
Laparoscopy in emergency hernia repair
Introduction
Minimal access surgery (MAS) has revolutionaries the world of surgery. Apart from the well-known early post-operative advantages, it has superior surgical view and maneuverability compare to open approach for pelvic floor surgery. Its long-term benefits are also important and have major impact to our health care system. The lower rate of bowel adhesion after MAS leads to less chance of adhesive bowel obstruction. Majority of small bowel adhesion requiring open surgery and adhesiolysis is result from previous open surgery. On the other hand, MAS has significantly less incisional hernia rate. Trocar site incisional hernia rate was commonly reported as <1% (1,2), compare to open surgery with incisional hernia rate of 12.6% in post-operative first year and 22.4% in 3 years for laparotomy wound (3). Some literature even reported incisional hernia rate as high as 36% after laparotomy and suggest the use of prophylactic onlay mesh during closure in the primary operation (4). The application of MAS was quickly expanded to emergency surgical conditions. Some common acute surgical conditions where laparoscopic approach is considered to be first line treatment include acute cholecystitis and acute appendicitis. In specialized center laparoscopic approach is also being employed for acute small and large bowel conditions (5-7). There is similar trend in hernia surgery. Laparoscopic treatment for emergency hernia conditions has been reported and proven to be safe and feasible in expert hand (8).
Groin hernia (including inguinal, femoral and obturator hernias) is a common condition that requires surgical treatment. Laparoscopic repair for elective groin hernia is a widely accepted approach with low morbidity and excellent long-term results. Transabdominal preperitoneal (TAPP) and totally extra-peritoneal (TEP) approaches are the two most accepted laparoscopic repair for groin hernias. While laparoscopic groin hernia repair has comparable results compared to open groin hernia repair (9-11), it has a unique advantage over open repair in its ability to detect any concurrent ipsilateral and contralateral hernias intra-operatively. The advantage of laparoscopic repair is even more significant in cases of pelvic floor hernias like femoral and obturator hernia, and bilateral groin hernia repair. The mesh placement in laparoscopic repair is superior to open approach since it covers all the potential hernia orifices including inguinal, femoral and obturator canal. Rapidly it gains popularity as a choice for elective groin hernia repair all over the world.
Strangulated hernia is one of the commonest causes of small bowel obstruction. For groin hernia the yearly strangulation risk is around 1–3% (12,13). These patients have a wide spectrum of presentation, ranging from painful groin lump to severe sepsis in case of ischemic perforated bowel. Traditional management for emergency groin hernia conditions involve open anterior repair. This involves making an incision over the hernia site; identify the hernia sac and open the sac followed by the assessment of the incarcerated content. If the incarcerated bowel or organ is not viable, then bowel resection is performed, either through the groin wound or via separate laparotomy wound. If the intra-peritoneal assessment is inadequate through the groin incision, laparotomy will also be performed (14,15). Incarcerated obturator hernia is often managed with laparotomy (16,17).
Most of these patients are elderly, strangulated hernia is associated with higher post-operative morbidity and mortality, particularly for those who required laparotomy, bowel resection, or those with late presentation who suffered from perforated bowel with peritoneal contamination (18). This is especially true for strangulated pelvic flood hernia like femoral or obturator hernia where most of the time it involves frail elderly lady with delayed presentation because of the occult position of the hernia site, leading to bowel ischemia at the time of diagnosis.
With the experience obtained in elective laparoscopic groin hernias repair, there is increasing confidence on both of the surgical technique and understanding of the pre-peritoneal anatomy. This together with the experience obtained from laparoscopic management for other surgical emergencies has led expert surgeons to perform laparoscopic treatment for emergency groin hernia conditions. It was first reported in 1993 by Watson et al. (19). They described the use of totally laparoscopic approach for hernia repair together with bowel resection.
There are clinical reports and comparative studies for laparoscopic treatment for emergency groin hernia from center specialized in laparoscopic hernia surgery. On the other hand, reported literature for laparoscopic repair for emergency ventral and incisional hernia is scarce.
Evidence
The evidence for elective laparoscopic groin hernia repair is well established. Compare to open repair, it has the advantages of accurate diagnosis of the involved hernia, detection of any concurrent ipsilateral and contralateral hernias, smaller wound with less pain, significant lower surgical site infection rate, faster recovery and superior mesh placement which allow coverage for all potential myopectineal orifices. On the other hand, there are only handfuls of literatures on the evidence of emergency laparoscopic groin hernia repairs. In 2009, Deeba et al. (8) reported their systematic review on laparoscopic approach to incarcerated and strangulated inguinal hernia.
