
A novel framework for surgical reflection
Introduction
Background
Surgeons operate in a high-stakes profession where even small mistakes can have devastating consequences for patients (1). In such a demanding and fast-paced environment, it is essential for these healthcare professionals to regularly reflect on their performance to maintain and improve their skills. Reflective practice allows surgeons to step back and examine their actions and decision-making processes, identify areas for improvement, and implement changes to their practice (2). This can lead to increased competence and better outcomes for patients (3). In addition, reflective practice can also foster a culture of continuous learning and improvement in the surgical field, which can help to reduce medical errors and enhance patient safety (4). Given the critical nature of their work, incorporating reflective practice into the regular routine of surgeons is of utmost importance to ensure that they are providing the highest standard of care for their patients. Unfortunately, in the fast paced, physically and mentally demanding environment of modern-day medicine, it is understandable that these doctors move rapidly from case to case without the opportunity to step-back and deeply critique the methods and outcomes of their practice (3). The conventions of clinical practice can take generations before enough momentum builds behind any change, often only triggered when a patient comes within touching distance of critical harm. What makes the surgical status quo even more resistant to change is that their patients can often present more heterogeneously, such that distinguishing common features and patterns can be a challenge (5).
Clinical example
It is proposed that encouraging each member of the surgical team to form constructive thoughts after a challenging or eventful case can improve the likelihood of formulating potential advancements in future care (6). For example, here we describe a case of a patient who was scheduled to undergo an elective resection of a hepatocellular carcinoma (HCC) but had developed life-threatening spontaneous haemorrhage preoperatively, a finding only identified once the surgeons had opened the abdomen. The patient, understandably, was experiencing symptoms of this severe complication, which should have been identified preoperatively by the team. However, the team were not notified of any symptomatic changes, which, in reflection, had been attributed to insufficient information provision regarding signs that should warrant self-reporting, in addition to a more rigorous pre-operative assessment of the patient.
Reflective analysis of this case resulted in a greater appreciation of this life-threatening complication and an understanding that it is more common than initially assumed. The incidence of HCC ranges considerably depending on geographical data but can run in parity with the annual risk of rupture for an abdominal aortic aneurysm measuring less than 7 cm in some instances (7,8). In response to this reflection, our team submitted a formal suggestion to the National Health Service (NHS), in attempt to amend their public information resources, such that it includes warnings of complications such as intra-abdominal haemorrhage.
Rationale
This case, and many others similar, reinforce the importance of structured reflection in the field of surgery and emphasise the value of regularly evaluating the team’s performance in such a high-stakes profession. In response, a structured framework was developed to facilitate reflective practice among surgeons particularly, but also healthcare professionals in general. This framework provides a layered approach for professionals to reflect on their actions, decision-making processes and outcomes, and allows identification of areas for improvement. By using this framework, surgeons and their colleagues can develop a deeper understanding of their own practice and gain new insights that can be applied to future cases. The framework also helps to standardise reflective practice in the surgical field and ensures that all colleagues have a consistent approach to evaluating clinical performance.
Development of the framework
To begin the development of a reflective framework, it was imperative to first acknowledge and address the critical concerns that have previously afflicted the practice of evaluating serious incidents. This information was gathered through an extensive literature search and discussions with colleagues. Our findings highlight that the lack of a formal structure to evaluate near miss incidents in clinical practice is a significant issue (9). This often leads to incidents being underreported and missed opportunities for learning and improvement. Moreover, there is limited time allocated for reflection in clinical practice, which negatively impacts the ability to learn from incidents and identify opportunities for improvement (9). It has also been highlighted that there is often too little importance placed on the actions that are suggested following reflection. This lack of follow-up on potential improvements is not only unhelpful in addressing the issues at hand, but it also negatively impacts team morale and the trust in the process of reflection.
