Minimally invasive approach to intrahepatic cholangiocarcinoma: technical notes for a safe hepatectomy and lymphadenectomy
Introduction
Intrahepatic cholangiocarcinoma (ICC) is the second most common primary liver cancer in humans after hepatocellular carcinoma, with an incidence of 0.3–3.36 new cases every 100,000 yearly in western countries (1). Differently from hepatocellular carcinoma, whose risk factors are well known and also related to the geographic distribution (2), ICC’s risk factors are less recognized. Some of these include the presence of intrahepatic biliary stones and primary sclerosant cholangitis (3). ICC’s growth is often silent and weaselly, with the possibility of reaching huge dimension at the moment of the diagnosis, making about half of the patients affected by ICC not suitable for surgery with curative intents. ICC’s prognosis is dismal as well, with a mortality at 3 months for advanced cases (4), and a 5-year survival which is inferior to 40%.
The resectability of patients affected by ICC is determined by the possibility to obtain R0 margin through liver surgery. For ICC, this often means requiring major liver resection. Furthermore, the role of LND is well recognized, indeed a “formal lymphadenectomy” is recommended not just to complete the staging of the disease, but also to limit the possibility of a tumor spread through the lymphatic system. The previous two arguments made laparoscopy to be historically poorly applied in treating cholangiocarcinoma, both for the needing of major hepatectomies and for the necessity of performing formal lymphadenectomies.
The aim of this review is to investigate the extension and the diffusion of the use of laparoscopy applied to surgical treatment of ICC, beside to furnish technical notes to conduct safe liver resection and LND for ICC.
Methods
Search strategy
We conducted a literature search using PubMed, screening all English publications on laparoscopic (LPS) liver resection for ICC. The following keywords were used to identify articles relevant to our study: “laparoscopic cholangiocarcinoma”, “laparoscopic intrahepatic biliary cancer”.
Results
Search results
Through the described keywords, we identified 11 studies encompassing both small series and case reports from institutions which approached ICC laparoscopically with curative intents (Table 1). Five more papers were identified, which are relative to the importance of diagnostic laparoscopy as a staging tool, but without any mention of a minimally invasive treatment of ICC through LPS surgery.
Table 1
| Study name | Study characteristics | No. of patients treated (open vs. LPS) | No. of laparoscopically treated affected by ICC | No. of laparoscopic major resections | No. of conversion | Morbidity (open vs. LPS) |
|---|---|---|---|---|---|---|
| Abu Hilal, 2011 | Case report | 0 vs. 2 | 2 (100%) | 2 (100%) | 0 | NA vs. 0% |
| Bryant, 2009 | Case series | 0 vs. 166 | 3 (1.8%) | 31 (18.7%) | 16 (9.6%) | NA vs. 15% |
| Tang, 2006 | Case series | 0 vs. 40 (36 hand assisted, 4 pure laparoscopic) | 1 (2.5%) | 0 | 1 (2.5%) | NA vs. 20% |
| Uy, 2015 | Case series | 26 vs. 11 | 5 (45.5%) | 6 (54.5%) | 0 | 26.9% vs. 9.1% |
| Chan, 2014 | Case series | 112 vs. 100 | 4 (4%) | 26 (26%) | 8 (8%) | NR vs. 21% |
| Rotellar, 2014 | Case report | 0 vs. 1 | 1 (100%) | 1 (100%) | 0 | NA vs. 0% |
| Takahashi, 2013 | Case report | 0 vs. 1 | 1 (100%) | 1 (100%) | 0 | NA vs. NR |
| Wang, 2015 | Case series | 60 vs. 30 | 5 (16.7%) | 0 | 0 | 16.7% vs. 10% |
| Lee, 2016 | Case series | 23 vs. 14 | 14 (100%) | 7 (50%) | 0 | 21.7% vs. 21.4% |
| Aldrighetti, 2015 | Case series on a national survey | 0 vs. 1,497 | 45 (4.1%) | 106 (7.1%) | 180 (10.7%) | NA vs. 22.8% |
| Ratti, 2015 | Case series | 60 vs. 20 | 20 (100%) | 17 (85%) | 1 (5%) | 13.3% vs. 15% |
LPS, laparoscopic; ICC, intrahepatic cholangiocarcinoma; NA, not applicable; NR, not reported.