They concluded that both TAPP and TEP were feasible with comparable overall rate of complications, hernia recurrence and hospital stay to those documented in open repair for strangulated hernia. The literatures analyzed in this systematic review were all case series (20-26). One of the limitations of this systematic review is the wide variation on the operative approaches in these case series, such that it is difficult for us to comprehend their result collectively. Within these series, there are differences in the approach for reduction of the strangulated content, subsequent management of the gangrenous strangulated content and how they define open conversion. For example, in Ferzli et al. series (20), they utilized TEP approach from the very beginning including the reduction of the strangulated content without any peritoneal laparoscopy. With this, one case resulted in injury to the caecum while opening up the sac. The relaxation incision described by Ferzli to aid the reduction of the strangulated content was meant to be used in the extra-peritoneal plane. They reported that there are three open conversions out of 11 cases. Yet one case involves resection of the omentum through an extended umbilical wound, another case involved small bowel resection because of gangrenous strangulated obturator hernia through an abdominal incision. However, in majority of other series, laparoscopic reduction of the strangulated content was usually performed trans-peritoneally. Also when bowel resection is required, extended subumbilical wound was not considered as open conversion. And in some series, gangrenous omentum resection could be done laparoscopically. Some series had also reported totally laparoscopic intra-corporeal bowel resection and anastomosis.
There is one retrospective study involving 27 patients having strangulated inguinal hernia, comparing on laparoscopic versus open tension-free repair by a Chinese group in 2015 (27). The author reported that laparoscopic group has shorter operative time; lower complication rates on seroma, haematoma, and wound infection; faster return of bowel function; and shorter hospital stay. However, this comparative study used biological mesh which is currently controversial for groin hernia repair.
Our group has reported a retrospective comparative study on open versus laparoscopic treatment for strangulated hernia (28). Altogether 188 patients were included, of which 57 received laparoscopic and 131 with open repair. In our series within the open group, 48% of the laparotomy was performed without the need for bowel resection which is similar to other literature (18). Bowel resection rate in laparoscopic group was 1.75% versus 7.63% in the open group. There was more surgical site infection in the open group (12 patients in open group versus 0 in laparoscopic group). Breakdown of the wound infection rate in open group showed groin wound infection rate was 6% and laparotomy wound infection rate was 21%. The hospital stay was longer in the open group although it was not statically significant.
It appears from all the available literature that the major benefits of laparoscopic treatment for emergency hernias are:
- Accurate diagnostic ability;
- The avoidance of laparotomy;
- Somehow the laparoscopic group has less rate of bowel resection;
- A lower wound infection rate in the laparoscopic group;
- Advantages in laparoscopic repair for pelvic floor hernia and bilateral hernias.
The benefit of inguinal hernia repair itself in laparoscopic group over open group may not be so significant in cases with strangulated hernia, as most of the time the delay in hospital discharge are related to bowel function like ileus and bowel anastomosis. These are, however, yet to be defined from future larger scale randomized control study. For emergency ventral and incisional hernia, the evidence for laparoscopic management is scarce.
From our experience gained from emergency hernia repair, it is apparent that each surgical step should be broken down and interprets independently in order to see the true laparoscopic value in each step and determine which patients benefit most from.
Difference in open and laparoscopic repair for emergency hernias
The difference between laparoscopic and open repair for emergency hernia surgery is not only about the size of the wound and wound related trauma. The surgical steps and sequence of events are different such that it has major contribution to the clinical outcome.
Surgical steps sequence
The surgical steps sequence in open surgery is different from laparoscopic approach, such it contributes to the benefit of laparoscopic approach.
In open surgery, after skin incision over the hernia site and identify the hernia sac, the sac is opened with or without widening of the hernia neck, allowing the release of the strangulated content. The content is then assessed for its viability. The next step is the decision for the need of bowel resection and if laparotomy is required. Both bowel resection and laparotomy are the major contributors for increased morbidity and mortality on emergency hernia surgery. If the assessment is inadequate through the hernia wound, laparotomy should be performed. Regarding bowel resection, the classical teaching is to use a warm saline pad to re-warm the strangulated bowel for 5 to 10 min to see the response. Since this is emergency condition and time is essence, it is very difficult for the surgeon to idle for 10–20 min trying to make a return on the bowel condition, so most of the time, surgeon would just proceed for bowel resection. For some cases the bowel ischemia may be potentially reversible. In contrary, surgical approach involves laparoscopy as described below; the time span for reassessment is often around 60 min.
