Stapled hemorrhoidopexy: no more a new technique
Introduction
In the literature, there are several theories describing the causes of the hemorrhoidal disease. Some believe that it is primarily a disease of the veins in line with the varicose veins in the esophagus. A morphological and functional failure of a sphincter mechanism coordinating the filling and drainage of the anorectal vascular cushions may be the cause (1). Another hypothesis is that the disease is caused by a weakening of the collagen support in the anal canal where the submucosal collagen fibrils degenerates with sliding mucosa during defecation or physical activity as a result (2). A third theory suggests an increased arterial flow to the vascular plexus (3). Constipation and bowel habits with straining are associated with the hemorrhoidal disease (4,5). The hemorrhoidal disease affects the general population between 4.4% and 36.4% (6,7). Physiologically hemorrhoids are anal cushions that can become symptomatic through prolapse and bleeding. When they become symptomatic you may occur secondary symptoms: pain, pruritus and mucus loss. Often it is not found correlation between the presence of hemorrhoids and the clinical symptoms (6,8). The common symptoms are: bleeding, prolapse, pain, discharge, itching and hampered anal hygiene. There is no correlation between specific symptoms and anatomic grading. The presence of a severe hemorrhoidal prolapse can cause poor symptomatology (2), while the presence of normal anal cushions may be associated with important clinical symptoms that can cause great anxiety in patients. In this last case, the socioeconomic and cultural factors play an important. A few attempts to create a symptom score have been made, but a validated symptom score is not available at the moment. History should include toilet habits, stool frequency, stool consistency and difficulties in rectal emptying. Dietary habits in terms of fiber intake should be assessed. Milligan et al. in 1937 proposed the open hemorrhoidectomy for the treatment of symptomatic hemorrhoids, since then this surgical technique was the most practiced and accepted in the world (9,10). Despite its effectiveness, this technique is associated with postoperative pain for the presence of open wounds in a sensitive area and that require local therapy. For these reasons, the technique is not well accepted by patients and different approaches have been advocated from time to time (7,11). In the past years, several studies (9,11,12) have modified the anatomy and physiology of hemorrhoids underlying some important pathogenetic aspects. These findings are also the rational basis of a totally new surgical approach in the treatment of hemorrhoidal disease. In 1998 Longo proposed what sounded, at the time, like an ideal solution: a procedure for hemorrhoidectomy with minimal postoperative pain, no perianal wound requiring postoperative wound care and a relatively short operative time (13). His technique presented a new notion for treating hemorrhoids as he proposed circumferential rectal mucosectomy that results in mucosal lifting (anopexy). His aim was not excision of the hemorrhoidal tissue but rather restoring anatomical and physiological aspects of the hemorrhoidal plexus (14). As early as 2001, there were several studies to confirm that stapled hemorrhoidopexy is a safe procedure that is associated with a shorter operative time, low postoperative pain, shorter hospital stay and a more rapid return to normal activities of daily living than other surgical techniques (15). Several subsequent randomized controlled trials and reviews confirmed these findings, with some studies claiming that stapled hemorrhoidopexy is the most effective and safe procedure for hemorrhoids (16). Based on these early successes and the expected interest in new procedures that might reduce postoperative pain, stapled hemorrhoidopexy has acquired a considerable popularity (17) with a reputation as a safe and effective alternative approach for the treatment of hemorrhoids (18). There have been recent calls for further randomized trials to investigate the long-term outcomes of stapled hemorrhoidopexy. Whether such trials are now practical is debatable. Given the proven short-term benefits of the stapled technique, it is possible that clinicians and patients will be reluctant to randomise to open surgery. Long-term follow-up data is already beginning to emerge (19-23), and perhaps future research efforts might better be engaged in undertaking a comprehensive cost-effectiveness analysis, incorporating both hospital and community costs. The latest evidence on stapled hemorrhoidopexy suggests that it is a technique that is finally coming of age and establishing itself as a credible alternative to conventional hemorrhoidectomy. It is probably most suited to the treatment of grade III, and perhaps circumferential grade II, hemorrhoidal prolapse. Controversy remains regarding its role in large volume and grade IV prolapse, due to increased rates of recurrence. Until this is resolved, it is unlikely that stapled hemorrhoidopexy will attain acceptance as the preferred “gold standard”. In comparison, the fate of conventional hemorrhoidectomy appears somewhat uncertain, accepting that it will continue to have a role in specific circumstances. It is likely that “patient’s choice” will ultimately determine its survival or otherwise, and will be driven by how acceptable postoperative pain is in the era of modern surgical technology.
