Umbilical hernia: when and how
Introduction
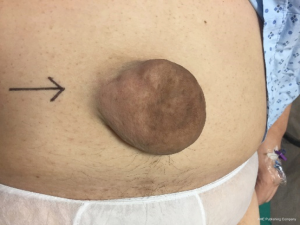
The term hernia originates from the ancient Greek word for “bulge” and similarly in Latin, hernia represents a tear or rupture. An umbilical hernia is defined as a protrusion or bulge of an organ or part of it, usually omentum, small bowel or less commonly colon (1) from an umbilical or paraumbilical opening. A true umbilical hernia is congenital and results from a failure of closure of the umbilical ring in the early years of life (2). In adults, umbilical hernias are usually acquired, defined as a defect from 3 cm above to 3 cm below the umbilicus and they are usually classified as indirect hernia (3,4) (Figure 1).
The incidence of umbilical hernias in adults ranges from 10% to 25% in the literature and is increased in females (2). Some predisposing factors for the development of umbilical hernia include pregnancy, obesity, ascites and large abdominal tumor leading to increased abdominal pressure (4). Asolati et al. also described that in patients with type II diabetes, hyperlipidemia, and in those positive for human immunodeficiency virus, these groups of patients may have a higher risk of recurrence after elective umbilical hernia repair (5).
In infants, genetic conditions such as low birth weight (<1,500 g), African or African-American ancestry, Beckwith-Wiedemann syndrome and trisomy 21, 18, 13 are also described as risk factors (6).
In this review, the literature on umbilical and para-umbilical hernia in adults was reviewed from relevant databases. The objective is to give a comprehensive, up-to-date overview on umbilical hernia treatment, including special cases such as cirrhotic patients, pregnancy and emergency repair. Our challenge is to critically-appraise and summarize the abundant literature on umbilical hernia repairs. Although there is a good amount of recently-published data, the majority of studies are limited by small sample size and quality, high bias associated with hernia defect size, mismatched groups and heterogeneity in types of hernia: epigastric, Spigelian, recurrent, emergency situations and high-risk patients.
Umbilical hernia repair: when?
Approximately 175,000 umbilical hernias are surgically repaired annually in US (4). According to the National Health System in UK, the average waiting time for hernia surgery increased to almost 104 days, from year 2010 to 2015.
The neck of acquired umbilical hernia in adult is usually narrow hence the higher likelihood of strangulation, incarceration, obstruction, skin ulceration and rupture (Figure 2). Symptoms include pain (44%), pressure (20%) and nausea or vomiting (9%) (2,7). Thus, in this scenario surgery is recommended, taking into consideration the risk of complications as high as 30% without surgery.
In a cohort study encompassing 3,000 hospitals and 279 employers in the United States, two groups were evaluated for the cost of watchful waiting as a strategy in patients with umbilical hernia. Surgical group (open and laparoscopic approach) showed higher costs at 90 and 365 days than the non-surgical group. However, non-surgical group had a significantly higher utilization of healthcare and estimated days off work than the surgical group, concluding that early intervention decreases costs and resource utilization (8).
On the other hand, Kokotovic et al., in a retrospective analysis of 789 patients with both umbilical and epigastric hernias found that the probability for patients who underwent watchful waiting to receive later surgery in 5 years was 16% and 4% for emergency hernia repair (9).
Therefore, they consider watchful waiting to be a safe strategy. Limitations of that study include a retrospective analysis, inclusion of all ventral hernias, and no information on hernia size.
In a randomized trial conducted by Abdel-Baki et al., 42 patients underwent emergency hernia repair either with or without mesh placement. The complication rate was approximately 26% for both groups, much higher than the one cited in the literature for elective procedures (10).
Umbilical mesh repair: how? Mesh or primary suture repair
In recent years, utilization of mesh in the repair of umbilical hernias bigger than 3cm has gained popularity. This is due to the fact that the rate of recurrence is lower after mesh repair when compared to open suture repair (3). In contrast, other studies have shown an increased rate of wound infection and complications with mesh repair (11-13).
There is much debate involving umbilical hernias <2–3 cm and even more for defects less than 1 cm. Berger et al. in a retrospective study with 392 patients, compared 126 patients with open mesh repair and 266 patients with open primary suture repairs, both groups with 30 months follow-up. There was no difference in recurrent rate in both groups and mesh repair was associated with increased rates of seroma and wound infection. However, in case-matched outcomes, recurrence was 10% on suture repair group and 5.6% on mesh repair. Surgical site infection (SSI) was 10% on the suture group vs. 16.7% on mesh group. These results were not statistically significant (12).