Furthermore, junior medical staff have reported feeling underappreciated and even feeling pressured to conform to the views of their seniors during reflective sessions. This may lead to a loss of valuable input and hinder the ability to identify potential solutions. A potential reason for this may be due to the unspoken element of hierarchy which seniors possess, or it could be due to objective roles which seniors play in these reflective sessions, such as acting as chairs of the meeting (10).
The role of the entire surgical team, ranging from junior foundation doctors all the way to senior consultants, has been increasingly respected and appreciated throughout the years. Each member plays a critical role in analysing and improving healthcare provision. Team members come from a variety of backgrounds and bring unique perspectives and experiences to the table, making their input invaluable in assessing the effectiveness of care delivery. Within the surgical field, the contributions of these various healthcare professionals are particularly significant. Junior doctors, for instance, bring novel insights to the surgical team. As they are often in the earlier stages of their careers, they have recently completed extensive training and are up to date with the latest medical practices and technologies. Their perspectives can help the team to question assumptions and explore new solutions, leading to more effective care delivery. Consultants, on the other hand, offer a wealth of knowledge and expertise. With years of experience in their field, they can provide guidance and leadership to the surgical team. They are often called upon to make complex decisions and help to ensure that care delivery is of the highest quality.
Finally, meetings to discuss near miss incidents are often described to be exclusive to medical doctors, and even to a single specialty of doctors. This understandably reduces the ability to gain a broader perspective on the incident and can limit the range of solutions that are considered. Anaesthetic colleagues, for example, play a crucial role in the surgical team. They are responsible for managing the patient's experience of the surgery and ensuring that they are comfortable throughout the procedure. Their unique insights on the delivery of care can help to identify underappreciated areas for improvement and enhance patient outcomes. Nurses and other allied healthcare professionals (AHPs) involved in the delivery of care also contribute significantly to the team. They play a pivotal role in patient care, managing the patient’s post-operative recovery and providing ongoing support.
Our reflective framework addresses the aforementioned issues by promoting a more structured approach to near miss incident evaluation, providing adequate time for reflection, and ensuring that reflective actions are followed up on. The framework also emphasises inclusivity and encourages junior medical staff to contribute their thoughts and ideas during reflective sessions. This is done through the dual-phase structuring of reflection where individual reflection is initially encouraged, followed by a separate meeting where collective inputs are collated, and a plan of action reached.
Together, the doctors and AHPs collaborate to provide the best possible care to patients, drawing on their diverse perspectives and experiences. Through ongoing reflection and critical analysis, the team can identify areas for improvement and work to enhance the quality and safety of care delivery.
It is for this reason that we conducted separate and independent interviews from each healthcare professional to avoid any subconscious biases which may have arisen in the presence of senior influences. We propose a novel method of reflective practice as a standard to be replicated in future reflections as it provides a stringent, non-pressurised environment to achieve the most authentic feedback (Figure 1).

Clinical vignette
Our patient, a 60-year-old woman, was admitted for an elective resection of a right sided exophytic liver tumour. Computer tomography (CT) suggested that the lesion was an HCC, arising from liver segments V and VI, measuring approximately 12 cm (Figure 2). The patient had a good functional reserve for her age, with no significant past medical history.

On opening of the abdominal cavity, however, a distressing finding presented itself to the team, a large volume of intraabdominal blood. These circumstances are rarely observed during elective procedures. The extensive preparation, medical imaging and investigations obtained prior to ‘knife-to-skin’ gave the team a degree of certainty regarding the internal pathology which then allowed them to classify the case as a non-urgent elective case. Nevertheless, every so often, patients can present with an unexpected finding. The anaesthetist immediately obtained a venous blood gas sample and identified a significant fall in haemoglobin, consistent with acute haemorrhage. On closer inspection the source was identified, a spontaneous rupture of the tumour. Given that the patient’s preoperative haemoglobin, taken a few days prior to surgery, was within the reference range, the haemorrhage was concluded to have commenced within the past few days (Figure 3).