Patient selection and workup
Treatment of the hemorrhoidal disease and assessment of treatment outcome must be based on a uniform grading. Investigation in different positions is described, lithotomy position, left lateral position (Sims) position, sitting on a toilet chair and photo documentation with the patient standing or sitting. Grading is dependent on the position of the patient examined. The prerequisite for a proper grading is standardized examination conditions, or at least, a description of the position during examination. The grading system described by Goligher, is the most commonly used and is based on objective findings and history (24):
- Grade I: no prolapse, vascular cushions in the anal canal visualized by endoscopy;
- Grade II: prolapse during defecation, but spontaneous reduction;
- Grade III: prolapse during defecation, which need manually reduction;
- Grade IV: persistent prolapse irrespective attempt to reduce the prolapse.
Clinical examination can be performed in different positions. The patient can be placed in the prone position, on the left side with knees bent to his chest, or in the knee-elbow position. The inspection will evaluate the perianal skin and anus closure. At this stage, grade IV hemorrhoids will already be visible. The strain can be highlighted hemorrhoids of grade II and III as spontaneous prolapse. Subsequently, digital rectal exam will evaluate the functionality of sphincter anus. Grade II–IV hemorrhoids may be appreciated as tense-elastic cushions. The instrumental exams includes colonoscopy and defecography; the first is performed both in women than in men, especially in the case of bleeding and family history of malignant disease, the second is useful in women and optional for men. This latest exam helps the surgeon to exclude the presence of rectal prolapse, rectocele, edrocele and uro-gynecological pathologies associated. Surgery is performed for grade III and IV (Figures 1,2), for grade II in case of major bleeding. Absolute contraindications are the presence of abscess, gangrene, anal stenosis and complete rectal prolapse.
Pre-operative preparation
Preoperatively, the patient is subjected to blood and urine tests, chest X-ray and electrocardiogram. These tests are normally done a few days prior to surgery. These exams are performed prior to admission. The anti-platelet drugs such as aspirin should be discontinued three days before the surgery, while the anticoagulants should be replaced with subcutaneous heparin seven days before. For spinal anesthesia, dietary restrictions vary. The patient must observe fasting after midnight, it is tolerable 2 hours before take, with a little water, antihypertensive and antidiabetic drugs. It would be better perform this type of surgery in the hospital and not in outpatient. Admission occurs on the same day of the surgery and after the anesthesiologist examination the patient is given the informed consent form that must be well understood and signed. Two or three hours before surgery, a low enema is practiced to eliminate solid stool that could reduce the view of the operating field. Finally, a sedative is administered before surgery.
Equipment preference card
- Team: two surgeons, two nurses.
- Procedure: stapled hemorrhoidopexy.
- Anesthesia: spinal.
- Antibiotic prophylaxis: single dose of prophylactic antibiotic, cephalosporin 2 g (monocef), was given intravenously 2 h before the procedure.
- Position: lithotomy.
- Skin preparation: wash with iodopovidone solution (5 min).
- Equipment: suction apparatus, headlamp (available), urinary catheter, minor instrumentation set, 10 cm × 10 cm gauzes, 1 stapler (special sterile kit consisting of a circular stapler, 33 mm, a circular anoscope with dilator and a suture anoscope), lubricating solution, long gauze for the final buffer.
- Suture: 2-0 prolene for pursestring, 3-0 polygalactine for hemostasis along staple line.
- Other equipment: one precision scale to weigh the surgical specimen.