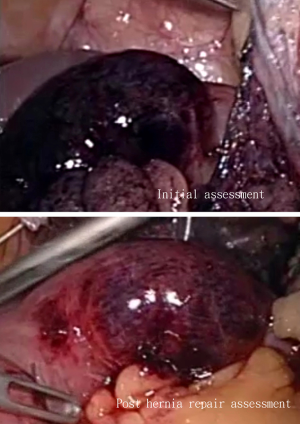
In laparoscopic approach, after identifying the hernia, the strangulated content is reduced. Initial assessment of the strangulated bowel is performed. Unless there is gangrenous perforation which requires control of the perforation first, the surgeon will proceed to hernia repair. After the reduction of the incarcerated or strangulated content, accurate diagnosis on the involved hernia is performed, together with the assessment on any concomitant ipsilateral and contralateral hernia. The hernia repaired comes next. It usually occupies the next 45 to 60 min. After the hernia repair, the surgeon will then come back for reassessment of the strangulated segment of bowel. This allow ample time for the strangulated bowel to recover, and this in fact will avoid unnecessary laparotomy and bowel resection as most of the time the strangulated bowel can recovered if we allow enough time for them to revascularize.
This is how the surgical steps sequence difference between open surgery versus laparoscopic surgery in emergency hernia influence on the rate of laparotomy and bowel resection. As Romain et al. (18) described, “The first intention exploratory laparotomy in strangulated hernia surgery was a major cause of post-operative complication”. One can start to see with the aid of diagnostic laparoscopy alone, it already made a difference in clinical post-operative outcome. It is therefore important in future clinical study to define accurately what it’s meant be laparoscopic approach, laparoscopy with laparoscopic repair of hernia or laparoscopy with open repair of hernia.
Patient selection and preoperative assessment
Patient selection and pre-operative planning is vital for every surgery to be successful. The surgeon, theater personnel and the center with available necessary equipment and instrument are all essential components for successful laparoscopic hernia repair, especially in emergency setting.
Those patients with peritonitis and free perforation on imaging study should be considered for open approach with emergency laparotomy. This also applies to those patients who are heamodynamically unstable as well.
If laparoscopic repair is contemplated for a patient with strangulated hernia, a pre-operative diagnostic contrast CT scan of the abdomen is desirable. The reason behind is that, despite the benefit of laparoscopy which can accurately assess the strangulated organs, the site of hernia and presences of any concurrent hernia, it is difficult for laparoscopy to fully assess the whole length of the small bowel. Unlike in laparotomy which the surgeon can run through the whole length of small bowel from duodenojejunal flexure to terminal ileum, it is often difficult to do so in laparoscopy because of the limited working space and oedematous distended bowel. Given the accuracy of CT scan nowadays, a pre-operative CT scan can help us to detect any double pathology that might occasionally occur. It is most important to discuss with the radiologist pre-operatively about the actual site of bowel obstruction in patient presented clinically with strangulated hernia. In order to avoid patient presented with incarcerated hernia but with obstruction further down caused by pathology like adhesion, volvulus or tumor. In which case reducing and repair the hernia will not relief the obstruction. If a different site of obstruction other than the hernia is suspected on CT scan, this should be looked for specifically during laparoscopy, and consider converting to open approach if there is any doubt.
Post-operative clinical assessment is also important in which if the obstruction or ileus does not resolve in a matter of days’ time, other underlying pathology should be sort for like delay perforation of bowel, or second obstruction pathology. Prolong clinical recovery should be a warning sign especially in elderly.
Laparoscopic repair for emergency hernia—technical aspect
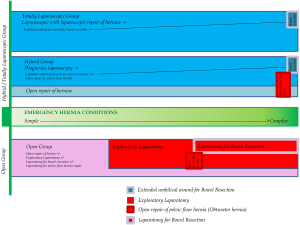
Laparoscopic approach can means anything, from using diagnostic laparoscopy and then open hernia repair to totally laparoscopic including the hernia repair and or bowel resection. As described later adding just diagnostic laparoscopy alone can make significant difference. For better definition and understanding, in the rest of the discussion we describe diagnostic laparoscopy followed by open hernia repair as “hybrid approach”, and diagnostic laparoscopy followed by laparoscopic repair of the hernia as “totally laparoscopic approach”.
Bowel resection can be performed either through an extended subumbilical port wound or intra-corporeally using endostapler. Both of these approaches for bowel resection created minimal stress to the patient so the difference in clinical outcome and recovery should be minimal.
Hybrid approach
This involves performing diagnostic laparoscopy via subumbilical wound first, identify the hernia, reduce the strangulated hernia content, and then proceed to open repair for the hernia in the usual manner. After the completion of open hernia repair, re-laparoscopy was performed again to reassess the strangulated segment of bowel for its viability. The decision on whether the strangulated bowel segment required resection will be decided at this time. If bowel resection is required, it is usually performed via an extended small subumbilical wound.