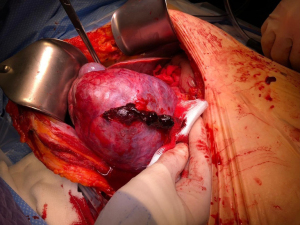
The team diverted from the original surgical plan immediately, implementing procedures to achieve haemostasis. Almost simultaneously, the team collectively started to wonder how the patient had managed to get to the hospital and appear well with this level of bleeding. Normally a major intraabdominal haemorrhage would be an emergency and signs of an acute abdomen would be starkly apparent. After receiving two units of red cells, the patient’s blood pressure stabilised, and the tumour stopped bleeding. The team continued with the resection and closed the abdomen shortly thereafter. The estimated total blood loss was 1,500 mL.
Later that day, the patient was informed of the intraoperative findings. It was then that she recounted that the day prior to her surgery she had suffered sudden and severe abdominal pain and vomiting, together with two episodes of syncope at home. Then, just as suddenly as the symptoms had appeared, they abated, except for an ongoing discomfort in her abdomen. The patient explained that a search on the NHS England website had yielded little information in keeping with her symptoms and thus she had attributed them to anxiety about the next day’s operation (11). This case has been discussed at length by the clinical team, and at each level of experience both specific and generalisable lessons have been drawn.
Implementing the framework to this case
This case acted as a trial of how surgical reflection could be conducted using a structured framework, in attempt to improve learning and outcomes. The structured framework involved both individual and collective reflection, providing a unique approach to identifying areas for improvement in patient care.
Each member of the surgical team, including the anaesthetic doctors and AHPs, began by reflecting on their individual experiences and observations; this would include evaluating their own actions, decision-making processes, and outcomes in the specific case. The individual reflections were shared and discussed in a safe and protected environment, providing a forum for team members to gain insight into differing viewpoints and foster a shared understanding of the event. A dedicated 45-minute time slot was reserved for this group discussion, with the surgical consultant serving as the meeting chair, but for administrative purposes only. It was emphasised that this role did not impose authority on the validity of members’ input and was solely to ensure a structured and organised discussion. Once members had gained confidence in the structure, it was proposed that the chair be alternated. The team then worked together to agree on a collective response and plan of action. During this stage of the process, the chair made a conscious effort to avoid directional interference in the team’s efforts to reach a summary. Instead, they would utilise open-ended prompts and neutral terms when signalling a move to work towards a collective goal. This collective reflection helped identify areas for improvement and lead to the development of a shared understanding of the best practices for patient care. By combining individual and collective reflection, this framework encourages a culture of continuous learning and improvement among the surgical team and minimises the cognitive biases such as overconfidence, anchoring, and confirmation bias, three types of bias which have been previously associated with overinflated perceptions of ability, and inaccurate risk-benefit estimations (12). A synopsis of three members of the larger team have been provided below for reference.
The surgical consultant
As the consultant, the ultimate responsibility for any patient and the outcome of a surgical procedure lies with us. In this particular situation, our first assumption was that the bleeding was iatrogenic, perhaps caused by a momentary lapse in concentration. Good surgical practice involves maintaining one’s composure and acting as an example for the rest of the team, hence preparing them to deal with similar situations proficiently in their future independent practice. We must utilise all members of our team to deal with crises efficiently. Often the most senior colleague to hand is the consultant anaesthetist. In this case, the anaesthetist was informed of the findings and promptly began investigations, allowing the surgical team to continue with the operation and locate the source of bleeding. To the team’s relief, further exploration revealed that the haemorrhage was secondary to a previous spontaneous rupture of the tumour, rather than iatrogenic damage at the time of operation. Almost immediately, however, that relief morphed into a sense of urgency and discomfort as the magnitude of the event became clear to us. It was unlikely that this bleeding had been asymptomatic, so our collective question remained: why had the patient not sought attention sooner?
