Mini gastric by-pass and bridged mini gastric by-pass: what is new?
Introduction
With increasing living standards and decreasing physical activity, today’s people have had to deal with the problem of obesity. Between 1980 and 2008, the mean global body mass index (BMI) increased by 0.4–0.5 kg/m2 per decade for both men and women (1). Obesity and associated disorders such as type II diabetes, hypertension, lung problems reduce life expectancy and increase the importance of bariatric surgery. Long-term effects of diet, exercise and medical treatment on weight loss are not effective enough to manage morbid obesity. In the last years, mini gastric bypass (MGB) has been presented as an option of surgical treatment for obese patients to reduce operation time and avoiding eventual postoperative complications after Roux-en-Y gastric bypass (RnY) (2). MGB, is both malabsorptive and restrictive procedure, can be easily applied with a single gastrointestinal anastomosis and is seen as an ideal bariatric procedure that can be reversible with a significant superior effect on remission of type II diabetes compare to RnY.
In 1997, Robert Rutledge, a trauma surgeon at the University of North Carolina, conducted an operation that would later be described as MGB by performing gastrojejunostomy after antral resection of the stomach of a gunshot patient. This reconstruction leads to a longer small curvature and has superior results in morbidly obese patients (3). In this technique, the five trocars method is used. A small window is created for entering from the lesser sac at incisura angularis. The stapler is applied horizontally to the axis of the stomach through the window. Gastric tube about 60–80 mL is created by repeated application of stapler vertically upward to the angle of His. The jejunal segment, 150–200 cm from the Treitz ligament is brought up to the distal end of the gastric tube as ante colic end-to-side anastomosis was performed (Figure 1).
Why we need this modification of MGB?
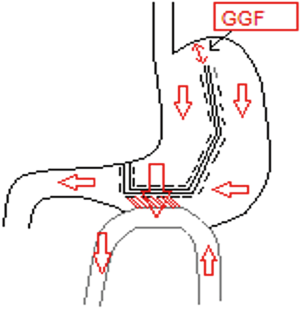
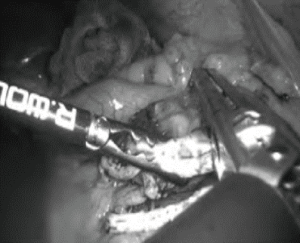
MGB has gradually become popular in bariatric surgery. The frequency of this technique has increased significantly in the last decade (4). In fact, in terms of etiology of obesity, the stomach and the small intestine are two innocent organs. However, they are irreversibly resected and destroyed. Trying to solve the problem of obesity by irreversible damaging these two innocent organs can be considered a crime against them. Moreover, in all bariatric bypassed procedures, there are still questions about the fate of the remnant stomach. After Roux-n-Y gastric bypass, carcinoma in the stomach and lower esophagus has been reported in 46 patients (5,6). In Taiwan where the incidence of gastric carcinoma is high, one carcinoma 9 years after MGB has been reported in the bypassed stomach (7). From the perspective of reversible and less damaging to stomach, we modified the previously described technique by leaving a bridge at the most cranial 2 cm of fundus such as artificial gastro-gastric fistula (GGF) and we would like to entitle this new technique as bridged mini gastric bypass (BGMB, Sumer’s technique) (Figure 2).
BMGB might be the most physiological and anatomical technique with weight loss and metabolic effects as much as MGB. Moreover, via GGF, BMGB allows endoscopic procedures, especially in the remnant stomach.
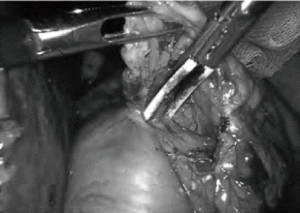
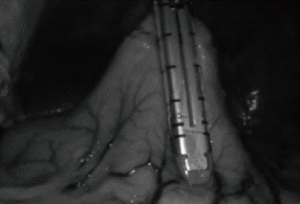
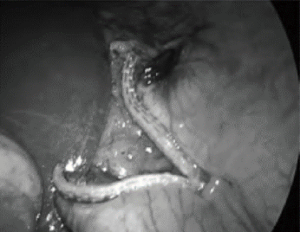
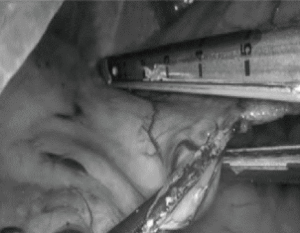
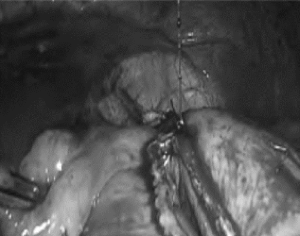
In this surgical technique, the patient is positioned at reversed Trendelenburg and the surgeon is at the between the patient’s legs. Five trocars method is used. An opening, adequate for stapler entrance, is created in the hepatogastric ligament at the level of incisura angularis via vessel sealing device or mono polar hook (Figure 3). Then, the first stapler was introduced through the subxiphoid tracer or right subcostal trocar and placed parallel and 3–4 cm away from the pylorus (Figures 4,5). Before the last stapler, approximately a 2 cm long passage was left at the uppermost stomach (Figure 6). After a gastric transaction, the patient is re-positioned as Trendelenburg and transverse colon and omentum are retracted cranially (Figures 7,8). According to the patient’s BMI between 150 and 250 cm from Treitz ligament, a small bowel segment is brought close to the gastric pouch. After, the patient is re-positioned again, via mono polar hook a hole for the entrance of the stapler is created both on the stomach and the bowel. Finally, gastrojejunostomy anastomosis is created via stapler and stapler entrances sites are closed in a single layer by hand-sewn stich (Figures 9,10). You can find the stages of the BMGB technique step by step below.