Procedure
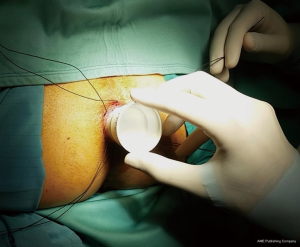
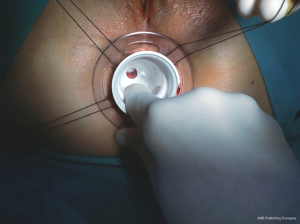
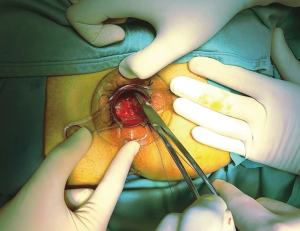
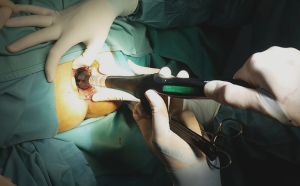
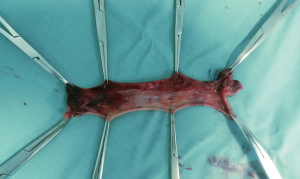
The patient can be placed in the lithotomy position, jack knife position or on the left side with knees to chest, it is generally preferred the lithotomy position (Figure 3). All patients receive antibiotic prophylaxis before induction of anesthesia. The same way as open hemorrhoidectomy, different types of anesthesia can be chosen, local, spinal or general can be used, and the choice depends on the surgeon’s preferences. Urinary catheter is positioned in all patients. After disinfection of the surgical field, stapled hemorrhoidopexy is performed with Longo’s technique. The anal canal is manually dilated, with subsequent insertion of the obturator (Figure 4). Obturator is extracted and placed inside the circular anal dilator, and simultaneously inserted into the anal canal. After obturator removing will observe the placement within the external hemorrhoidal prolapse (Figure 5). Anal dilator is positioned correctly when the inside edge past the dentate line. This will help prevent damage to the dentate line and the internal sphincter. Externally anal dilator is provided with four slits through which is firmly fixed to the perianal skin with four silk staples (Figure 6). Inside the anal dilator is positioned anoscope, the surgeon rotates the anoscope and manufactures a circumferential purse string of 2-0 prolene. The correct height for the suture is at 2 cm from the apex of hemorrhoids, and it must include only mucosa and submucosa (Figure 7). At each rotation, the anoscope must be extracted and inserted again to avoid the rolling of the mucosa with consequent asymmetry of the purse-string. At the end, while tightening the suture is inserted a finger inside to check its circumferential integrity. At this point the open circular stapler is introduced in such a way that the anvil goes beyond the suture line. The suture is tightened and closed with a surgical knot around the stem of the stapler and the two ends of the suture thread are pulled through the lateral casing slits. The ends of the suture are knotted externally or fixed using a clamp. Pulling slightly and constantly the terminal portion of the suture the stapler is tightened so as to favor the entry of the tissue inside the casing. Once the casing reaches the half of the anal dilator the stapler should be pushed into the anal canal and completely closed. The stapler is aligned to the longitudinal axis of the anal canal, and after releasing the block it is fired. The closure must be maintained for 30 seconds to aid in hemostasis (Figure 8). In females posterior vaginal wall was checked before firing the stapler to prevent entrapment. The stapler was then one turn anticlockwise opened to its maximum and gently withdrawn. The staple line should be well checked for possible bleeding that can be corrected with surgical staples of polyglactin 3-0. At the end of operation, anal canal was packed with gauze dressing which was removed in the morning after surgery. The circular sample can be sent for histopathological analysis (Figure 9).

Role of team members
The team consists of four persons (Figure 10): (I) the surgeon who performs the surgery; (II) assistant (surgeon or trainee surgeon) that helps in aspiration and maintain the correct position of the instrumentation and then draw up the histology; (III) the instrumentalist nurse prepares the surgical site and assists the surgeon with the correct surgical instruments; finally, (IV) a second circulating nurses for all that can occur during surgery and in conclusion cleans instrumentation.