Later, our assumptions were proven correct, the patient had indeed experienced relatively severe symptoms. She explained that following an online search and failing to have read of any such pre-operative complication, she had attributed her symptoms to pre-operative nerves. This immediately prompted a reconsideration of how to counsel patients with HCCs in the future. On the one hand, spontaneous ruptures in such tumours are rare, even as a consultant hepatopancreatobiliary (HPB) surgeon one may only see this condition a handful of times in a career. Seemingly, this is a shared opinion across the country as the NHS website fails to mention this complication and it is not common practice amongst colleagues in other trusts to counsel patients about this risk. On examining the evidence, however, between 3–15% of HCCs are reported to undergo spontaneous haemorrhage, with potentially disastrous consequences (8). What appears rare to the individual clinician, is in reality a relatively common event with potentially disastrous consequences. Furthermore, mortality rates following ruptured liver tumours range from 33–100% (13). A sudden recognition of a discrepancy between the evidence and one’s own practice was no comfortable realisation, which opens the question of how we should respond.
The surgical registrar
Surgical registrars are exposed to a large number of standard surgical procedures, particularly those which span a wide range of surgical subspecialties, such as a laparotomy. These surgical cases build on one another to form a cumulative foundation and allows us to develop an understanding of what to view as ‘normal’ and likewise ‘abnormal’. In this case, it quickly became apparent that the findings inside the patient’s abdomen were anything but normal. We quickly began to ponder as to what the origin of this haemorrhage could have been. An iatrogenic injury is always a possibility, however, having closely observed the early stages of the operation we were almost certain that this was not the case. It is often the responsibility of the registrar to consent the patient prior to surgery—as was the case in this instance. During this rigorous and systematic process, a wide variety of preoperative complications and contraindications to surgery are screened for. With all protocols having been followed, it became apparent that this patient could not have suffered an intra-abdominal bleed prior to surgery without any signs of peritonism. In this moment, we became plagued by several questions, and our sense of shock was compounded by our understanding that, as highlighted by the literature, early presentation and intervention is the key to averting disaster in such cases (14). We knew, however, that the priority was to control the bleeding, proceed with the resection and deal with all our unanswered questions afterwards. Following recovery of the patient and learning that she had indeed suffered signs of peritonism, it became clear that our protocol for preoperative consent was not as robust as assumed. A large part of a surgical registrar’s day involves counselling and consenting patients. We are constantly grappling with the question of how to present information efficiently and how to describe risk in a realistic but responsible manner. Too much information risks overwhelming patients and generating anxiety, whilst too little may prevent patients from making properly informed decisions and would be contrary to our professional duties (15). With more experience, a subconscious and almost automated script for each procedure becomes established in our minds. Yet this case has jolted us; the ‘scripts’ we have developed are instead a work-in-progress, subject to constant revisions informed by experience.
The junior doctor
Foundation training is filled with learning experiences. With each day, there is a unique opportunity to see something that textbook medicine can rarely encapsulate. The certainty and comfort of medical school where ‘right’ answers were easy to come by, quickly gives way to the shifting sands of real-life clinical medicine. This is an uncomfortable transition and one which is often accompanied by insecurity; is there a right answer, are there multiple right answers or is it that we simply don’t know? In this instance it became immediately apparent that my seniors were equally discomfited by the fact that the patient had not sought help for their symptoms and had very nearly suffered disastrous consequences. Witnessing senior colleagues grappling with an unexpected finding, even after decades of practice, was in some ways reassuring, but also daunting. Reflecting on this case, however, has been tremendously helpful, demonstrating that even in the most complex and potentially distressing circumstances, employing a systematic and stepwise approach to managing the situation can help to tackle feelings of anxiety and uncertainty. Furthermore, through this case, we’ve became aware of the risk of spontaneous rupture in HCC and now feel confident in counselling patients about during pre-operative clinics. Taking a step back to reflect on this case has taught us a wider lesson, namely, that at every level of experience, our patient’s stories will plant the seeds of an evolving and responsive practice.
