Laparoscopic management of acute presentations of obstructed, congenital, diaphragmatic hernias in adults: case reports
Introduction
Diaphragmatic hernias can be divided into congenital and acquired. 1/2,500 of new-borns have a congenital diaphragmatic hernia (CDH) (1). This results when there is incomplete formation of the diaphragm during embryogenesis, and consequently the abdominal viscera herniates into the thorax. An acquired diaphragmatic hernia (ADH) has an incidence of <5% and usually result from a direct penetrating injury (~65%) such as gunshot or stab injuries, or blunt abdominal trauma (~35%) such as road traffic accidents or falls (2).
A diaphragmatic hernia can occur at the oesophageal hiatus (sliding and paraoesophageal hiatal hernias), in the posterolateral region (Bochdalek’s hernia), or in the parasternal region (Morgagni-Larrey). Morgagni-Larrey hernias account for only 3% of all diaphragmatic hernias (3) and 70% of patients are female (4). It is a congenital anomaly that arises due to a para-retrosternal defect between the septum transversum and sternum. In 95% of patients the transverse colon and omentum herniate into a sac within the thorax (5). The hernia occurs mostly on the right side, accounting for 90% of cases (6). Left sided cases may be less common due to the pericardial attachment to the diaphragm. Morgagni’s hernia often refers to those occurring on the right, whilst Larrey’s hernia refers to those on the left (4). An early review article reported only 93 case reports on adults (7).
Bochdalek hernia is the commonest CDH, with an incidence of up to 6%. An early review reported only 100 symptomatic cases in adults in world literature (8). It results from failure of proper fusion of the posterolateral diaphragmatic foramina, with the defect generally located just superior to the adrenal gland (9). In contrast to Morgagni-Larrey’s, the majority of Bochdalek-type hernias occur on the left side (85%), with a lower number on the right side (13%) and bilateral (2%) (1), and are more common in the male population (57%) (9).
Cardiac anomalies are most commonly associated with CHD. 10% of patients have chromosomal abnormalities (4) and a relationship has also been described with developmental disorders (10). Adult associations further include obesity, trauma, weight lifting, or other causes of increased intra-abdominal pressure.
Case presentation
Case report 1: Morgagni hernia
Patient information
We present a case of a 62 years old gentleman who was admitted with severe abdominal pain, which began 4 days prior to admission, associated with vomiting and one episode of diarrhoea. Past medical history included bariatric surgery—a Roux-en-Y gastric bypass 12 years ago, and a total hip replacement. The patient lived in supported accommodation due to poor mobility albeit with no carers.
Clinical findings
On examination, there was central and epigastric tenderness with voluntary guarding. There was reduced air entry in the right lower zone with mild increased work of breathing. Heart sounds were normal and the patient was well perfused.
Timeline
Please find timeline of the events of the Morgagni Hernia case study in Box 1.
Table 1
| Variable | Minimally invasive approach | Open repair |
|---|---|---|
| Average hospital-stay | 4 days | 14 days |
| Complication rates | 5% | 17% |
| 30-day morbidity rates | 0% | 3% |
Diagnostic assessment
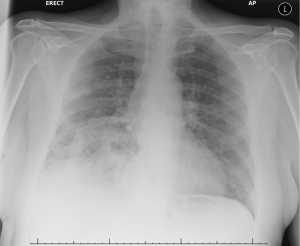
Blood results revealed raised inflammatory markers. A chest x-ray was done as the primary investigation (Figure 1) and an abdominal and pelvic CT scan confirmed proximal small bowel obstruction with a transition point within a large right-sided diaphragmatic hernia of Morgagni (Figure 2). Reactive free fluid suggested strangulation and probably resultant chest aspiration.
Therapeutic intervention
The patient was started on IV antibiotics, fluids and proton pump inhibitor (PPI). A nasogastric (NG) tube was inserted. Laparoscopic repair of the hernia of Morgagni took place on day 4 of the admission. Laparoscopic ports were inserted as shown in Figure 3.
