification of embryological planes
Recently, a new concept of the mesentery as a separate “organ” with its own lymphatic and a vascular watershed area has been introduced by Keller et al. (7). This anatomical concept has its surgical contra part with the complete mesocolic excision (CME) as treatment for right colon cancer proposed by Hohenberger et al. (8). Nevertheless, the routine used of CME is controversial as well as technically demanding. Recently Keller et al. (7) proposed the use of fluorescence to enhance the identification of the mesenteric plane by injecting 1 mL of ICG (concentration 5 mg/10 mL) into the subserosa layer of the colon waiting for ICG to spread into the mesentery to help surgeons to define the embryological planes. This concept has been also investigated in gastric cancer where endoscopic injection of ICG the day before surgery can help during the lymphadenectomy to define the mesogastric area. While in gastric cancer surgery results seems promising (9), in colorectal surgery this is still experimental.
Control of lymphatic drainage
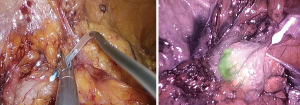
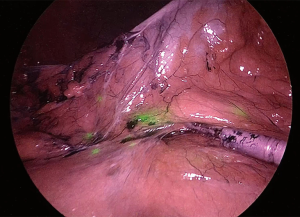
Opposite to the concept of CME, especially in case of early stage cancers (T1-2) where lymph node metastases are less frequent, lymphatic mapping/drainage of the area around the tumor can also be evaluated using intra-operative laparoscopic or endoscopic injection of ICG. After few minutes from the injection, ICG will be drained by the local lymphatic defining fluorescent lymphatic route and the lymphatic “basin” for this specific tumor/patient.
This technique has been proposed also in case of early gastric cancer with extremely interesting preliminary results (9) to perform a “selective” rather than an extensive and complex lymphadenectomy (10).
In colorectal surgery the “lymphatic basin” theory should be considered as in its infancy and to be used in course of clinical trial to prove its oncological value. In this case, at the beginning of the procedure, the tumor is localized and minimal mobilization of the colon is performed. At this point, using a fine needle 3 cc of ICG are injected in subserosal layer, paying attention to avoid accidentally spillage of the fluorophore. After few minutes by switching to NIR light the lymphatics as well as the lymph nodes, draining from that area will became evident allowing to identify the lymphatic route and, in theory, to customize the lymphadenectomy (Figures 1,2).
Discussion
This paper highlights that ICG fluorescent use has possible applications in general surgery procedures and in particular during right hemicolectomy: control of tissue perfusion and vascular anatomy and evaluation of lymphatic draining pathway. Fluorescence-guided surgery is an innovative way of integration between surgery and images, providing better surgical and oncological results.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Roberto Bergamaschi and Mahir Gachabayov) for the series “Right Colon Cancer Surgery: Current State” published in Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.05.09). The series “Right Colon Cancer Surgery: Current State” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McDermott FD, Heeney A, Kelly ME, et al. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 2015;102:462-79. [Crossref] [PubMed]
-
Intestinal Anastomosis - James DR, Ris F, Yeung TM, et al. Fluorescence angiography in laparoscopic low rectal and anorectal anastomoses with pinpoint perfusion imaging--a critical appraisal with specific focus on leak risk reduction. Colorectal Dis 2015;17:16-21. [Crossref] [PubMed]
- Yoneya S, Saito T, Komatsu Y, et al. Binding properties of indocyanine green in human blood. Invest Ophthalmol Vis Sci 1998;39:1286-90. [PubMed]
- Nishigori N, Koyama F, Nakagawa T, et al. Visualization of Lymph/Blood Flow in Laparoscopic Colorectal Cancer Surgery by ICG Fluorescence Imaging (Lap-IGFI). Ann Surg Oncol 2016;23:S266-74. [Crossref] [PubMed]
- Mangano A, Fernandes E, Gheza F, et al. Near-Infrared Indocyanine Green-Enhanced Fluorescence and Evaluation of the Bowel Microperfusion During Robotic Colorectal Surgery: a Retrospective Original Paper. Surg Technol Int 2019;34:93-100. [PubMed]
- Keller DS, Joshi HM, Rodriguez-Justo M, et al. Using fluorescence lymphangiography to define the ileocolic mesentery: proof of concept for the watershed area using real-time imaging. Tech Coloproctol 2017;21:757-60. [Crossref] [PubMed]
- Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis 2009;11:354-64; discussion 364-5. [Crossref] [PubMed]
- Kwon IG, Son T, Kim HI, et al. Fluorescent Lymphography-Guided Lymphadenectomy During Robotic Radical Gastrectomy for Gastric Cancer. JAMA Surg 2018; [Epub ahead of print]. [PubMed]
- Watanabe J, Ishibe A, Suwa Y, et al. Real-Time Indocyanine Green Fluorescence Imaging-Guided Laparoscopic Right Hemicolectomy in Hepatic Flexural Colon Cancer. Dis Colon Rectum 2018;61:1333-4. [Crossref] [PubMed]
Cite this article as: Macina S, Boni L, Della Porta M, Baldari L, Cassinotti E. What is the added value of intraoperative indocyanine-green in right colectomy for cancer? Ann Laparosc Endosc Surg 2019;4:52.