Conclusions
Our collective interrogation of this case has led to various insightful conclusions, both in relation to how evidence-based medicine should be communicated to patients, but also regarding the wider process of reflective practice and how it can be harnessed to improve clinical practice. For instance, this novel framework for reflection can be incorporated into current-day reflection sessions, such as morbidity and mortality (M&M) conferences, allowing healthcare professionals to engage in a more structured and focused reflection where they are actively encouraged to participate their individual thoughts more proactively compared to M&M conferences.
Following the group meeting held with the entire multidisciplinary team comprising of surgeons, junior doctors, anaesthetists and other AHPs, a collective response was reached. The team unanimously agreed that the incident was caused due to several flaws in the surgical process. We identified that there was a lack of rigorous pre-operative screening, which could have helped to identify potential complications before the surgery, including repeating a full abdominal examination on the patient prior to being sent to theatre. Within our team locally, it has been highlighted that a comprehensive screening process involving a thorough history, physical examination, and observations to be performed on each patient immediately prior to sending for theatre. Furthermore, the team found that the NHS website failed to provide a dedicated section on rupturing of liver tumours. Despite acknowledging that the purpose of this resource is not to be a comprehensive clinical information source, as a solution, the team recommended updating the website with accurate and up-to-date information. In the UK, the NHS website has become the repository for health information. It is here that patients are directed, promising as it does, trusted, evidence-based information. For the most part, this level of influence over health information should be celebrated, helping to provide clarity and to combat the proliferation of poor information which runs rampant on the internet (16). Yet, there is an undeniably flattening effect to the information such a generic website can hold. It goes back to the flaws of textbook medicine in comparison to the heterogeneity of clinical medicine; it cannot be expected to deal with nuance and relies heavily on statistics, which, by definition, may strip out the quirks of real-life experience, often only visible to experts in a particular field. On the day that the patient in question experienced severe abdominal pain, she went to this very site and found nothing to suggest she should be concerned and instead dismissed her symptoms as anxiety-induced somatic pain.
Understandably, the patient expressed concern about the fact that such a potentially severe complication could be omitted from the NHS’s web resources on liver tumours. Spontaneous rupture is both a potentially devastating complication, but, importantly, is also not as rare as one may assume. Its incidence is comparable with the rupture of abdominal aortic aneurysms, a complication which is widely taught at all levels of medical education and for which patient counselling is very well established. The nature of practicing evidence-based medicine is often to not heed the warnings contained within individual, and often rare, cases, preferring instead to focus on the bigger picture. From a public health perspective, this represents a reasonable approach to providing patient counselling, ensuring that essential information is provided without unnecessarily frightening patients with information about rare side effects (17). This is, however, a fine balance; with many patients stating that they would rather be told everything and be allowed to draw their own conclusions from this information (18,19).
In spite of this, the team fully acknowledged that it was their responsibility to inform the patient about the purpose and limitations of the NHS website. As a result, it had been suggested improving communication with patients during pre-operative consultations by advising the patient to mention anything out of the ordinary to the surgical team.
The lack of information may also be a function of the fact that liver tumours are relatively rare, and their rupture even more so. This being said, we have established that this can be a catastrophic and life-threatening event, which is in fact less rare than previously anticipated. By contrast, the convention of counselling patients with abdominal aortic aneurysms about the signs and symptoms of rupture is well established (20). We suspect that perhaps there has been an insufficient level of attention focused on the stories of patients’ with this condition, preventing us from knitting together their experiences and revealing the patterns contained within them. Had we paid more attention to these cases and discussed them with our colleagues, we may have developed a more stringent counselling approach. In response to this reflection, we have discussed our findings with colleague at NHS England, to suggest that the webpage for liver tumours be updated with these amendments taken into account. In this instance, our colleagues at the NHS have responded and advised that complications of cancers can be wide ranging and often too lengthy to list on their website in detail. However, should the body of medical evidence shift significantly, to a degree where it is mentioned by national guidelines produced by the National Institute for Health and Care Excellence (NICE), other clinical policy teams, or clinical bodies such as the Royal Colleges, they would consider the information to be included on their website. Currently the body of evidence regarding spontaneous haemorrhage in HCCs is too sparse and the addition of our case study provides too little weighting to shift a change in the national website (21). Despite this, however, our local team have ensured that information pamphlets are provided to all patients diagnosed with HCC. These leaflets include information regarding major complications such as rupture, and signs to look out for which may alert clinicians in a timelier fashion.