Totally laparoscopic approach
Totally laparoscopic approach differs in that the hernia repair is performed also laparoscopically. In case of groin hernia, either TEP or TAPP will be performed after diagnostic laparoscopy and the reduction of the strangulated content. After TEP or TAPP repair, re-laparoscopy will be performed again for reassessment of the strangulated bowel segment for its viability. If bowel resection is required, similar to above it can be performed via an extended subumbilical wound or totally laparoscopically with intra-corporeal bowel anastomosis.
Diagnostic laparoscopy in emergency hernia repair
Diagnostic laparoscopy provides us a clear understanding of what is involved in the strangulated hernia sac. This can ranged from omentum, small bowel, large bowel, bladder or appendix in rare cases. This does not only allow us to understand more about the spectrum of strangulated hernia presentation, it also provides the opportunity to record this in the form of image or video of some rare conditions. Such imaging and videos would be extremely valuable for hernia disease management and can be used for future academic and teaching purpose.
Reduction of the strangulated content
This is the single most crucial step in emergency hernia surgery. It determines whether the case can be managed laparoscopically or not, in both hybrid and totally laparoscopic approach. The chance of irreducibility laparoscopically and require full laparotomy conversion is rare in all the clinical reports.
When we refer to the fact that emergency hernia patients have a spectrum of presentation, in large this is what we meant. Some patient presented with easily reducible incarcerated hernia, some presented with horribly tightly strangulated hernia. Some presented with strangulated omentum which can be sacrificed, some presented with small bowel, large bowel or bladder strangulation which make subsequent surgical management more challenging. This factor largely influences the surgical approach and outcome of the patient presented with emergency hernia conditions.
For reduction of the strangulated content, we recommend to rely mainly on external compression for reduction using peritoneal laparoscopic guidance. With laparoscopy, we can accurately determine the direction of external compression to reduce the hernia. The external compression can itself reduce the oedema of the strangulated content, together with the pneumoperitoneum which strength the abdominal wall under general anesthesia relaxation, such that most of the hernias can be reduced in this way. Using laparoscopic instrument to grasp the bowel has to be very careful to avoid tearing the bowel loops. If laparoscopic grasping is needed, it is recommended to grasp the less important structures like omentum or peritoneal fat first. If further required, the distal collapsed bowel loop can be grasped gently while applying external pressure in the correct direction, the strangulated content should be reducible.
In one study, special technique on widening of the hernia ring to allow reduction of strangulated content is mentioned (20). This is however meant for TEP approach for the reduction of the strangulated content, not for peritoneal laparoscopic approach.
Once the strangulated content is uneventfully reduced, meaning that there is no injury to the content, the most difficult part of the surgery has been done and psychologically we are almost to the end of the operation already. Peritoneal laparoscopic reduction should allow safer reduction of the strangulated content. The surgeon has the time to decide on which method of hernia repair is to be used. It is therefore ultimately important to carefully execute the reduction of strangulated content without injury to both the strangulated content and surrounding important structures. If the content cannot be reduced despite various methods, there are two options. One can sacrifice the strangulated short small bowel segment by using Endo GIA to transect it completely and removed the strangulated stump and perform bowel anastomosis at the end of the operation, or convert to open repair. Fortunately in majority of the cases the reduction of content can be achieved. In reported literatures including ours, the chance of irreducibility intraoperatively requiring laparotomy is extremely rare. Also the chance of gangrenous bowel requiring resection is also low. This means in majority of the patients their strangulated hernia can be reduced uneventfully and does not require any resection.
Mesh placement/usage in emergency hernia repair
Using mesh in strangulated hernia was previously seen as a controversial issue. Gathering most of the available evidence, using mesh in strangulated hernia cases is safe unless in the ultimate extreme case where there is a perforation of bowel with heavy contamination in the mesh placement area. Doing TAPP or TEP, or open Lichtenstein repair, because the mesh is placed in the different plane, mesh infection rate in strangulated hernia is low. In our series (28) of 188 strangulated hernias, only 10 cases were done with tissue repair without using mesh. In the rest of the 178 cases, whether it was laparoscopic or open mesh repair, no case of mesh infection was recorded.
