Open versus laparoscopic splenectomy a meta-analysis of larger series
Introduction
Sutherland and Burghard made the first description of splenectomy in 1910. Laparoscopic splenectomy (LS) was first described in 1995 by Poulin et al. for a splenic trauma (1). Minimally invasive surgery for elective splenectomy has become a routine procedure in all laparoscopic centers. Since then, this technique was increasingly used and has quickly become referred to as the gold standard of treatment in cases of elective. After first case series, many groups has published comparative studies between open and laparoscopic approach.
For this purpose, a meta-analysis investigating comparative studies of open versus laparoscopic approach for splenectomy was performed. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/ales-20-90).
Methods
A systematic review of the current literature was made up to December 2019. The search strategy was under the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) guidelines, as well as PRISMA for abstracts. We searched the electronic databases MEDLINE-PubMed using the following items: (splenectomy) AND (laparoscopic OR minimally invasive) AND (versus OR compar*) AND (open OR traditional OR laparotomic).
The inclusion criteria were as follows: papers written in English, comparing two groups (open and laparoscopic), and containing surgical data of the two procedures.
Papers were excluded according to the following criteria: sufficient statistical details, review articles, nonclinical studies, letters, expert opinions, conference summaries, and case reports. All kinds of manuscripts were reviewed, and we included the only studies with a laparoscopic group number ≥50 cases.
Data extraction
Two authors reviewed and extracted data from all included studies. In case of disagreement, the paper was discussed by all the authors. For each study, the following characteristics were collected: first author name, year of publication and reference, number of patients, surgical duration, length of hospital stay, morbidity, and mortality.
Statistical analysis
Values are presented in descriptive statistics. Statistical analysis was performed using the Statistical Package for the Social Sciences version 22.0 (SPSS Inc., Chicago, IL, US). Meta-analyses of RCTs were performed using Review Manager 5.3 (Cochrane Collaboration, Oxford, England). The drain effect was described by OR such that a given value <1 favors the presence of the drain. The weighted pooled ORs were calculated under the fixed effects model and reported with a 95% CI. Statistical heterogeneity was assessed by inspecting the forest plots and I2 statistics.
The Z-test for overall effect and its 2-sided P value were also assessed. Discrete variables were analyzed using the X2 or the Fisher exact test. Statistical significance was set at the 0.05 probability level.
Newcastle-Ottawa Quality Assessment Scale (NOS): studies with scores >6 were defined as high-quality studies. NOS details of each selected study were reported in Table 1.
Table 1
| Ref. | Selection | Comparability | Outcome | Quality Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case definition | Representativeness | Selection of controls | Definition of controls | Comparable for therapy | Comparable for etiology | Assessment of outcomes | Integrity of follow-up | ||||
| Rescorla 1998 (2) | * | * | * | * | * | * | No | * | ******* | ||
| Park 1999 (3) | * | * | * | * | * | * | * | * | ******** | ||
| Qureshi 2005 (4) | * | * | * | * | * | * | No | * | ******* | ||
| Goers 2008 (5) | * | * | * | * | * | * | No | * | ******* | ||
| Zhu 2009 (6) | * | * | * | * | * | * | * | * | ******** | ||
| Deeb 2012 (7) | * | * | * | * | * | No | * | * | ******* | ||
| Ahad 2013 (8) | * | * | * | * | * | * | * | * | ******** | ||
| Ardestani 2013 (9) | * | * | * | * | * | No | * | * | ******* | ||
| Musallam 2013 (10) | * | * | * | * | * | * | No | * | ******* | ||
| Zhe 2013 (11) | * | * | * | * | * | * | No | * | ******* | ||
| Casaccia 2019 (12) | * | * | * | * | * | No | * | * | ******* | ||
| Utria 2019 (13) | * | * | * | * | * | * | * | * | ******** | ||
Results
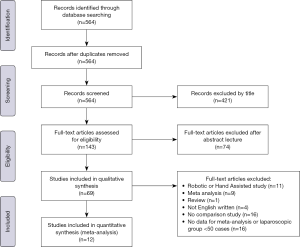
The literature search, performed until December 31, 2019, identified a total of 564 records. Four hundred twenty-one records were excluded according to the title. One hundred forty-three abstract records were screened, and seventy-four records were then excluded. Sixty-nine studies were included in the qualitative synthesis. Fifty six records were excluded after review: Robotic or Hand Assisted study (n=11), Meta-analysis (n=9), Review (n=1), Not English written (n=4), No comparison study (n=16), No data for meta-analysis or laparoscopic group <50 cases (n=16). After full-text analysis, twelve studies were included in the meta-analysis (2-13). PRISMA flow diagram is represented in Figure 1.