The wider narrative which can be drawn from this case is that a system of reflective practice should be imposed as an integral part of any clinical team. This process must begin with the ability to identify when an incident is significant enough to trigger reflection. This should typically be the role of the consultant, as their experience and knowledge can pay dividend in triaging cases which provide most benefit for the team to reflect on. However, this is not to say that other healthcare professionals should be excluded from raising concerns, but rather empowered to do so. Once identified, the severity of the incident should be categorised, and all parties involved should be informed. The severity will allow healthcare professionals to gain a brief overview of how important and in-depth their reflection should be in this case and how significantly they should focus on implementing changes. Thereafter, all healthcare professionals involved should be encouraged to reflect individually, allowing them time to consider the case in a non-judgmental manner, away from the influence of seniors. Once this is complete, the team can then discuss the case collectively and reach a plan of action on how to proceed. Not all incidents will require intervention, just the act of reflecting will be of benefit.
However, when intervention is warranted, this must be carefully organised, and should take into account whether the intervention should be local or national, what exactly the intervention should entail, who it focusses on, where it should be publicised, and the financial and administrative logistics of implementation (Figure 4).

The implementation of this novel framework in our own practice has highlighted several limitations both to the framework specifically, and to reflective practice as a whole. To minimise the potential risks to both working relationships and patient safety, it is imperative to address these limitations proactively. Firstly, the tone and approach brought by individuals to the reflective workspace must be considered. There is a significant risk of introducing a culture of blame and scrutiny, which can negatively impact the integrity of the team-dynamic within the hospital and ultimately harm patient care. Therefore, it is essential to remind and encourage all healthcare professionals to maintain a respectful approach and implement a zero-tolerance policy to bullying during these meetings. Secondly, it is apparent that conducting rigorous and detailed reflective meetings regularly is a time and resource-intensive process. Adequate planning and preparation are required, and staff must be encouraged to organise their individual thoughts beforehand, which may not always be a requirement in traditional M&M conferences that mainly encourage collective reflection. Furthermore, a limitation in our single-case analysis of this framework is that the reflections of the anaesthetic colleagues, in addition to AHPs such as nurses was not formally reported in this paper, despite their inputs being collated and acknowledged both individually and collectively in reality. Despite this, it still remains an area for improvement for future studies looking into the same topic.
Nonetheless, we are confident that with a thorough understanding of how to minimise these risks, the new framework for reflection can have a significant positive impact on patient care.
Whatever the roots of this oversight, one clear thread has drawn itself through our experience and reflection of this case. Regardless of clinical seniority, a renewed recognition that being sensitive clinicians entails not only treating the patient’s complaints, but learning, as Rita Charon has said, to practice medicine is to be “fortified by narrative competence…to recognize, absorb, metabolize, interpret, and be moved by stories of illness” (22). One call to action from this story is clear, that we must be willing to counsel our patients about this potential complication and we must ensure that information about it is widely available. But there is a subtler demand being made; that clinicians in receipt of stories must share what they hear and be willing to change their practice even in the face of even ‘rare’ events.
Acknowledgments
The authors would like to pass on their many thanks to the patient involved in modelling this case of reflective practice.
Funding: None.
