
Extended laparoscopic liver resection: initial experience and review of the literature
Introduction
The number of liver resections performed by minimally invasive approach has increased significantly in recent year (1-7). Laparoscopic extended liver resections have been limited to very few centers with only few reported papers so far (7-15).
The estimated number of minimally invasive extended liver resections, including pure laparoscopic, laparoscopic-assisted and robotic-assisted is 35 cases. Duplicated cases whenever identified were excluded (9,10,15).
The objective of this study is to perform a comprehensive analysis of our experience with extended laparoscopic liver surgery, with emphasis in the safety and feasibility.
Methods
All patients undergoing liver resection from a prospective database at our institution were analyzed. The prospective database and the retrospective study were approved by our institutional review board and patient consent was waived due to anonymization of data in the database and its retrospective character. Patients submitted to extended laparoscopic liver surgery between 2007 and December 2016 were object of the present study. Future liver remnant (FLR) assessment was performed by either CT or MRI volumetry. Patients with insufficient FLR were submitted to preoperative portal vein embolization. In cases of bilateral disease and/or extremely small FLR, two-stage liver resection was performed.
Surgical technique
In all cases, the technique employed was the intrahepatic Glissonian approach, except two patients with intrahepatic cholangiocarcinoma with hilar extension that needed dissection of the portal triad at the level of the hepatic hilum and Roux-en-Y hepaticojejunostomy. The technique used in the majority of the patients is described below.
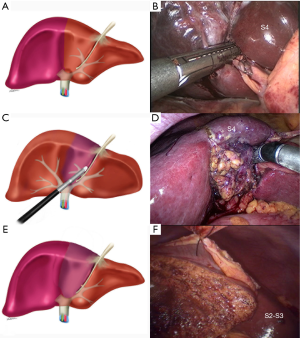
Right extended liver resection
Operation begins with examination of the abdominal cavity followed by intraoperative ultrasound. Patient is operated on in supine position with legs spread apart, with the surgeon placed between the patient’s legs. Usually four or five trocars are necessary. For the control of the right pedicle, we use the intrahepatic Glissonian approach as previously described. Briefly, two tiny liver incisions are performed following specific anatomical landmarks (16,17). The first at the level of the hilum, and another is done in the transition zone between segments 7 and 1. A clamp is introduced through these incisions and its closure will result in ischemic discoloration of the right liver. The clamp is substituted by an endoscopic stapler (Figure 1A) and the right pedicle is completely partitioned (Figure 1B). Once this is performed, the pedicle from segment 4 is divided by inserting a stapler between two new incisions (Figure 1C); one above the hilum to the left and another on the right margin of the round ligament (Figure 1D), as previously reported (18,19). This maneuver will complete the inflow control to proceed with extended right hepatectomy (Figure 1E). The line of future transection is marked with cautery and parenchymal division is performed (Figure 1F).
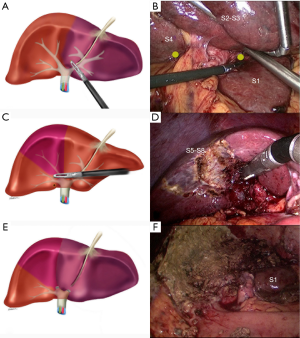
Left extended liver resection
The main steps are the same as described for right extended hepatectomies. However the intrahepatic accesses for Glissonian pedicles for left extended hepatectomy are different and have already been described elsewhere (17,19). In brief, a tiny incision is made above the ligament of Arantius and another is performed above the hilum to the left (Figure 2A). Temporary insertion of a vascular clamp through these incisions (Figure 2B) will confirm control of the left liver Glissonian pedicle (segment 1 is spared). The left pedicle is then divided with stapler. To complete the inflow control for extended left hepatectomy, right anterior section (segments 5 and 8) pedicle needs to be divided. This can be achieved with two incisions, one above the hilum, and another on the right edge of the gallbladder bed (Figure 2C), as previously described (17). The pedicle is divided by stapler (Figure 2D) resulting in complete control of the inflow control for extended left hepatectomy (Figure 2E). Liver is transected as usual (Figure 2F).