Another retrospective study evaluated 146 patients with open primary suture repair, 52 patients underwent open mesh repair and 18 laparoscopic mesh repair with a median follow-up of 56 months. Suture repair was preferred when the defect was between 2–4 cm (70.5%), open mesh and laparoscopic technique were used for defects bigger than 4 cm and for patients with body mass index (BMI) higher than 30 kg/m2. Overall recurrence rate was 13.1%, higher for open mesh group and BMI >30 with no statistical difference between the groups (14).
In a meta-analysis comparing 637 mesh repairs and 1,145 patients with primary suture repair recurrence rate for mesh repair was 2.7% as opposed to 8.2% in the suture repair group, showing a reduction in recurrence for mesh repairs. Additionally, mesh usage increased the risk of seroma formation (7.7% vs. 3.8%) and SSI (7.3% vs. 6.6%) (11). The limitation of this study is the inclusion of different types and position of meshes, omitted hernia size, and several different techniques for suture repair.
In a Danish cohort study with 4,786 patients that underwent either open mesh or suture repair for umbilical and epigastric hernias ≤2 cm, recurrence rate was 2.2% in the mesh group and 5.6% in the suture group with a follow-up period of 21 months (15). In a second publication the same group compared 928 patients in the mesh group and 385 in the suture group. The authors found that a higher recurrence rate in the second group, after 55 months follow-up. Cumulative recurrence for suture repair was 21% and 10% for mesh repair, far higher than seen in the literature. In addition, there was no difference in terms of type or placement of meshes in terms of recurrence. On the other hand, in the 0–1 cm subgroup mesh, there was 12% recurrence rate whereas the suture-only group has 21% recurrence rate. In the 1–2 cm mesh subgroup, the recurrence rate was 8% while in the suture-only subgroup, it was 17%, which was a statistically significant difference (7).
According to Shankar et al., after analyzing data from 332 patients from a public database of military veteran patients who were followed-up for 8.5 years, the recurrence rate for open mesh repair was 2.4% and for open suture repair was 9.8%. Interestingly, 50% of recurrences happened within the first year, 75% in the first 5 years and 25% five years after repair (16). This study has several limitations including lack of information on hernia size defect in a war veterans’ group of patients with several associated comorbidities and mix of elective and emergency surgery. Nevertheless, it implies once again that hernia recurrences should be evaluated on a much longer term than the current literature has provided.
Between 2001 and 2017 there were only four randomized controlled trials (RCT) on umbilical hernia repair reported in the literature (10,17-19). Arroyo et al. randomized 200 patients into two groups: primary interrupted suture repair and polypropylene mesh or mesh plug repair. Recurrence rate was 11% in the suture repair group vs. 1% after mesh repair. The mean follow-up was 64 months and there were no differences in complications such as seroma, hematoma or SSI between the groups (17). However, the mesh groups studied were heterogeneous, there is no mention on the time of recurrence and it lacks precise defect sizes.
Polat et al. studied 50 patients randomized in three groups. Thirty-two patients underwent umbilical mesh repair and 18 patients Mayo repair, with a mean follow-up of 22 months. There was no recurrence on the mesh group and 11% recurrence on Mayo group (18). Small randomized samples, usage and placement techniques of different types of mesh and hernia defects smaller than 4 cm could be a limitation for this RCT.
A recent RCT published in The Lancet shed light upon small umbilical hernias with diameter between 1–4 cm. This study randomized 300 patients from 12 different hospitals in two groups: mesh and suture repair. This RCT was a two-arm study comprising standardized techniques for both mesh and suture repair, with only one type of mesh allowed and they studied only umbilical hernias. Post-operative analgesia was standardized and patients were followed up for a maximum of 30 months. Recurrence rate was lower in the mesh group (4% vs. 12%) than in the suture group. In the 1–2 cm subgroup, there were 2% recurrence with mesh repair versus 8% recurrence with suture repair. The results were similar in the 2–4 cm subgroup, with a higher recurrence rate in the suture group (9% vs. 22%). The onset of recurrence was earlier for the suture group when compared to mesh (3.6 vs. 12.6 months). Neither BMI nor hernia diameter affected hernia recurrences in both groups. Complications such as seroma, hematoma and SSI were 1–3% with no significant difference seen in both groups (3).
Post-operative pain was evaluated at two different time-points in time: 2 weeks and 2 years after surgery. Once more there was no difference in both groups, 93% of patients in the suture group and 95% in mesh group were pain-free at 2-year follow-up (3).