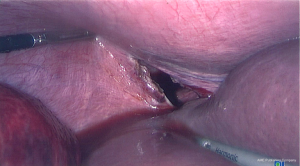
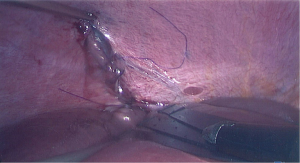
Intra-operatively, a large Morgagni hernia was found lying to the right of the falciform ligament with a neck of approximately 9 cm diameter containing small bowel, large bowel and omentum within the hernial sac (Figure 4). Previous Roux-en-Y surgery was visualised and appeared satisfactory. To perform the repair, the hernial sac contents were reduced into the peritoneal cavity. This was an easy reduction to achieve in this patient. The hernial sac was partially reversed. Primary closure of the defect was not possible and a 15 cm synthetic mesh (Symbotex, composite, round) was placed over the defect (Figure 5). Interrupted Prolene sutures were used to fix the mesh to the edges of the defect leaving 2–3 cm overlap. The abdomen was washed out with 1 litre of 0.9% saline and laparoscopic ports were removed under direct vision. A 20 F drain was placed in the right subphrenic position. There were no intra-operative complications and patient blood loss was minimal.
Postoperatively, the patient recovered well and was discharged on day 2 following the operation. He was initially on intravenous Tazocin, which was converted to oral Amoxicillin on discharge to complete a course at home. His drain was taken down on day 2 and he was clinically well on discharge with decreasing inflammatory markers.
Follow up
A CT of the abdomen and pelvis with contrast was performed 2 months following the surgery, where no evidence of hernia recurrence was found. At 3 months, examination was grossly unremarkable with soft abdomen and healed port site scars, and furthermore, no signs of recurrence.
Patient perspective (phone conversation)
The patient expresses frustration at previous diagnoses given for his symptoms, including food poisoning, which again highlights the importance of including CDH in the differential when assessing adults who present with similar symptoms. On reflection, he mentions that although waiting for the surgery was difficult, once he had the surgery, his pain was relieved leading to an early discharge.
Case report 2: Bochdalek hernia
Patient information
Fifty years old female presented with acute right upper quadrant pain and vomiting. She also felt she was working harder to breath. There was no significant past medical or social history.
Clinical findings
On examination, there were epigastric and right upper quadrant tenderness as well as guarding. There was reduced air entry in the right lower zone. Heart sounds were normal and she was well perfused. Observations revealed tachypnoea, with a rising heart rate.
Timeline
Please find timeline of the events of the Bochdalek hernia case study in Box 2.
Diagnostic assessment
Blood tests revealed high inflammatory markers. Abdominal CT demonstrated a strangulated diaphragmatic hernia on the right hemidiaphragm. There was herniation of small bowel under the right, medial arcuate ligament into the chest through the hernia described on CT (Figure 6).
Therapeutic intervention
IV co-amoxiclav was commenced and the patient was taken to theatre. On laparoscopy, the herniated small bowel was initially dusky in colour with some petechial and mesenteric haemorrhages but recovered following reduction of the hernia contents.
During the procedure, the neck of the hernia was tight. The arcuate ligament was divided and the loop of bowel reduced. The diaphragmatic defect was 4–5 cm in diameter (Figure 7). This was repaired by primary closure with the use of interrupted, polydioxanone sutures (Figure 8). The patient experienced a tension pneumothorax following closure, so a chest drain was inserted intra-operatively. A Redivac drain was inserted into the abdomen.
The patient had a 2-day, uneventful stay in the intensive care unit, following which, drains were removed and she was transferred to the surgical ward. There were no complications post-operatively and the patient mobilised well. They were discharged on the 6th post-operative day.
Follow up
A chest X-ray following surgery revealed no recurrence and resolution of the intraoperative pneumothorax. At 6-week follow up, despite a short ITU stay following the operation, the patient had a good course of recovery since discharge with no symptoms or signs of recurrence.