Variables
Safety was assessed as the occurrence of complications and 90-day mortality. Feasibility was assessed by conversion rate, operative time, blood loss, need for transfusions, and hospital length of stay. The data was prospectively registered by the surgical team. Pathology reports were also reviewed.
Results
Between 2007 and 2016, 23 extended laparoscopic liver resections were performed. Twelve (52%) as a second stage in a staged liver resection and 11 (48%) were performed during one-stage resection with or without preoperative portal vein embolization. There were 13 women and 10 men with mean age of 56.3 years [22–73]. The main indication for liver resection was colorectal liver metastases (15 patients), cholangiocarcinoma (5 patients), hemangioendothelioma (2 patients) and one patient with angiomyolipoma. The latter patient was object of a previous publication (11). No patient presented cirrhotic liver but all colorectal patients’ undergone preoperative systemic chemotherapy.
Two patients needed conversion to open surgery, one due to hemorrhage and one due to technical difficulties. Blood loss was significant in 6 patients with need for transfusion. The mean operative time was 245 minutes. One patient operated on for malignant disease presented with positive margins. Median hospital stay was 7 days.
Significant complications occurred in six patients (26.1%). Three patients developed liver failure, two had infectious complications and one patient developed limited biliary fistula. No 90-day mortality was observed.
Discussion
Extended liver resections are rarely performed by laparoscopy (8-15). There are very few centers performing this operation in the literature. The main reason is that whenever a patient needs such a large liver resection the laparoscopic approach is seldom considered. However, high volume centers with experience in laparoscopic liver resection are performing this complex operation with excellent results.
The number of minimally invasive liver resections is rapidly increasing with more than 9,500 cases performed worldwide (20). The proportion of surgeries being done for malignancies has increased from 50% at the time of the first international consensus to 65% currently after the second international consensus (21). The total number of cases has rapidly increased from 2,804 to more than 9,500, according to a recent review (20).
In the present study, we share our experience and lessons learned with the performing of laparoscopic extended liver resection. The main concern with this type of operation is indeed with the FLR. Another issue is the quality of the liver, once prolonged chemotherapy or underlined liver disease may compromise the safety of this operation. FLR should be precisely calculated with preoperative imaging. In the majority of cases, portal vein embolization or two-stage operations are valid strategies to supersede low FLRs.
In our experience, the use of the Glissonian approach was helpful in all cases where the tumor was not close to the hilar plate that warrants complete dissection of hilar elements. This situation was present in two of our cases; both of them were intrahepatic cholangiocarcinomas with invasion of the hilar plate and needed hepaticojejunostomy. This situation requires the same approach as for hilar cholangiocarcinoma (13,14). In all other cases, ischemic delineation after control of the Glissonian pedicles facilitated the correct identification of the future line of transection which is the main difficulty in such cases.
Despite the lack of randomized controlled trials, there is enough evidence to confirm the safety of laparoscopic liver surgery in selected patients (20). Non-anatomic wedge and left lateral resections are now considered standard in several centers, including ours.
Although laparoscopic hemihepatectomies have been performed by our team since the beginning of our experience (22), minimally invasive left and right hepatectomies are still performed by a limited number of centers worldwide.
Meta-analysis of studies comparing laparoscopic to open liver surgery shows that laparoscopy is associated with less complications, less blood loss, less transfusions, less hospital stay, equivalent operative time and equivalent resection margins (23). However, most studies combine major and minor liver resections and there is still a debate whether laparoscopic major liver resection would have the same results and outcomes if studied separately.
Laparoscopic extended hepatectomies have been limited to very few centers and there still no clearly statement in the literature. During the second international consensus of laparoscopic liver surgery in Morioka (3), extended liver resection was not thoroughly discussed due to scarce literature and requires further evaluation and caution. To date, we found few studies mentioning extended liver resections, in a total of 35 cases. Adding 22 new cases from our center, we have now 57 cases in the literature so far.