Pelvic floor hernia
Pelvic floor hernias include femoral and obturator hernia. It is not uncommon that these hernias occur as bilateral hernia. Open repair for obturator hernia requires laparotomy. Open repair for femoral hernia can be performed through different approaches, either anterior groin incision approach, or posterior approach such as McEvedy’s vertical incision or Lockwood incision. In femoral hernia, if the viability of the incarcerated bowel is in doubt, extension of the incision can be done either upward or transversely to enter the peritoneum via incising on the transversalis fascia for exploration laparotomy or bowel resection. Whichever approaches one used, it involve major incision on the abdominal wall and groin muscle which causes significant structural damage to the functional abdominal wall which in itself is one of the major causes for hernia formation.
MAS approach has several obvious advantages for emergency pelvic floor condition.
The diagnostic accuracy of laparoscopy is superior than open approach. It can accurately diagnose the type of hernia, whether it is femoral or obturator, with also the ability of detecting any presence of concurrent hernia in the ipsilateral and/or contralateral side. The laparoscopic operative view and its surgical maneuverability are also superior to that of open surgery in pelvis, even compare to laparotomy. This has been recognized by many surgeons operating in pelvic floor such as rectal surgery. Moreover, operation can also be performed on both sides via the same working ports in cases it is a bilateral disease. The pre-peritoneal mesh placement for pelvic floor hernia repair is also superior to that of open repair counterpart. Therefore MAS approach for pelvic floor hernias enjoy significant advantages while avoiding major abdominal incision and disruption of the abdominal wall architecture (29-34).
TEP or TAPP in groin hernia repair in emergency cases
There is no consensus on whether to perform TAPP or TEP for emergency strangulated groin hernia. However, after years of observation, many surgeons naturally prefer TEP approach after peritoneal laparoscopic reduction of the strangulated content, contrary to what we might believe initially as TAPP to be a more logical step after laparoscopic reduction of the strangulated hernia.
In TEP, the surgeon operates through a completely different surgical plane, outside the peritoneal cavity which house the distended obstructed bowel loop. With TEP approach, we do not need to make an incision on the peritoneum using sharp cutting instrument, and at the end of the repair we do not need to close the peritoneal flap with tack or sharp suture. During TEP the laparoscopic instrument go in and out in the pre-peritoneal plane only. Therefore operating through TEP avoids the risk of bowel injury as compared to TAPP, this is especially true in cases where bowel distension and obstruction is significant. Also working in different plane, TEP avoids any contamination from the peritoneal cavity with the protection of intact peritoneum, in case of gangrenous bowel with perforation and those required bowel resection.
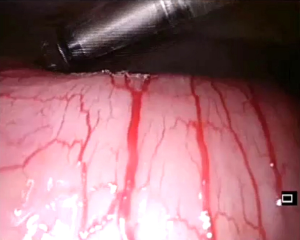
In TAPP, you need to incise the peritoneum with sharp cutting instruments to create the peritoneal flap. And during the surgery, the instruments go in and out through the peritoneal cavity. With the patient tilted, the bowel loops can move and lies in front of the working trocar ports (Figure 1). When placing the laparoscopic instruments in and out through the working ports, one can inadvertently cause injury or puncture the distended small bowel without realizing, especially when the instrument is a sharp cutting instrument. Not to mention at the end of the operation the surgeon will need to close the peritoneal flap. If suture is used for this step the sharp end of the suture needle again will post laceration risk to the dilated bowel loops in TAPP repair.
Laparoscopic emergency hernias repair requires high level of surgeon’s concentration and meticulous maneuver of each steps, includes inserting and withdrawing the instrument in and out of the working trocars. Thus with TEP working through the pre-peritoneal space, completely outside the peritoneal cavity, this can ease the tension of the surgeon and keep a peace of mind.
Reassessment laparoscopy
In both hybrid and totally laparoscopic approach for emergency hernias, reassessment laparoscopy is vital, and this is one of the key factors contribute to the improved clinical post-operative outcome. After repair of the involved hernia, with mesh or without mesh, the intra-peritoneal condition and the strangulated organ (e.g., bowel) should be reassessed carefully.
Peritoneal laparoscopy is vital in order to determine if there was any inadvertent injury to the bowel. In difficult situation or suspicious cases it would be advisable to insert a new gauze inside the peritoneal cavity and mop around the reduced strangulated bowel and/or the bowel loops involved in adhesiolysis to see if any bowel stained fluid is detected on the gauze which might indicate micro-perforation. Of course when placing instrument or gauze inside laparoscopically, at the end of the operation one has to make sure everything is accountable for with double correct instruments and gauze counts.