Feasibility
Exclusion criteria of patients affected by ICC from LPS programs may be addressed to the disease’s features themselves, which constitute a relative contraindication for the presence of technical challenges: firstly, huge resections requiring vascular or biliary reconstructions, and, secondly, the necessity to guarantee an adequate LND, which is nowadays recommended by the European Association for the Study of the Liver guidelines (1) for the treatment of ICC.
As laparoscopy is currently poorly applied to the treatment of ICC, data regarding this pathology are often included in casuistries encompassing both primary and secondary liver diseases, with scarce specificity to ICC. Nevertheless, we would point out the reasons capable of affecting the feasibility of laparoscopy for ICC, that we assume being three: the needing to convert to open surgery, the post-operative morbidity and the role of LPS LND.
Conversion to open surgery
Among the 11 studies we identified, 5 presented the conversion rate to open surgery and the reasons for conversion. Of these, 3 studies (5-7) are miscellaneous case series that encompass just few LPS resections for ICCs (range, 1.8–4%). This small portion of LPS resections for ICCs is also aligned to the bigger casuistry collected by Aldrighetti et al. in a national survey (8), whereas on a sample of 1,497 LPS resections, 4.1% were executed for ICCs.
In Table 2, we reported the conversion rate and we analysed the reasons that took authors to convert to open surgery.
Table 2
| Reason for conversion | Study name/No. of conversion to open surgery | Amount | ||||
|---|---|---|---|---|---|---|
| Bryant, 2009/16 (9.6%) | Tang, 2006/1 (2.5%) | Chan, 2014/8 (8%) | Aldrighetti, 2015/180 (10.7%) | Ratti, 2015/1 (5%) | 206 | |
| Intraoperative hemorrage | 8 | 1 | 3 | 62 | 74 (35.9%) | |
| Concerns for oncological radicality | 5 | 47 | 1 | 53 (25.7%) | ||
| Technical difficulties (adhesions, bowel injury, poor exposition) | 3 | 5 | 58 | 66 (32%) | ||
| Anesthesiological problems | 5 | 5 (2.4%) | ||||
| Not reported | 8 | 8 (4%) | ||||
Among the 1,882 cases included in the studies we analyzed, there were 206 (10.9%) conversions to open surgery. Of these, the main reason were intraoperative hemorrhages (35.9%), followed by technical difficulties (32%) encompassing adhesions from previous surgery, hollow viscous injuries or toughness related to inadequate exposition and managing through laparoscopy. Another quarter of the causes of conversion were due to concerns to achieve oncological radicality (25.7%), whereby a LPS management would not have allowed R0 margins under safe circumstances. It should be bear in mind that these data are relative to spurious casuistries, not specific for ICCs, although if it is likely they embody also the reality of the LPS treatment of cholangiocarcinoma.
Post-operative morbidity
We found three studies that were specific in analyzing the role of laparoscopy for ICCs (9-11) and that were aimed to compare post-operative morbidities between open and LPS surgery (Table 3).
Table 3
| Morbidity | Study name/No. of open vs. cases LPS | |||||||
|---|---|---|---|---|---|---|---|---|
| Uy, 2015/26 vs. 11 | Lee, 2016/23 vs. 14 | Ratti, 2015/60 vs. 20 | ||||||
| Open | LPS | Open | LPS | Open | LPS | |||
| Ascitis | 0 | 1 (9.1%) | 1 (4.3%) | 0 | ||||
| Intraabdominal fluid collection | 2 (7.7%) | 0 | 0 | 1 (7.1%) | ||||
| Wound problems | 2 (7.7%) | 0 | 1 (1.7%) | 0 | ||||
| Pneumonia | 2 (7.7%) | 0 | 1 (1.7%) | 0 | ||||
| Ileus | 1 (1.8%) | 0 | 2 (3.3%) | 0 | ||||
| Biliary leakage | 4 (17.4%) | 2 (14.2%) | 2 (3.3%) | 1 (5%) | ||||
| Hemorrage | 1 (1.7%) | 0 | ||||||
| Transient liver failure | 1 (1.7%) | 0 | ||||||
| Pleural effusion | 2 (3.3%) | 1 (5%) | ||||||
| Fever | 2 (3.3%) | 1 (5%) | ||||||
| Overall morbidity | 7 (26.9%) | 1 (9.1%) | 5 (21.7%) | 3 (21.4%) | 8 (13.3%) | 3 (15%) | ||
LPS, laparoscopic.