Post-operative management
Patients normally eat the next day. On the same day they remove the urinary catheter and the gauze pad. For the evaluation of postoperative pain it is useful to use the VAS scale (0 indicates no pain; and 10, maximum pain). The pain can be estimated at 12 or 24 hours after surgery and at discharge. Pain therapy consists of a basic analgesia (paracetamol or ketorolac) on request. At discharge the patients receive a laxative syrup to be taken once a day for 15 days and the basic analgesia. Generally the average hospital stay is 2–3 days. The follow-up consists of a patient interview and physical examination to 15 days, 1 month, and 2 months after surgery.
Tips, tricks and pitfalls
After its description, some surgeons have had serious complications, but this was due to technical errors and a short learning curve. This technique is simple but needs to be applied properly. It is important that the technique is transmitted by an experienced surgeon, and including at least 25 interventions as primary surgeon. Another important aspect is the indication for surgical treatment of hemorrhoidal disease. Postoperative bleeding depends on the attention that the operator dedicated to the control of hemostasis, in 1–2% of cases may need reoperation. The cases of stenosis of the staple line are rare but may require dilations. If there is a partial dehiscence of the staple line can suffice observation. The externalized staples should be removed because they can give granulomas that bleed easily and cause prolonged postoperative pain. Compared to open hemorrhoidectomy in 30–40% of the stapled hemorrhoidopexy occurs a defecatory urgency. An answer to this could be that the suture line engages a sensitive area of the lower rectum, but it will resolve spontaneously within the first week.
Some serious complications have been described in the literature: tearing of the rectal wall may be due to a purse string too high or irregular, excessive tensile force during the closure of the stapler may also be responsible; irregular or high purse string may also be responsible for the obliteration of the rectal lumen; rectovaginal fistula can occur in women when the bag in the front wall is too deep and during the closure of the stapler is not checked the posterior vaginal wall; resection of the internal anal sphincter could happen if the purse string is too low, so that the internal sphincter will be pulled into the case of the stapler and partially or totally resected.
Other rare but serious complications: some patients 3–5 days after surgery have intense pelvic pain, this symptom often requires the use of benzodiazepines and morphine; rare reports have described some cases of necrosis of the staple line and Fournier’s gangrene of the anus; moreover, also some cases of pelvic emphysema extended to the retroperitoneum have been described. Despite the rarity of these severe complications may occur and are difficult to explain to the patient that has suffered. To date more than 4 million stapled hemorrhoidopexy have been performed worldwide with complications in very low percentage, the most serious events are rarer. For success in this type of surgery it is essential to give adequate information to the patient and perform the surgery with proper technique.
In conclusion this technique is feasible and easily reproducible, the reduction of the hemorrhoidal prolapse occurs in approximately 90% of patients with moderate postoperative pain. After a few days or at most a few weeks bowel habits return to a normal pattern without urgency. However, approximately 40% of patients may have occasional symptoms such as involuntary gas passage and soiling. After one year or longer 11% of patients may present remaining or recurrent prolapse, the reintervention rate is about 10% including a second stapled hemorrhoidopexy, open hemorrhoidectomy, excision of symptomatic skin tags, or rubber band ligation.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Aigner F, Gruber H, Conrad F, et al. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis 2009;24:105-13. [Crossref] [PubMed]
- Haas PA, Fox TA Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum 1984;27:442-50. [Crossref] [PubMed]
- Aigner F, Bodner G, Gruber H, et al. The vascular nature of hemorrhoids. J Gastrointest Surg 2006;10:1044-50. [Crossref] [PubMed]
- Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology 1990;98:380-6. [Crossref] [PubMed]
- Riss S, Weiser FA, Schwameis K, et al. Haemorrhoids, constipation and faecal incontinence: is there any relationship? Colorectal Dis 2011;13:e227-33. [Crossref] [PubMed]
- Hardy A, Chan CL, Cohen CR. The surgical management of haemorrhoids--a review. Dig Surg 2005;22:26-33. [Crossref] [PubMed]
- Loder PB, Kamm MA, Nicholls RJ, et al. Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg 1994;81:946-54. [Crossref] [PubMed]
- Jóhannsson HO, Graf W, Påhlman L. Long-term results of haemorrhoidectomy. Eur J Surg 2002;168:485-9. [Crossref] [PubMed]
- Buls JG, Goldberg SM. Modern management of hemorrhoids. Surg Clin North Am 1978;58:469-78. [Crossref] [PubMed]
- Practice parameters for the treatment of hemorrhoids. The Standards Task Force American Society of Colon and Rectal Surgeons. Dis Colon Rectum 1993;36:1118-20. [Crossref] [PubMed]
- Senagore A, Mazier WP, Luchtefeld MA, et al. Treatment of advanced hemorrhoidal disease: a prospective, randomized comparison of cold scalpel vs. contact Nd:YAG laser. Dis Colon Rectum 1993;36:1042-9. [Crossref] [PubMed]
- Thomson WH. The nature of haemorrhoids. Br J Surg 1975;62:542-52. [Crossref] [PubMed]
- Longo A. Treatment of hemorrhoid disease by reduction of mucosa and hemorrhoidal prolapse with a circular suturing device: a new procedure. Bologna: Proceedings of the 6th World Congress of Endoscopic Surgery, Rome, Italy; Monduzzi Publishing, 1998:777-84.