When it comes to the reassessment of the strangulated bowel, not only the color of the strangulated bowel loops is reassessed, but the improvement compare to the initial assessment, the integrity of the bowel wall, presence of any micro-perforation, pulsation of the supplying vessels at the mesenteric border, and its peristalsis all need to be taken into account to decide whether bowel resection is required (Figure 2). Through the laparoscope with clear and magnified view, we can appreciate the bowel wall integrity and its details much more clearly then open surgery. Surgeon’s threshold for bowel resection under laparoscopic view is increased. This may be the other factor that contributes to the lower bowel resection rate in the laparoscopic group, together with the longer waiting time for bowel to recover.
Bowel resection
Bowel resection can be done extra-corporeally through an extended subumbilical incision of approximately 3 cm size, or totally intra-corporeally using endostapler anastomosis. Majority of the surgeon will prefer extra-corporeal bowel resection and anastomosis through a small extended subumbilical wound. It is because we are dealing with obstructed bowel in emergency setting, intra-corporeal bowel resection and anastomosis using endostapler is not only time consuming, but also is done with limited operating space and running the risk of spillage of bowel content during enterotomy for staple anastomosis, not to mention the risk of using energy cutting instruments and sharp suture in the presence of distended obstructed bowel loops.
In both techniques, the wound difference is only marginal and both create only minimal stress to the patient therefore it would be difficult to demonstrate any difference in recovery and post-operative clinical course. Therefore for the speed of surgery and avoidance of any spillage of bowel content most surgeons will prefer extra-corporeal bowel resection anastomosis through a small extended subumbilical wound.
Laparoscopic management for emergency ventral and incisional hernias
In emergency ventral and incisional hernia, same as groin hernia patients, except there is an even greater heterogeneity in their presentation. The site and size of the hernias, the number of hernias, the presence of intestinal obstruction, the presence of bowel gangrene and perforation, their intraperitoneal condition, the patient’s abdomen build and size in relative to the hernia pathology, and also the patient’s underlying conditions, all of these contribute to the decision on the surgical approach.
Stringent patient’s selection is vital for the result of various surgical approach, including laparoscopy, laparoscopic reduction, and totally laparoscopic repair or laparotomy.
The technique of gaining access to the peritoneal cavity (first port placement) is vital in this condition, as often the bowel loops are dilated. Using Veress needle blindly will pose higher risk of bowel injury, open Hasson technique is considered to be a safer approach by most surgeons. This first port position has to be well away from the hernia site, most appropriated at the right upper quadrant subcostal area where the liver is located, since accidental injuring the liver post less of a problem then injury the bowel. After laparoscopic assessment, attempt is to reduce the strangulated ventral hernia and incisional hernia. It is vital to identify correctly the strangulated segment of bowel among those adhesive bowel loops.
Reduction method can be totally laparoscopic or combined with the aid of small open incision over the strangulated hernia sac in case if laparoscopic view is limited to determine if there is any adhesion to prevent reduction of the hernia.
After reduction of the strangulated hernia, there are two options for repairing the ventral hernia: direct suture closure or mesh repair [intraperitoneal onlay mesh (IPOM) repair]. It can also be a staged repair where mesh repair can be performed as electively at later stage after direct suture repair. Most of the surgeons will probably opt for direct suture closure of the hernia defect because there is a hesitation in placing a large synthetic mesh inside the peritoneal cavity in acute abdominal condition with distended bowel loops. After all, there is always a risk of unforeseeable bowel injury during laparoscopic treatment for emergency ventral and incisional hernia, however small. One can always come back later for second stage elective mesh repair if consider necessary. This is especially true when the surgical field is contaminated by the gangrenous strangulated bowel with or without perforation, or if the patient is on peritoneal dialysis or with history of underlying malignant condition undergoing chemotherapy.
Decision on laparoscopic or open approach
The decision on laparoscopic or open surgical approach for emergency hernia conditions depends on: (I) the expertise of the surgeons and the center; (II) the benefits and risks of each technique in such emergency situation; (III) the patient’s hernia nature, their presentation and clinical status. Open conversion should always be kept in mind of the surgeon, according to the progress of surgery, the duration of the surgery, and the patient’s tolerance to pneumoperitoneum.
The post-operative clinical progress should be monitored closely.
Benefit of laparoscopic approach (hybrid or totally laparoscopic)
In summary, laparoscopic approach for emergency hernias repair has its benefits in several areas. Apart from the benefits of MAS, its advantages which contribute to the improvement in clinical outcome include:
- Superior diagnostic value;
- Detection of concurrent disease and bilateral disease with mesh placement able to cover all potential hernia orifices;
- Superiority in pelvic floor hernia repair such as obturator hernias;
- Lowering the rate of laparotomy;
- Lowering the rate of bowel resection;
- Reduction in wound infection rate.