Although the exiguity of the samples, the LPS technique didn’t show any significant variances in terms of increasing post-operative morbidity, witnessing the applicability and the feasibility of the minimally invasive technique also in ICC’s treatment.
The role of LND
Among the six studies that discussed the role of LND (Table 4), Wang et al. (12) considered the needing of a LND as exclusion criteria to perform the operation laparoscopically due to the difficulty of achieving R0 resections. On the other side, few authors performed LND laparoscopically, proving performing LPS LND didn’t constitute an element of increased morbidity in comparison to not doing it or compared to the lymph nodes harvesting in open surgery (9), thereby demonstrating LPS LND should not contraindicate the minimally invasive approach.
Table 4
| Study name | No. of laparoscopically treated affected by ICC | Lymphadenectomy (No. of cases) | No. of lymph nodes harvested | No. of patient with metastatic lymph nodes |
|---|---|---|---|---|
| Abu Hilal, 2011 | 2 | 1 (50%) | NR | 0 |
| Uy, 2015 | 5 | 1 (20%) | NR | 0 |
| Takahashi, 2013 | 1 | 1 (100%) | NR | 1 |
| Wang, 2015 | 5 | 0 | ||
| Lee, 2016 | 14 | 5 (35.7%) | 5 (average) | 0 |
| Ratti, 2015 | 20 | 10 (50%) | 7 (median) | 2 |
ICC, intrahepatic cholangiocarcinoma; NR, not reported.
Technical issue
As we described, surgery for ICC requires both a hepatic transection which were oncologically correct achieving R0 margins, associated to a LND. These criteria belonging to open surgery must be applied to the LPS procedures as well, in the purpose of guarantee the adequate principles of oncologic validity.
Our intent is to describe technical issues regarding both LPS LND and the hepatic transection.
LPS LND
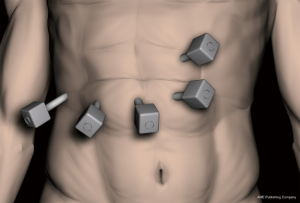
Under general anesthesia, using the LPS French position with the first operator between the patient’s legs and having the first and the second assistant respectively on the left and on the right side of the patient, five LPS ports are placed in a standardized fashion drawing an “inverted J” on the patient’s abdomen (Figure 1).
We routinely adopt a slightly modified French position for any kind of liver resection, having both the knees and the hips lightly bent thus allowing a better and safer reverse Trendelenburg tilting. Both arms are kept opened to increase the patient stability, to allow a better anesthesiologic management and to reduce the risk of involuntarily injuries to upper arms and hands (Figure 2). A pneumatic heaver under the right hemicostate on the back can be inflated as needed to allow better achieving of posterior and superior segments.

After prepping and draping, a Rochard’s retractor is always placed to allow a faster conversion to open surgery in case of necessity.
Pre-resective assessment is completed intraoperatively through an accurate US using the LPS probe, in order to confirm the operability in an R0’s target.
As we consider the LPS LND a demanding surgical time, which requires an advanced LPS training, we prefer performing it as the first surgical time, before proceeding with the hepatic transection.
The LND is guided by an accurate preoperative CT evaluation, which allows clearly to identify the celiac tripod, the origin or the common hepatic artery and its right and left branches, and possible accessory branches coming from the left gastric artery and/or from the superior mesenteric artery. Finally, particular attention should be also paid to the anatomy and to anatomic variations of common portal trunk, with particular carefulness to extraparenchimal “early” origin of left or right portal branches.