Eventually, twelve articles were identified, with a total of 5,058 LS and 3,229 OS (Table 2).
Table 2
| Ref | Number | Operative time | Morbidity | Mortality | Length of stay | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vls | Open | Vls | Open | Vls | Open | Vls | Open | Vls | Open | |||||
| Rescorla 1998 (2) | 50 | 32 | 115 | 83 | – | – | 0 | 0 | 1.4 | 2.5 | ||||
| Park 1999 (3) | 147 | 63 | 145.1 | 77.3 | 10.2% | 34.9% | 0 | 0 | 2.4 | 9.2 | ||||
| Qureshi 2005 (4) | 81 | 59 | 231 | 138 | – | – | 0 | 1 | 2.4 | 4.1 | ||||
| Goers 2008 (5) | 98 | 42 | 158 | 152 | – | – | – | – | 2.9 | 5.4 | ||||
| Zhu 2009 (6) | 81 | 135 | 174 | 156 | 27.2% | 25.2% | 0 | 0 | 8.2 | 11.9 | ||||
| Deeb 2012 (7) | 991 | 592 | – | – | 13.2% | 25.8% | 19 | 18 | 3.7 | 7.4 | ||||
| Ahad 2013 (8) | 1,644 | 851 | 119 | 103 | 12% | 24% | 22 (1.4%) | 27 (3.3%) | 3 | 6 | ||||
| Ardestani 2013 (9) | 267 | 372 | 142 | 108 | 17.6% | 31.5% | (1.5%) | (4%) | 3 | 5 | ||||
| Musallam 2013 (10) | 874 | 907 | 138 | 125 | – | – | (1.4%) | (4.6%) | 3 | 6 | ||||
| Zhe 2013 (11) | 80 | 73 | 254 | 234 | – | – | 3 (3.8) | 3 (4.1) | 10.1 | 14.4 | ||||
| Casaccia 2019 (12) | 132 | 43 | 143 | 112 | 15.1% | 20.9% | 1 (1.5%) | 4 (9.3%) | 6 | 9 | ||||
| Utria 2019 (13) | 613 | 60 | 120 | 133 | 12.4% | 23.3% | 0 | 1 (1.7%) | 2 | 4 | ||||
As for the quality of the reported studies, all the investigated articles were retrospective cohort studies. Four studies had a NOS score of eight and the others 8 studies presented NOS value of seven (Table 1).
Two studies come from China (6,11), one from Italy (12) and nine from the USA (2-5,7-10,13). Eight studies were monocentric, and four used a national database. Four studies were focused on pediatric patients and the other eight on the adult population.
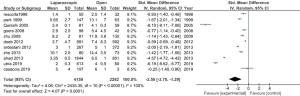
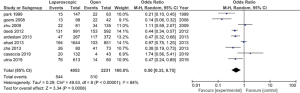
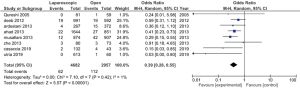
Operative time was higher for the laparoscopic group in all but one study. However, in the study from Utria (12), the difference between the two groups was not statistically significant. Ten studies were included in the analysis. The random-effects meta-analysis showed a difference in favor of the open group (Figure 2). The length of stay was in eleven studies in favor of the laparoscopic group; one study does not report data on the length of hospital stay. According to these results, the random-effects meta-analysis showed a difference in support of the laparoscopic group (Figure 3). The morbidity was less frequent in the laparoscopic group in seven studies. The random-effects meta-analysis showed a difference in favor of the laparoscopic group (Figure 4). The mortality was higher in all studies in the open group (Figure 5). In this case, the heterogeneity test I2 =1%. The random-effects meta-analysis of mortality is reported in Figure 4. Results are grouped in Table 2.
Discussion
Laparoscopic splenectomy is a worldwide recognized procedure. Many Centers have reported their own experience comparing LS and OS. In the present study, we identify twelve comparative studies with the LS group >50 cases. Regarding the operative time, in all but one, LS was longer than OS. A well-standardized technique explains these interesting results for the OS. LS, which was described first in 1995, need a learning curve. Only two articles were recent, the others were published in 2013 or earlier, reporting retrospective data. A recent prospective study in a high volume Center report a minor surgical time in the LS group (13), suggesting a reduced operative due to the high experience. The heterogeneity test I2 was high for the surgical time; this can be explained by the main difference of monocentric and national studies for the cohort number. The study of Utria was in favor of LS, using the American College of Surgeons National Surgical Quality Improvement Program Pediatric (12).