The advantages of BMGB method can be summarized below as eight “N”s:
- Never touch and destroy the angle of His;
- Not removing 75–80% of the stomach as in SG;
- No short gastric vessel bleeding during dissection of the fundus during the last stapler as it is performed in the MGB;
- No leak due to an opening between the newly formed pouch and the gastric remnant, the risk of leakage from the pouch is theoretically lower;
- No chance for endoscopic intervention in MGB and Roux-en-Y gastric bypass in cases of remnant gastric bleeding (8,9). Since the remnant stomach can be evaluated endoscopically, remnant gastric bleeding can be controlled more easily during surgery or in the postoperative period. Furthermore, endoscopic surveillance of the remnant stomach, in cases of gastric cancer suspicion, could be performed;
- No narrow pouch-like in the MGB;
- No complications in revisional surgery after adjustable gastric banding because the fundus is fibrotic and thick after gastric banding, the risk of leakage increases in the operations that transect the fundus such as in SG, MGB, and Roux-en-Y gastric bypass (10);
- Not using one extra cartridge for the last few centimeters may provide a significant benefit in terms of cost (11).
After experimental studies, we published a series of five cases on which BMGB was applied. The long-term results of the gastric bridge are not clear in terms of the stenosis or widening of GGF. Although current results are encouraging, further research is needed to provide more information on the long-term effects of this modified technique.
Conclusions
Although MGB is a simple, safe, and effective bariatric procedure, its disadvantage is not to access to remnant stomach. The technique we have developed can solve this problem. We need further studies to prove the reliability and effectiveness of this new technique. A large sample and multi centric randomized control trials are needed to compare the effectiveness and safety between MGB and BMGB.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (M. Mahir Ozmen) for the series “Bariatric and Metabolic Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.12.02). The series “Bariatric and Metabolic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 2011;377:557-67. [Crossref] [PubMed]
- Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11:321-6. [Crossref] [PubMed]
- Deitel M. History of the MGB and OAGB operations. Int J Surg 2019;66:79-83. [Crossref] [PubMed]
- Carbajo MA, Luque-de-León E, Jiménez JM, et al. Laparoscopic One-Anastomosis Gastric Bypass: Technique, Results, and Long-Term Follow-Up in 1200 Patients. Obes Surg 2017;27:1153-67. [Crossref] [PubMed]
- Scozzari G, Trapani R, Toppino M, et al. Esophagogastric cancer after bariatric surgery: Systematic review of the literature. Surg Obes Relat Dis 2013;9:133-42. [Crossref] [PubMed]
- Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, sleeve dilatation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg 2017;27:3092-101. [Crossref] [PubMed]
- Wu CC, Lee WJ, Ser KH, et al. Gastric cancer after mini-gastric bypass surgery: a case report. Asian J Endosc Surg 2013;6:303-6. [Crossref] [PubMed]
- Rabl C, Peeva S, Prado K, et al. Early and late abdominal bleeding after Roux-en-Y gastric bypass: sources and tailored therapeutic strategies. Obes Surg 2011;21:413-20. [Crossref] [PubMed]
- Issa H, Al-Saif O, Al-Momen S, et al. Bleeding duodenal ulcer after Roux-en-Y gastric bypass surgery: the value of laparoscopic gastroduodenoscopy. Ann Saudi Med 2010;30:67-9. [Crossref] [PubMed]
- Tran TT, Pauli E, Lyn-Sue JR, et al. Revisional weight loss surgery after failed laparoscopic gastric banding: an institutional experience. Surg Endosc 2013;27:4087-93. [Crossref] [PubMed]
- Aziz S, Deniz A, Umut B, et al. Bridged Mini Gastric Bypass: A Novel Metabolic and Bariatric Operation. Barıatrıc Surgıcal Practıce and Patıent Care 2019;14:62-7. [Crossref]
Cite this article as: Sumer A, Aktokmakyan TV, Peksen C. Mini gastric by-pass and bridged mini gastric by-pass: what is new? Ann Laparosc Endosc Surg 2020;5:8.