- Infantino A, Altomare DF, Bottini C, et al. Prospective randomized multicentre study comparing stapler haemorrhoidopexy with Doppler-guided transanal haemorrhoid dearterialization for third-degree haemorrhoids. Colorectal Dis 2012;14:205-11. [Crossref] [PubMed]
- Laughlan K, Jayne DG, Jackson D, et al. Stapled haemorrhoidopexy compared to Milligan-Morgan and Ferguson haemorrhoidectomy: a systematic review. Int J Colorectal Dis 2009;24:335-44. [Crossref] [PubMed]
- Stuto A, Favero A, Cerullo G, et al. Double stapled haemorrhoidopexy for haemorrhoidal prolapse: indications, feasibility and safety. Colorectal Dis 2012;14:e386-9. [Crossref] [PubMed]
- Jayaraman S, Colquhoun PH, Malthaner RA. Stapled hemorrhoidopexy is associated with a higher long-term recurrence rate of internal hemorrhoids compared with conventional excisional hemorrhoid surgery. Dis Colon Rectum 2007;50:1297-305. [Crossref] [PubMed]
- Basso L, Cavallaro G, Polistena A. Experience of 3711 stapled haemorrhoidectomy operations (Br J Surg 2006; 93: 226-230). Br J Surg 2006;93:507. [Crossref] [PubMed]
- Van de Stadt J, D'Hoore A, Duinslaeger M, et al. Long-term results after excision haemorrhoidectomy versus stapled haemorrhoidopexy for prolapsing haemorrhoids; a Belgian prospective randomized trial. Acta Chir Belg 2005;105:44-52. [PubMed]
- Ganio E, Altomare DF, Milito G, et al. Long-term outcome of a multicentre randomized clinical trial of stapled haemorrhoidopexy versus Milligan-Morgan haemorrhoidectomy. Br J Surg 2007;94:1033-7. [Crossref] [PubMed]
- Riss S, Riss P, Schuster M, et al. Impact of stapled haemorrhoidopexy on stool continence and anorectal function: long-term follow-up of 242 patients. Langenbecks Arch Surg 2008;393:501-5. [Crossref] [PubMed]
- Kanellos I, Zacharakis E, Kanellos D, et al. Long-term results after stapled haemorrhoidopexy for third-degree haemorrhoids. Tech Coloproctol 2006;10:47-9. [Crossref] [PubMed]
- Slim K. Long-term outcome of a multicentre randomized clinical trial of stapled haemorrhoidopexy versus Milligan-Morgan haemorrhoidectomy (Br J Surg 2007; 94: 1033-1037). Br J Surg 2007;94:1306-7; author reply 1307. [Crossref] [PubMed]
- Goligher JC. Advances in proctology. Practitioner 1964;193:526-32. [PubMed]
Cite this article as: Cianci P, Altamura A, Tartaglia N, Fersini A, Calabrese E, De Stefano U, Menga MR, Ambrosi A, Neri V. Stapled hemorrhoidopexy: no more a new technique. Ann Laparosc Endosc Surg 2016;1:25.