Patient perspective (extract from email from patient)
“The anaesthetist and surgeons came to see me before the operation and described the proposed procedure once more which helped to reduce the stress and worry of the situation. Following my operation, I was transferred to ICU where I had one to one nursing care, and following this, to an HDU ward. The nursing care I received whilst on both wards was brilliant. All of the nurses were professional, knowledgeable, kind and understanding, and were supported by a team of great health care assistants.
My pain was managed effectively, initially via a drip and manual pump and subsequently by regular medication once it was proving difficult to insert/maintain a canula. I was encouraged to become mobile once in HDU, and I feel this helped in speeding up the recovery process. I was discharged from hospital on Monday 24th June, having been shown how to monitor and empty the abdomen drain and was advised to follow a soft diet for 4 weeks.
[Months following surgery] I feel very well. I do not have any ongoing complications following the surgery and feel as well as I did before going into hospital.”
Discussion
Presentation
The presentation of a CDH varies depending on the degree of pulmonary hypoplasia and pulmonary hypertension that results from the abdominal contents herniating into the chest during embryological development. Patients can be asymptomatic with incidental findings, or present with severe respiratory and gastrointestinal symptoms, as well as haemodynamic instability (1). A Morgagni-Larrey hernia is often diagnosed early, but can sometimes remain unrecognised until adulthood usually in the absence of other associated developmental anomalies. Abdominal contents may not initially herniate through the diaphragmatic defect, leading to variable age of presentation. Literature (9) shows most common presenting symptoms of the Bochdalek-type hernia are abdominal.
Diagnosis
Diagnosis is made primarily through imaging. A Morgagni hernia diagnosis is confirmed by chest and abdominal computed tomography (CT). Although commonly used as a first line investigation a plain chest radiograph is not the preferred imaging modality because herniated abdominal contents are generally radiolucent (10). A plain chest radiograph may, however, reveal a particular bowel gas pattern, air-fluid level in thoracic cavity, varied lucency in the chest, or deviation of the heart and mediastinum (5). Other diagnostic modalities that may assist when the CT is equivocal or alternative diagnoses are considered include oesophagogastroduodenoscopy (OGD), barium study, gastrografin study and magnetic resonance imaging (MRI) (10). An ultrasound of the chest may also be useful, where suspected (5).
Emergency cases
Examples from current literature of emergency diaphragmatic hernia cases resulting in definitive laparoscopic surgery are few, as the majority of complex cases require open surgery. Nevertheless, few reports include presentation of breathlessness and dysphagia in a 73-year-old, where CT found herniated stomach in the chest and the defect was repaired with a mesh with an uneventful post-operative course (1). Another reported case is of a 42-year-old who presented with abdominal pain and pneumothorax secondary to trauma and CT revealed left diaphragmatic hernia, where the laparoscopic approach was used for reduction and repair with composite mesh fixed with absorbable tackers (6). In emergency cases with compromised bowel i.e., ischaemic bowel requiring resection (1), an open approach is commonly required. This correlates with our case reports, where there was no ischaemic bowel in both patients, allowing for laparoscopic approach.
Prognosis
In late-presenting CDH, survival rates vary between 97 and 100% following correct diagnosis (5). This is in contrast to neonatal CDH, where the predicted survival rate is 68% (11). Herniation of abdominal contents poses the potential risk of strangulation leading to bowel ischaemia or perforation (10).
Management
Surgery is the preferred method of treatment for diaphragmatic hernia. It can be performed through a laparoscopic, thoracoscopic, transthoracic, transabdominal, or open approach (6). The minimally invasive laparoscopic or thoracoscopic approaches are preferred due to lower morbidity and complication rates (Table 1) (12).
This paper discusses the laparoscopic approach in emergencies in adults.