“Formal lymphadenectomy” of ICC encompasses the complete removal of lymph node station 8 (on the common hepatic artery) and 12 (encompassing regional nodes 12a along the hepatic artery, 12b along the bile duct and 12p behind the portal vein) (Figure 3).
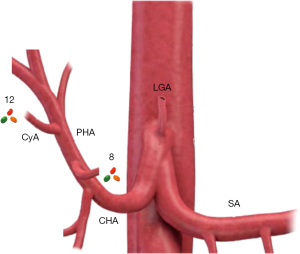
A possible extension to station 13 (lymph nodes on the posterior surface of the pancreatic head) is possible if the preoperative workup (CT and/or MRI) is consistent with a severe lymphadenopathy involving that region.
We start lymph nodes dissection at the celiac tripod, detecting the origin of the common hepatic artery, and it should be conducted up to completely skeletonizing the common hepatic artery (Figure 4), upon its entrance into the hepatoduodenal ligament.
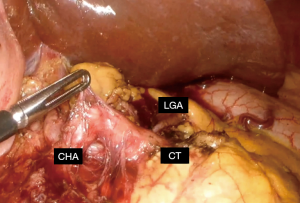
We believe the utilization of a device both capable of sealing and cutting contemporaneously were particularly useful in this phase, alternatively using the hook and bipolar forceps for a particularly precise dissection. During this time of dissection, it is particularly important also recognize the left gastric artery arising from the celiac tripod, avoiding to interrupt or to damage possible accessory arteries deriving from it that may be directed to the left hepatic lobe, if this is not in accordance with the planned liver resection.
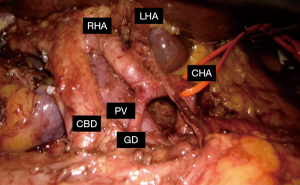
Once obtained a complete LND of the common hepatic artery, the aim of LND is to obtain a complete removal of the lymphatic tissue encompassed into the hepatoduodenal ligament, in order to complete the harvesting of the entire station 12. The dissection should be particularly precise at this time as well, in order to avoid any injury to the common bile duct, to the right and left branches of the hepatic artery and to the portal trunk (Figure 5).
Once the LND of the hepatic pedicle is completed, the following surgical time is constituted by the hepatic transection.
Hepatic transection
Before any kind of hepatic transection, with the exception constituted by superficial nodulectomy and by the left lateral sectionectomy, we retain the placement of a Pringle’s manoeuver as a must in order to have a vascular control to avoid any major bleeding during both open and LPS resections. However, we think the placement of a Pringle’s manoeuver in a standard fashion by using an umbilical lace and a tourniquet, should be avoided in cases where the vessel’s walls are exposed as a result of the LND. We recommend, instead, the use of LPS clamps for selective portal and arterial intermittent clamping, alternating 10 minutes of ischemia to 5 minutes of reperfusion. Once confirmed the resection’s limits through US, the transection is performed by using an ultrasound dissector, exposing vascular structures which are selectively coagulated by bipolar forceps or sealed through clips or staplers, according to dimension.
Short term outcome
Although the lack of data specific for ICC showed in feasibility, we retain the 3 limiting factors (conversion to open, morbidity, LPS LND) might be overtaken and tackled in the contest of an advanced LPS skills. Particularly, the conversion rate of 10.9% is comparable to the overall conversion rate to open for other advanced LPS procedures.
We could not identify neither significant differences in terms of morbidity between open and LPS surgery for ICC. In favour of this, there might be a particular attention to the selection of cases, aimed in candidate to laparoscopy cases of ICCs with a not widely extended disease. To our knowledge, the most important series of patients affected by ICC was recently described by Ratti et al. (9), with a 7.6% (20/266) of patients treated laparoscopically on a consecutive series who were affected by ICC, whereas the national average presented in an Italian survey was 4% (45/1,085) of the total of patients treated for malignant tumors (8). In their series, Ratti et al. demonstrated morbidity was similarly low and comparable between the LPS group and the open one; additionally, patients belonging to the LPS group showed a faster functional recovery, as a result of an inferior biologic stress.