Chronic pain after mesh repair is a main factor in considering the type of repair in umbilical hernia. More than one publication proposed the theory that chronic pain is associated with hernia recurrences rather than the mesh itself (7,14,18,20).
Christoffersen et al. evaluated 1,313 patients and they found an incidence of chronic pain in 6% of mesh repair and 5% when suture repair was chosen and they concluded that the only independent risk associated to chronic pain was recurrence (7).
At the same time, Xie et al. studied 123 patients whom underwent lightweight mesh plug technique for umbilical hernias <3 cm and they found 2.4% of their patients suffered from chronic pain after 33 months of follow-up (21).
Laparoscopic or open repair
Although laparoscopic procedures are accepted worldwide and these techniques are considered as indispensable in the armamentarium of many general surgeons, its utilization in umbilical hernias remains low. Laparoscopic umbilical repair is the preferred approach in only a quarter of umbilical hernia surgery (22). When we reviewed all RCTs published comparing open versus laparoscopic repair, the findings were quite similar.
We also looked at an Indian study comparing 42 patients in which 21 underwent laparoscopic mesh repair and 21 open mesh repair. The authors found higher SSI and recurrence rates in the open group (9.5% and 4.8%). Seroma occurred in about 4.8% of patients in both groups (23). However, this study did not publish the hernia defect sizes, has a small sample size and the patients were only on 3 months follow-up.
An Egyptian RCT with 20 patients on laparoscopic mesh repair and 20 open suture repair followed up for 36 months found 5% conversion rate to open repair. There were also 10% occurrence rate of seroma in the laparoscopic group, 15% of patients developed wound infection and seroma on open group. Recurrence rate was not mentioned (24). There was similar limitation to prior studies whereby there was no mention of hernia defect sizes and the sample size was small.
Malik in a study with 337 patients comprising 166 laparoscopic mesh repairs and 171 open mesh repairs. Patients were followed up for 24 months and the defect sizes ranged from 2.5 to 4.5 cm. Conversions to open were 6.6% and seroma and hematoma were higher on open group, as well as recurrence (9.3%) (20).
Cassie et al., in a retrospective cohort study with 13,109 patients that underwent open hernia repair and 1,543 patients on a laparoscopic hernia repair group, concluded that laparoscopic repair presented a decrease wound infection rate at the expense of increased operative time, LOS, and respiratory and cardiac complications (25).
In a meta-analysis from UK, six studies with 1,094 patients comparing open mesh and laparoscopic repair showed higher risk of wound infection in the open group but no statistical difference in wound dehiscence, seroma, hematoma or recurrence between the two groups.
When comparing open suture repair and laparoscopic mesh repair, 5 studies were included with a total of 689 patients. There was no difference in wound dehiscence rate, hematoma or seroma between the groups. Wound infection and recurrence rates were, however higher on open group (26).
Laparoscopic repair was associated with longer operative time which can be explained by the multiple extra steps needed for this technique when compared to open repair, less pain 24 h after surgery, and in some studies less wound infection rates (26,27). There is paucity of data on port-sites hernia, and this potential complication should be taken into consideration, especially when considering small umbilical hernias, while being mindful of increased cost in laparoscopic repair.
Special situations
Pregnancy and umbilical hernia
According to Oma et al., the incidence of umbilical hernia among Danish women of childbearing age (15–45 years) is 15.4% (28). On the other hand, the risk of umbilical hernia during pregnancy is only 0.08% (4).
There is no consensus on the right timing of elective repair for umbilical hernia in this population as there is scant literature on this topic. The majority of publications stratified cases according to the following scenarios:
- Umbilical hernia in women planning for a pregnancy;
- Umbilical hernia diagnosed during pregnancy;
- Simultaneous repair of umbilical hernia and planned C-section;
- Hernia repair after childbirth.
There are many considerations pertaining to achieving the most optimal strategy in the repair of an umbilical hernia in a pregnant woman or in a woman intending to become pregnant. Even in emergency situations such as incarceration or strangulation, there is concern that the mesh, as a foreign body, might cause infertility and abdominal pain especially in the last stages of pregnancy by compromising the flexibility of the abdominal wall (4,28,29).
By the 20th to 22nd week of pregnancy the uterus reaches the level of umbilicus, thereafter the risk of incarceration decreases. However if an emergency situation occurs, it appears to be safe to perform a surgical intervention on the first 6 months of pregnancy (4). Haskins et al. reported 126 pregnant women operated for umbilical hernia, 58% in emergency situations and 95% underwent open repair. No fetal loss was reported (30).