As mentioned above, laparotomy and bowel resection are the major contributors to post-operative complications in emergency hernia surgery. Both hybrid and totally laparoscopic approaches can effectively lower the laparotomy rate and bowel resection rate simply because of the diagnostic accuracy and reversal sequence of the surgical steps compare to open surgery. In center with less available expertise, the hybrid approach may be easier to manage by most surgeons. Even for those who require bowel resection, a small extended umbilical incision has much lower stress and trauma to the patient compare to laparotomy. Totally laparoscopic approach has the further advantages in pelvic floor hernia repair and bilateral hernia repair. It is not difficult to understand the inverse relationship between laparoscopic approach and patient’s post-operative morbidity and mortality especially in frail elderly group. Figure 3 summarizes the comparative difference in open, hybrid, and totally laparoscopic approach for emergency hernia repair (Figure 3).
Future
Further investigation in the future including randomized study is needed in this important area of hernia surgery. It will be complex because of the diversity of patients’ hernia presentation, their background conditions, together with the diversity of surgical approaches employed in difference centers. The level of surgical expertise varies among different laparoscopic centers, and even within the same center between different surgeons. However, since emergency hernia is a common surgical disease, and often this involves frail elderly patients; any possibility of improvement in post-operative clinical outcome is worth pursuing of. It is important for clinical investigators to define in details what it’s meant by laparoscopic approach? Is it laparoscopy with laparoscopic hernia repair or laparoscopy with open hernia repair? Also the approaches for bowel resection or omental resection need to be carefully defined during the design of the study. Subgroup stratification into inguinal and pelvic floor hernia is also important to compare the result between totally laparoscopic against hybrid and open laparotomy approaches. These details are required to allow effective comparison between totally laparoscopic approach, hybrid approach and open approach. The result of the future investigations will have significant impact on the post-operative outcome for patients suffer from emergency hernia conditions.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Davide Lomanto and Anil Sharma) for the series “Inguinal Hernia Repair” published in Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.05.05). The series “Inguinal Hernia Repair” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bunting DM. Port-site hernia following laparoscopic cholecystectomy. JSLS 2010;14:490-7. [Crossref] [PubMed]
- Azurin DJ, Go LS, Arroyo LR, et al. Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental preexisting umbilical hernia. Am Surg 1995;61:718-20. [PubMed]
- Fink C, Baumann P, Wente MN, et al. Incisional hernia rate 3 years after midline laparotomy. Br J Surg 2014;101:51-4. [Crossref] [PubMed]
- Caro-Tarrago A, Olona Casas C, Jimenez Salido A, et al. Prevention of incisional hernia in midline laparotomy with an onlay mesh: a randomized clinical trial. World J Surg 2014;38:2223-30. [Crossref] [PubMed]
- Tsui C, Klein R, Garabrant M. Minimally invasive surgery: national trends in adoption and future direction for hospital strategy. Surg Endosc 2013;27:2253-7. [Crossref] [PubMed]
- Catena F, Di Saverio S, Kelly MD, et al. Bologna Guidelines for Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2010 Evidence-Based Guidelines of the World Society of Emergency Surgery. World J Emerg Surg 2011;6:5. [Crossref] [PubMed]
- Borzellino G, Tasselli S, Zerman G, et al. Laparoscopic approach to postoperative adhesive obstruction. Surg Endosc 2004;18:686-90. [Crossref] [PubMed]
- Deeba S, Purkayastha S, Paraskevas P, et al. Laparoscopic approach to incarcerated and strangulated inguinal hernias. JSLS 2009;13:327-31. [PubMed]
- Schmedt CG, Leibl BJ, Bittner R. Endoscopic inguinal hernia repair in comparison with Shouldice and Lichtenstein repair. A systematic review of randomized trials. Dig Surg 2002;19:511-7. [Crossref] [PubMed]
- Stoker DL, Spiegelhalter DJ, Singh R, et al. Laparoscopic versus open inguinal hernia repair: randomized prospective trial. Lancet 1994;343:1243-5. [Crossref] [PubMed]
- Tschudi JF, Wagner M, Klaiber C, et al. Randomized controlled trial of laparoscopic transabdominal preperitoneal hernioplasty vs Shouldice repair. Surg Endosc 2001;15:1263-6. [Crossref] [PubMed]
- Abramson JH, Gofin J, Hopp C, et al. The epidemiology of inguinal hernia. A survey in western Jerusalem. J Epidemiol Community Health 1978;32:59-67. [Crossref] [PubMed]
- Neuhauser D. Elective inguinal herniorrphaphy versus truss in the elderly. In: Bunker JP, Barnes BA, Mosteller F. editors. Cost, risk and benefits for surgery. New York: Oxford University Press, 1977:(223-39).