The current literature does not advise on absolute indications or timing of surgery. However, if complications such as bowel obstruction occur, emergency surgery is recommended. Delay in intervention is associated with significant mortality and morbidity (1).
There is little consensus on the optimum surgical technique for laparoscopic repair of diaphragmatic hernia. Following reduction, repair of the diaphragmatic defect can be achieved with the use of sutures for primary closure or with combined use of a synthetic or biological mesh to cover the defect. Mesh repair is used when the defect is too large for primary closure (1). Primary closure can lead to significant tissue tension and mesh placement is associated with a reduced rate of recurrence (13).
One technique is to bring the diaphragm to the anterior abdominal wall using a series of incisions inferior to the lower costal border and sutures, followed by tacking a composite mesh to the diaphragm to reinforce this closure. This technique leads to good recovery post-operatively with no recurrences in the small sample trialled (14). There is also description of suturing a mesh in place intracorporally, over a defect too large for primary closure without the need for separate skin incisions (15). Another technique involves use of a stapled Marlex patch of mesh to close the diaphragmatic defect (16).
A recent report described a technique where defect closure was achieved with intermittent, extra-abdominal, transfascial, non-absorbable sutures with pledgets, suturing the posterior rim to the anterior abdominal wall’s full thickness, without the use of any prosthesis. The outcomes were early discharge, no complications and asymptomatic follow up at 3 months (17).
In another case, in the absence of sufficient innate diaphragmatic muscle for a primary closure following removal of the sac, 3 interrupted sutures were placed in the anterior portion of a mesh which was positioned in the subdiaphragmatic space and reconstruction of the anterior diaphragm was performed. 3 transfascial sutures then allowed for the mesh to be brought to the anterior abdominal wall and interrupted endo stitch fixation to the native diaphragm was used for full coverage of the defect, whilst staples were used to enable layering of the mesh. Results were a smooth postoperative course with quick discharge and no recurrence of symptoms (18).
Controversies exist in the current literature on whether the hernia sac should be excised.
In some reports, retention of the sac is described with no obvious complications arising due to the remaining sac (7,19). There is concern that removal of the sac may lead to pneumomediastinum and damage to pericardium or mediastinal structures (3). Reports describing resection of the sac have also had good results (16,20). Excision of the sac may lead to reduced tissue trauma, fluid collection and recurrence (3).
There are limitations of the laparoscopic approach. On encountering intrathoracic adhesions, the laparoscopic approach may be difficult due to unfavourable angles between the instruments (13).
There is scope for robotic-assisted laparoscopic repair of diaphragmatic hernias. It offers many advantages including improved dexterity, 3D observation, seven degrees of freedom, elimination of physiologic tremors and a favourable ergonomic position (13).
Conclusions
Diaphragmatic hernias commonly present in childhood and are rare in adults. Diagnosis is confirmed with a chest and abdominal CT. Surgery is the preferred management approach employing laparoscopic techniques in the uncomplicated cases. There is a lack of standardisation currently when considering the best surgical technique for the procedure. This paper discusses two emergency cases in adults: one of a Morgagni hernia, and another of a Bochdalek hernia, where successful laparoscopic approach was used to reduce the hernias, remove their sac and repair the defect.
| Day 1: Presentation to ED | → | Medical management | → | Day 4: Laparoscopic management | → | Day 6: Discharge home | → | Follow up |
| Day 1: Presentation to ED | → | Day 1: Laparoscopic management | → | Day 4: Laparoscopic management | → | Day 1: Laparoscopic management | → | Follow up |
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.11.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. We presented the cases in accordance with the CARE Guideline.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Testini M, Girardi A, Isernia RM, et al. Emergency surgery due to diaphragmatic hernia: case series and review. World J Emerg Surg 2017;12:23. [Crossref] [PubMed]
- Amboss. Acquired Diaphragmatic Hernias. Available online: http://www.amboss.com/us/knowledge/Acquired_diaphragmatic_hernias.