Knowledges relative to lymph nodes retrieving are even rarer. Few authors consider LND as a contraindication to approach cases laparoscopically due to technical difficulties. Others, instead, consider LPS LND feasible, with similar results in terms of number of lymph nodes retrieved compared to open, without causing any increasing in morbidity.
Long term outcome
Among the two case series which assessed the role of LPS for ICCs, having a group of open resection as control one, there wasn’t any statistically significant difference between the two groups in terms of disease free survival and on the 3-year overall survival (9,11).
Conclusions
Despite the dramatic improvements of LPS technologies and their extensive application to treatment of primary and secondary, either benign or malignant liver diseases, still few cases of ICC receive a minimally invasive treatment.
Although the lack of data in the literature, we believe application of LPS to ICC is safe due to a comparable conversion rate respectful to other major LPS liver resections, and because it did not show any increasing of morbidities in the examined series. Furthermore, it is effective, as long term results were equal to those deriving from open surgeries. Though LPS LND is technically challenging, we described it is feasible as well, by conducting an accurate preoperative assessment aimed to identify the vascular anatomy and its variations. Furthermore, LPS LND is not cause of increased morbidity.
We wish laparoscopy could soon join the standard of care for resective liver surgery and LND for ICC, in order that those patients also might benefit of advantages deriving from minimally invasive surgery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Giovanni Battista Levi Sandri) for the series “Laparoscopic Liver Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.03.05). The series “Laparoscopic Liver Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol 2014;60:1268-89. [Crossref] [PubMed]
- Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet 2012;379:1245-55. [Crossref] [PubMed]
- Cho SY, Park SJ, Kim SH, et al. Survival analysis of intrahepatic cholangiocarcinoma after resection. Ann Surg Oncol 2010;17:1823-30. [Crossref] [PubMed]
- Park J, Kim MH, Kim KP, et al. Natural History and Prognostic Factors of Advanced Cholangiocarcinoma without Surgery, Chemotherapy, or Radiotherapy: A Large-Scale Observational Study. Gut Liver 2009;3:298-305. [Crossref] [PubMed]
- Chan FK, Cheng KC, Yeung YP. Laparoscopic liver resection: lessons learnt after 100 cases. Hong Kong Med J 2014;20:386-92. [PubMed]
- Bryant R, Laurent A, Tayar C, et al. Laparoscopic liver resection-understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg 2009;250:103-11. [Crossref] [PubMed]
- Tang CN, Tsui KK, Ha JP, et al. A single-centre experience of 40 laparoscopic liver resections. Hong Kong Med J 2006;12:419-25. [PubMed]
- Aldrighetti L, Belli G, Boni L, et al. Italian experience in minimally invasive liver surgery: a national survey. Updates Surg 2015;67:129-40. [Crossref] [PubMed]
- Ratti F, Cipriani F, Ariotti R, et al. Safety and feasibility of laparoscopic liver resection with associated lymphadenectomy for intrahepatic cholangiocarcinoma: a propensity score-based case-matched analysis from a single institution. Surg Endosc 2016;30:1999-2010. [Crossref] [PubMed]
- Uy BJ, Han HS, Yoon YS, et al. Laparoscopic liver resection for intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 2015;25:272-7. [Crossref] [PubMed]
- Lee W, Park JH, Kim JY, et al. Comparison of perioperative and oncologic outcomes between open and laparoscopic liver resection for intrahepatic cholangiocarcinoma. Surg Endosc 2016;30:4835-40. [Crossref] [PubMed]
- Wang XT, Wang HG, Duan WD, et al. Pure Laparoscopic Versus Open Liver Resection for Primary Liver Carcinoma in Elderly Patients: A Single-Center, Case-Matched Study. Medicine (Baltimore) 2015;94:e1854 [Crossref] [PubMed]
Cite this article as: Fiorentini G, Ratti F, Cipriani F, Palombo D, Catena M, Paganelli M, Aldrighetti L. Minimally invasive approach to intrahepatic cholangiocarcinoma: technical notes for a safe hepatectomy and lymphadenectomy. Ann Laparosc Endosc Surg 2017;2:68.