- Kulah B, Kulacoglu IH, Oruc MT, et al. Presentation and outcome of incarcerated external hernias in adults. Am J Surg 2001;181:101-4. [Crossref] [PubMed]
- Mauch J, Helbling C, Schlumpf R. Incarcerated and strangulated hernias--surgical approach and management. Swiss Surg 2000;6:28-31. [Crossref] [PubMed]
- Sinha SN, DeCosta AE. Obturator hernia. Aust N Z J Surg 1983;53:349-51. [Crossref] [PubMed]
- Lo CY, Lorentz TG, Lau PW. Obturator hernia presenting as small bowel obstruction. Am J Surg 1994;167:396-8. [Crossref] [PubMed]
- Romain B, Chemaly R, Meyer N, et al. Prognostic factors of postoperative morbidity and mortality in strangulated groin hernia. Hernia 2012;16:405-10. [Crossref] [PubMed]
- Watson SD, Saye W, Hollier PA. Combined laparoscopic incarcerated herniorrhaphy and small bowel resection. Surg Laparosc Endosc 1993;3:106-8. [PubMed]
- Ferzli G, Shapiro K, Chaudry G, et al. Laparoscopic extraperitoneal approach to acutely incarcerated inguinal hernia. Surg Endosc 2004;18:228-31. [Crossref] [PubMed]
- Saggar VR, Sarangi R. Endoscopically totally extraperitoneal repair of incarcerated inguinal hernia. Hernia 2005;9:120-4. [Crossref] [PubMed]
- Leibl BJ, Schmedt CG, Kraft K, et al. Laparoscopic transperitoneal hernia repair of incarcerated hernias: Is it feasible? Results of a prospective study. Surg Endosc 2001;15:1179-83. [Crossref] [PubMed]
- Ishihara T, Kubota K, Eda N, et al. Laparoscopic approach to incarcerated inguinal hernia. Surg Endosc 1996;10:1111-3. [Crossref] [PubMed]
- Rebuffat C, Galli A, Scalambra MS, et al. Laparoscopic repair of strangulated hernias. Surg Endosc 2006;20:131-4. [Crossref] [PubMed]
- Legnani GL, Rasini M, Pastori S, et al. Laparoscopic trans-peritoneal hernioplasty (TAPP) for the acute management of strangulated inguino-crural hernias: a report of nine cases. Hernia 2008;12:185-8. [Crossref] [PubMed]
- Mainik F, Flade-Kuthe R, Kuthe A. Total extraperitoneal endoscopic hernioplasty (TEP) in the treatment of incarcerated and irreponible inguinal and femoral hernias. Zentralbl Chir 2005;130:550-3. [Crossref] [PubMed]
- Song B, Liu D, Liu S, et al. Efficacy comparison of laparoscopic versus open tension-free hernia repair using biologic mesh for inguinal strangulated hernia. Zhonghua Wei Chang Wai Ke Za Zhi 2015;18:1088-91. [PubMed]
- Yang GP, Chan CT, Lai EC, et al. Laparoscopic versus open repair for strangulated groin hernias: 188 cases over 4 years. Asian J Endosc Surg 2012;5:131-7. [Crossref] [PubMed]
- Yau KK, Siu WT, Chau CH, et al. Laparoscopic management of incarcerated obturator hernia. Can J Surg 2005;48:76-7. [PubMed]
- Ng DC, Tung KL, Tang CN, et al. Fifteen-year experience in managing obturator hernia: from open to laparoscopic approach. Hernia 2014;18:381-6. [Crossref] [PubMed]
- Tschudi J, Wagner M, Klaiber C. Laparoscopic operation of incarcerated obturator hernia with assisted intestinal resection. Chirurg 1993;64:827-8. [PubMed]
- Hayama S, Ohtaka K, Takahashi Y, et al. Laparoscopic reduction and repair for incarcerated obturator hernia: comparison with open surgery. Hernia 2015;19:809-14. [Crossref] [PubMed]
- Fujita J, Uyama I, Sugioka A, et al. Experience with Laparoscopic Repair of a Strangulated Obturator Hernia: Report of a Case. Dig Endosc 2000;12:338-40. [Crossref]
- Shapiro K, Patel S, Choy C, et al. Totally extraperitoneal repair of obturator hernia. Surg Endosc 2004;18:954-6. [Crossref] [PubMed]
Cite this article as: Yang GP. Laparoscopy in emergency hernia repair. Ann Laparosc Endosc Surg 2017;2:107.