Our initial experience with 23 patients showed that extended liver resections can be safely performed by laparoscopy if quality and volume of the FLR is adequately studied. Three patients presented with some degree of liver failure while one of them had a severe liver failure with full recovery after 10 days. These three patients were not submitted to preoperative portal vein embolization and retrospective analysis of the liver remnant showed that the future liver volume was overestimated in two of them and the quality of the liver was not well assessed in one of them (prolonged chemotherapy). Other complications were related to the liver resection per se and were not influenced by the degree of liver parenchyma removed.
Conclusions
In summary, this study shows that laparoscopic extended liver resections are safe and feasible. Adequate analysis of quality and volume of the FLR is of paramount importance and some patients may benefit from portal vein occlusion. Although these results could be related to increased expertize in laparoscopic liver resections, we observed complications, operative times, hospital stay and blood loss comparable to open extended liver resections.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Giovanni Battista Levi Sandri) for the series “Laparoscopic Liver Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.19). The series “Laparoscopic Liver Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The prospective database and the retrospective study were approved by our institutional review board and patient consent was waived due to anonymization of data in the database and its retrospective character.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Dagher I, O'Rourke N, Geller DA, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 2009;250:856-60. [Crossref] [PubMed]
- Castaing D, Vibert E, Ricca L, et al. Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 2009;250:849-55. [Crossref] [PubMed]
- Rao A, Rao G, Ahmed I. Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc 2011;25:1603-10. [Crossref] [PubMed]
- Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. World J Surg 2011;35:1478-86. [Crossref] [PubMed]
- Koffron AJ, Auffenberg G, Kung R, et al. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 2007;246:385-92; discussion 392-4. [Crossref] [PubMed]
- Gumbs AA, Bar-Zakai B, Gayet B. Totally laparoscopic extended left hepatectomy. J Gastrointest Surg 2008;12:1152. [Crossref] [PubMed]
- Gumbs AA, Gayet B. Multimedia article. Totally laparoscopic extended right hepatectomy. Surg Endosc 2008;22:2076-7. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC, et al. Intrahepatic Glissonian approach for laparoscopic right trisectionectomy. J Laparoendosc Adv Surg Tech A 2009;19:777-8; discussion 778-9. [Crossref] [PubMed]
- Nitta H, Sasaki A, Fujita T, et al. Laparoscopy-assisted major liver resections employing a hanging technique: the original procedure. Ann Surg 2010;251:450-3. [Crossref] [PubMed]
- Giulianotti PC, Sbrana F, Bianco FM, et al. Robot-assisted laparoscopic extended right hepatectomy with biliary reconstruction. J Laparoendosc Adv Surg Tech A 2010;20:159-63. [Crossref] [PubMed]
- Lin E, Sarmiento JM. Laparoscopic extended right hepatectomy, portal lymphadenectomy, and hepaticojejunostomy for hilar cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 2014;24:411-6. [Crossref] [PubMed]
- Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg 2015;102:796-804. [Crossref] [PubMed]
- Machado MA, Herman P, Machado MC. A standardized technique for right segmental liver resections. Arch Surg 2003;138:918-20. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Galvão FH, et al. Intrahepatic Glissonian approach for laparoscopic right segmental liver resections. Am J Surg 2008;196:e38-42. [Crossref] [PubMed]
- Machado MA, Herman P, Machado MC. Anatomical resection of left liver segments. Arch Surg 2004;139:1346-9. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC, et al. Laparoscopic resection of left liver segments using the intrahepatic Glissonian approach. Surg Endosc 2009;23:2615-9. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Brown KM, Geller DA. What is the Learning Curve for Laparoscopic Major Hepatectomy? J Gastrointest Surg 2016;20:1065-71. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC, et al. Laparoscopic right hemihepatectomy for hepatolithiasis. Surg Endosc 2008;22:245. [Crossref] [PubMed]
- Schiffman SC, Kim KH, Tsung A, et al. Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 2015;157:211-22. [Crossref] [PubMed]
Cite this article as: Machado MAC, Surjan RC, Basseres T, Makdissi FF. Extended laparoscopic liver resection: initial experience and review of the literature. Ann Laparosc Endosc Surg 2017;2:32.