Footnote
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-8/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-8/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Explicit, informed consent was obtained from the patient regarding the use of their case, albeit anonymised, in this report.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sarker SK, Vincent C. Errors in surgery. Int J Surg 2005;3:75-81. [Crossref] [PubMed]
- McGlinn EP, Chung KC. A pause for reflection: incorporating reflection into surgical training. Ann Plast Surg 2014;73:117-20. [Crossref] [PubMed]
- Koshy K, Limb C, Gundogan B, et al. Reflective practice in health care and how to reflect effectively. Int J Surg Oncol (N Y) 2017;2:e20. [Crossref] [PubMed]
- Mantzourani E, Desselle S, Le J, et al. The role of reflective practice in healthcare professions: Next steps for pharmacy education and practice. Res Social Adm Pharm 2019;15:1476-9. [Crossref] [PubMed]
- Gupta DM, Boland RJ Jr, Aron DC. The physician's experience of changing clinical practice: a struggle to unlearn. Implement Sci 2017;12:28. [Crossref] [PubMed]
- Peshkepija AN, Basson MD, Davis AT, et al. Perioperative self-reflection among surgical residents. Am J Surg 2017;214:564-70. [Crossref] [PubMed]
- Aggarwal S, Qamar A, Sharma V, et al. Abdominal aortic aneurysm: A comprehensive review. Exp Clin Cardiol 2011;16:11-5. [PubMed]
- Pinal-García DF, Nuño-Guzmán CM, Gómez-Abarca A, et al. Spontaneous Rupture of Hepatocellular Carcinoma in a Young Patient with Fatal Outcome. Case Rep Gastroenterol 2018;12:19-26. [Crossref] [PubMed]
- Gathu C. Facilitators and Barriers of Reflective Learning in Postgraduate Medical Education: A Narrative Review. J Med Educ Curric Dev 2022;9:23821205221096106. [Crossref] [PubMed]
- LibGuides: Reflective Practice Toolkit: Barriers to reflection. Available online: https://libguides.cam.ac.uk/reflectivepracticetoolkit/barriers
- What is liver cancer. Available online: https://www.nhs.uk/conditions/liver-cancer/
- Armstrong BA, Dutescu IA, Tung A, et al. Cognitive biases in surgery: systematic review. Br J Surg 2023;110:645-54. [Crossref] [PubMed]
- Tan FL, Tan YM, Chung AY, et al. Factors affecting early mortality in spontaneous rupture of hepatocellular carcinoma. ANZ J Surg 2006;76:448-52. [Crossref] [PubMed]
- Xia F, Ndhlovu E, Zhang M, et al. Ruptured Hepatocellular Carcinoma: Current Status of Research. Front Oncol 2022;12:848903. [Crossref] [PubMed]
- Palmboom GG, Willems DL, Janssen NB, et al. Doctor's views on disclosing or withholding information on low risks of complication. J Med Ethics 2007;33:67-70. [Crossref] [PubMed]
- Suarez-Lledo V, Alvarez-Galvez J. Prevalence of Health Misinformation on Social Media: Systematic Review. J Med Internet Res 2021;23:e17187. [Crossref] [PubMed]
- Givel JC, Meier B. How much information do patients want or need. World J Surg 2014;38:1610-3. [Crossref] [PubMed]
- Kennedy BM, Rehman M, Johnson WD, et al. Healthcare Providers versus Patients' Understanding of Health Beliefs and Values. Patient Exp J 2017;4:29-37. [Crossref] [PubMed]
- Ziegler DK, Mosier MC, Buenaver M, et al. How much information about adverse effects of medication do patients want from physicians? Arch Intern Med 2001;161:706-13. [Crossref] [PubMed]
- Knops AM, Ubbink DT, Legemate DA, et al. Information communicated with patients in decision making about their abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 2010;39:708-13. [Crossref] [PubMed]
- Sahu SK, Chawla YK, Dhiman RK, et al. Rupture of Hepatocellular Carcinoma: A Review of Literature. J Clin Exp Hepatol 2019;9:245-56. [Crossref] [PubMed]
- Charon R. What to do with stories: the sciences of narrative medicine. Can Fam Physician 2007;53:1265-7. [PubMed]
Cite this article as: Soleimani-Nouri P, Holtermann Entwistle O, Fehervari M, Spalding D. A novel framework for surgical reflection. Ann Laparosc Endosc Surg 2023;8:20.