As expected, concerning the length of stay, the laparoscopic group has shorter hospital stay than the open group. However, as for the surgical time, the heterogeneity test I2 was high. As previously, this can be explained with the high difference in the group’s numerosity in all studies. The morbidity was less frequent in the laparoscopic group. This result is explaining by the minimal invasiveness surgery. The extraction of the specimen in laparoscopy is mostly a Pfannenstiel access, which limits post-operative pain. Mortality was more frequent in the open group, with a heterogeneity test I2 =1%. To summarize the above results, the laparoscopic approach for splenectomy have better outcomes in terms of morbidity and mortality. Moreover, the length of stay is shorter in a patient treated in the laparoscopic group.
The main limitation of our study is the non-heterogeneity of all studies. The increasing use of a minimally invasive approach will undoubtedly decrease the difference in operative time and improving morbidity and mortality.
In conclusion, laparoscopic splenectomy is a safe procedure comparing to an open approach with fewer complications and less post-operative mortality. The gain of shorter hospital stay associated with the good outcomes suggests performing splenectomy by a laparoscopic procedure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Minimally Invasive Spleen Surgery”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/ales-20-90
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-90). The series “Minimally Invasive Spleen Surgery” was commissioned by the editorial office without any funding or sponsorship. Giovanni Battista Levi Sandri and Massimo Carlini served as the unpaid Guest Editors of the series. Giovanni Battista Levi Sandri serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Jun 2019 to May 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Poulin EC, Thibault C, DesCôteaux JG, et al. Partial laparoscopic splenectomy for trauma: technique and case report. Surg Laparosc Endosc 1995;5:306-10. [PubMed]
- Rescorla FJ, Breitfeld PP, West KW, et al. A case controlled comparison of open and laparoscopic splenectomy in children. Surgery 1998;124:670-5; discussion 675-6. [Crossref] [PubMed]
- Park A, Marcaccio M, Sternbach M, et al. Laparoscopic vs open splenectomy. Arch Surg 1999;134:1263-9. [Crossref] [PubMed]
- Qureshi FG, Ergun O, Sandulache VC, et al. Laparoscopic splenectomy in children. JSLS 2005;9:389-92. [PubMed]
- Goers T, Panepinto J, Debaun M, et al. Laparoscopic versus open abdominal surgery in children with sickle cell disease is associated with a shorter hospital stay. Pediatr Blood Cancer 2008;50:603-6. [Crossref] [PubMed]
- Zhu JH, Wang YD, Ye ZY, et al. Laparoscopic versus open splenectomy for hypersplenism secondary to liver cirrhosis. Surg Laparosc Endosc Percutan Tech 2009;19:258-62. [Crossref] [PubMed]
- Deeb AP, Kim MJ, Fleming FJ, et al. The impact of operative approach in elective splenectomy: a multivariate analysis of outcomes from the NSQIP database. Surg Laparosc Endosc Percutan Tech 2012;22:415-9. [Crossref] [PubMed]
- Ahad S, Gonczy C, Advani V, et al. True benefit or selection bias: an analysis of laparoscopic versus open splenectomy from the ACS-NSQIP. Surg Endosc 2013;27:1865-71. [Crossref] [PubMed]
- Ardestani A, Tavakkoli A. Laparoscopic versus open splenectomy: the impact of spleen size on outcomes. J Laparoendosc Adv Surg Tech A 2013;23:760-4. [Crossref] [PubMed]
- Musallam KM, Khalife M, Sfeir PM, et al. Postoperative outcomes after laparoscopic splenectomy compared with open splenectomy. Ann Surg 2013;257:1116-23. [Crossref] [PubMed]
- Zhe C, Jian-wei L, Jian C, et al. Laparoscopic versus open splenectomy and esophagogastric devascularization for bleeding varices or severe hypersplenism: a comparative study. J Gastrointest Surg 2013;17:654-9. [Crossref] [PubMed]
- Casaccia M, Sormani MP, Palombo D, et al. Laparoscopic Splenectomy Versus Open Splenectomy In Massive and Giant Spleens: Should we Update the 2008 EAES Guidelines?. Surg Laparosc Endosc Percutan Tech 2019;29:178-81. [Crossref] [PubMed]
- Utria AF, Goffredo P, Keck K, et al. Laparoscopic Splenectomy: Has It Become the Standard Surgical Approach in Pediatric Patients? J Surg Res 2019;240:109-14. [Crossref] [PubMed]
Cite this article as: Levi Sandri GB, Spoletini D, Tarantino G, Carlini M. Open versus laparoscopic splenectomy a meta-analysis of larger series. Ann Laparosc Endosc Surg 2020;5:36.