Laparoscopic treatment of obstructive right colon cancer
Despite the rapid expansion of minimally invasive surgery worldwide and the growing experience in the laparoscopic management of colon cancer high-quality studies on obstructing right colon cancer (RCC) are still lacking. The most recent meta-analysis of Cirocchi et al. attempted to shed a light in this field showing no difference in primary outcome—mortality (0.2% vs. 5.6%) and anastomotic leak (0% vs. 1.9%) and better secondary outcome (overall complication rate, length of incision, blood loss, hospital stay and early mobilization) (1). Despite the promising finding, however, this meta-analysis has several methodological issues and we completely agree with the critical remarks of Kwak et al. that the results should be interpreted with a caution (2). In fact, the meta-analysis includes only two studies with 78 patients and does not have enough statistical power, all studies are retrospective with a high risk for selection and publication bias. Recently, Jackson et al. critically addressed the assumption that meta-analysis increase the statistical power (3).
The problem is additionally complicated by the inherent difficulties to perform RCTs in emergency setting, including difficult randomization, various expertise of the attending surgeon, the frequently unstable general condition of the patients which preclude prolonged and technically tricky interventions. The rarity of the obstructing RCC (only 4% of all right-sided cancers) additionally hampers the recruitment of enough cases (4).
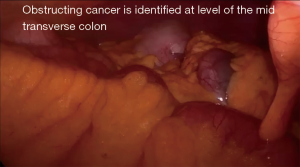
The oncological principles of resection should be applied even in emergency setting. This, however, although is feasible in experienced hands (Figure 1) (5), may not always be possible in obstructing RCC due to technical reasons such as the limited working space, different skills of the surgeons on call and frequently unstable general condition of the patients. Nowadays, it is well established fact that complete mesocolic excision (CME) improves the outcome in stage III cancers (decreased local recurrences—from 15% to 4%, and 5-year survival from 62% to 81%) (6), which is confirmed by a recent meta-analysis—HR 0.33 for 5-year survival (7). It is important to note, however, that CME is technically tricky procedure associated with a prolonged operative time (mean duration of 178 min) (8) and significantly more complications (RR 1.23) even in elective surgery (7), which could make its use in obstructing RCC questionable.
Therefore, all efforts to stabilize the patients and to resolve the obstruction are highly advisable. Similar to the combat practice, the mastery of surgery includes not only good technical skills but also an ability to choose the right tactic in the right patient. In their comment, Kwak et al. gave an excellent brief overview of the benefits of self-expanded metal stents (SEMS) as a bridge to elective surgery in obstructing colon cancer (2). On the background of the contradictory results for SEMS placement in obstructive RCC, the authors cited two small retrospective recent studies comparing a total of 39 cases with SEMS vs. 74 cases underwent emergency surgery, reporting no differences in the long term overall survival on the background of an increased rate of laparoscopic resection (4,9). In the study of Ji et al. only 12% of emergency group underwent laparoscopic surgery vs. 93% in SEMS group (9), whereas Kye et al. reported 39% vs. 60% (4).
Finally, we agree with Kim et al., that despite the lack of rigorous evidence the laparoscopy could be useful initial step in selected cases (Figures 1,2) (10,11). A multicenter prospective online platform to recruit enough data and to achieve the best evidence based strategy in obstructing RCC is highly warranted.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.04.10). SDS serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Apr 2018 to Mar 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cirocchi R, Cesare Campanile F, Di Saverio S, et al. Laparoscopic versus open colectomy for obstructing right colon cancer: A systematic review and meta-analysis. J Visc Surg 2017;154:387-99. [Crossref] [PubMed]
- Kwak JM, Dallemagne B. Obstructive right colon cancer: towards an optimal patient-tailored treatment strategy. Ann Laparosc Endosc Surg 2018;3:13. [Crossref]
- Jackson D, Turner R. Power analysis for random-effects meta-analysis. Res Synth Methods 2017;8:290-302. [Crossref] [PubMed]
- Kye BH, Lee YS, Cho HM, et al. Comparison of Long-Term Outcomes Between Emergency Surgery and Bridge to Surgery for Malignant Obstruction in Right-Sided Colon Cancer: A Multicenter Retrospective Study. Ann Surg Oncol 2016;23:1867-74. [Crossref] [PubMed]
- Di Saverio S, Segalini E, Birindelli A, et al. Laparoscopic extended right and transverse colectomy with completely intracorporeal ileo-descending anastomosis for obstructing colon carcinoma - a video vignette. Colorectal Dis 2018;20:80-2. [Crossref] [PubMed]
- Merkel S, Weber K, Matzel KE, et al. Prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision. Br J Surg 2016;103:1220-9. [Crossref] [PubMed]
- Wang C, Gao Z, Shen K, et al. Safety, quality and effect of complete mesocolic excision vs non-complete mesocolic excision in patients with colon cancer: a systemic review and meta-analysis. Colorectal Dis 2017;19:962-72. [Crossref] [PubMed]
- Li H, He Y, Lin Z, et al. Laparoscopic caudal-to-cranial approach for radical lymph node dissection in right hemicolectomy. Langenbecks Arch Surg 2016;401:741-6. [Crossref] [PubMed]
- Ji WB, Kwak JM, Kang DW, et al. Clinical benefits and oncologic equivalence of self-expandable metallic stent insertion for right-sided malignant colonic obstruction. Surg Endosc 2017;31:153-8. [Crossref] [PubMed]
- Birindelli A, Segalini E, Kwan S, et al. Challenging emergency laparoscopic right colectomy for completely obstructing caecal carcinoma - a video vignette. Colorectal Dis 2017;19:504-6. [Crossref] [PubMed]
- Kim BR, Kim YW. Minimally invasive colon resection for obstructing right colon cancer. Ann Laparosc Endosc Surg 2018;3:11. [Crossref]
Cite this article as: Di Saverio S, Tabakov M, Cirocchi R, Popivanov G, Mutafchiyski V. Laparoscopic treatment of obstructive right colon cancer. Ann Laparosc Endosc Surg 2018;3:39.