- Godazandeh G, Mokhtari-esbuie F. Laparoscopic Repair of Morgagni Hernia: Three-Case Presentation and the Literature. Case Rep Surg 2016;2016:4268539 [Crossref] [PubMed]
- Arikan S, Dogan MB, Kocakusak A, et al. Morgagni’s Hernia: Analysis of 21 Patients with Our Clinical Experiemce in Diagnosis and Treatment. Indian J Surg 2018;80:239-44. [Crossref] [PubMed]
- Kim JM, Couluris M, Schnapf BM. Late-Presenting Left-Sided Morgagni Congenital Diaphragmatic Hernia in a 9-Year-Old Male. ISRN Pulmonology 2011; [Crossref]
- Ağalar C, Atila K, Arslan NÇ, et al. Adult Morgagni hernia: a single-center experience of five cases and a review of literature. Turk J Surg 2018;11:1-4. [Epub ahead of print]. [PubMed]
- Loong TP, Kocher HM. Clinical presentation and operative repair of hernia of Morgagni. Postgrad Med J 2005;81:41-4. [Crossref] [PubMed]
- Alam A, Chander BN. Adult Bochdalek Hernia. Med J Armed Forces India 2005;61:284-6. [Crossref] [PubMed]
- Machado NO. Laparoscopic Repair of Bochdalek Diaphragmatic Hernia in Adults. N Am J Med Sci 2016;8:65-74. [Crossref] [PubMed]
- Sanford Z, Weltz AS, Brown J, et al. Morgagni Hernia Repair: A Review. Surg Innov 2018;25:389-99. [Crossref] [PubMed]
- Downard CD, Jaksic T, Garza JJ, et al. Analysis of an improved survival rate for congenital diaphragmatic hernia. J Pediatr Surg 2003;38:729-32. [Crossref] [PubMed]
- Chen B, Finnerty BM, Schamberg NJ, et al. Transabdominal robotic repair of a congenital right diaphragmatic hernia containing an intrathoracic kidney: a case report. J Robot Surg 2015;9:357-60. [Crossref] [PubMed]
- Arevalo G, Harris K, Sadiq A, et al. Repair of Morgagni Hernia in Adults with Primary Closure and Mesh Placement: First Robotic Experience. J Laparoendosc Adv Surg Tech A 2017;27:529-32. [Crossref] [PubMed]
- Ryan JM, Rogers AC, Hannan EJ, et al. Technical description of laparoscopic Morgagni hernia repair with primary closure and onlay composite mesh placement. Hernia 2018;22:697-705. [Crossref] [PubMed]
- Nguyen T, Eubanks PJ, Nguyen D, et al. The Laparoscopic Approach for Repair of Morgagni Hernias. JSLS 1998;2:85-8. [PubMed]
- Rau HG, Schardey HM, Lange V. Laparoscopic repair of a Morgagni hernia. Surg Endosc 1994;8:1439-42. [Crossref] [PubMed]
- Costa Almeida C, Caroço TV, Nogueira O, et al. Laparoscopic repair of a Morgagni hernia with extra-abdominal transfascial sutures. BMJ Case Rep 2019;12: [Crossref] [PubMed]
- Stone ML, Julien MA, Dunnington DH Jr, et al. Novel laparoscopic hernia of morgagni repair technique. J Thorac Cardiovasc Surg 2012;143:744-5. [Crossref] [PubMed]
- Angrisani L, Lorenzo M, Santoro T, et al. Hernia of foramen of Morgagni in adult: case report of laparoscopic repair. JSLS 2000;4:177-81. [PubMed]
- Ridai M, Boubia S, Kafih M, et al. Larrey or Morgagni hernias treated by laparoscopy. Presse Med 2002;31:1364-65. [PubMed]
Cite this article as: Mittal A, Cay P, Singh K. Laparoscopic management of acute presentations of obstructed, congenital, diaphragmatic hernias in adults: case reports. Ann Laparosc Endosc Surg 2020;5:20.