It is well-recognized that suture repair carries a higher risk of recurrence than mesh repair. Lappen et al. also describes that pregnancy itself carries a higher risk for recurrence caused by the increased in intra-abdominal pressure. In this study with 11,020 women of childbearing age, 7.6% were pregnant following umbilical hernia repair and this was independently associated with a 73% increase in risk of reoperation for recurrence (31).
A Danish study showed a 1.6-fold increased risk of hernia recurrence with subsequent pregnancy in a group of 267 patients (32).
Oma et al. in a Danish database found 224 patients that underwent pre-pregnancy umbilical hernia repair. Primary suture repair was done in 78% of the cases. No difference in mesh and suture repair was found after 3.8 years of follow up (33).
A Danish systematic review reported 74 umbilical hernias repair concomitant to elective caesarean section (C-section) compared to 645 elective C-section. Four case-control studies comparing C-section alone with concomitant hernia repair found no major complications in the short-term morbidity. Three studies reported low recurrence rate, however one case-control study shows a recurrence rate of 28%. All studies had a longer operation time and higher usage of analgesia for the concomitant repair group. In conclusion, these authors do not advocate concomitant umbilical hernia repair and elective C-section since only few patients (29%) required surgery if an umbilical hernia is left untreated during pregnancy (28).
In contrast to these findings a more recent prospective study with 45 patients divided in three groups: 15 patients undergoing umbilical hernia repair by pre-peritoneal mesh insertion during C-section; 15 by an incision other than the Pfannenstiel, and 15 with a later approach after C-section healing. The first group had shorter hospital stay, low incidence of wound infection, seroma, skin flap ischemia and mesh rejection, thus the authors concluded that this should be the best approach for pregnant women with umbilical hernia (34).
Therefore, suture repair in this population should be carefully considered and the patient must be advised on the possibility of a second repair with mesh after her last pregnancy.
Cirrhotic patient and umbilical hernia
Umbilical hernia repair in a cirrhotic patient with ascites is a very challenging scenario. In the past, most surgeons would avoid repairing any umbilical hernia in patients with more than Child-Pugh A liver cirrhosis unless in emergency situations (35). The incidence of umbilical hernias in cirrhotic patients is approximately 20%, higher than in the general population and occurs more on males than in females. These hernias tend to enlarge rapidly and have a marked predisposition for complications (36,37).
Saleh et al. in a total of 688 patients with ascites that underwent umbilical hernia repair found that 44% of cases were classified as emergency cases with 7% mortality rate (38).
Eker in a study with 30 patients that underwent elective umbilical hernia repair described that the majority of patients were of Child-Pugh B classification (63%). Thirty-three percent of them had mesh repairs and the mortality rate was 7% but the cause of death was most likely not related to the surgery itself (37).
Amar in a randomized study divided 80 patients with liver cirrhosis into two groups: group A underwent suture repair and group B mesh repair for the umbilical hernia. The recurrence rate was consistent with the literature: 14.2% for suture repair and 2.7% for the mesh repair group. Thirty-seven patients were Child-Pugh B and despite this, all patients described minimal wound complications and no mortality (39).
All of these studies suggested that Child-Pugh C classification and refractory ascites were risk factors for mortality and recurrence. Ideally, for patients who were within 3–6 months from a transplant, the umbilical hernia should be repaired during the transplant. Surgery for this group of patients should not be delayed as major risk of complications are at stake. On a final note, most authors suggested that we should be wary in offering any forms of surgical repair in patients with refractory ascites.
Emergency umbilical hernia repair: is laparoscopic approach accepted? Mesh or no mesh?
The most conventional approach to emergency umbilical hernia is the open hernia repair, especially if the patients are premorbidly unwell, be it with or without bowel resections. However, the laparoscopic approach is acceptable and may even be preferred when the patient is obese or when the presentation is early especially if there are no bowel resections required.
In the emergency setting, there are many advantages to the laparoscopic approach including better visualization of occult hernia within the abdominal wall, smaller incision which may lead to lesser analgesic requirements postoperatively, lower incidence of postoperative ileus and lower wound complications rate.
Nevertheless, there are some contraindications to the use of laparoscopy in the emergency setting including sick patients who are unable to tolerate pneumoperitoneum, dilated small bowels especially those more than 5 cm and dense adhesions or other factors prohibiting insertion of laparoscopic trocars.
In a few large case series of incarcerated umbilical hernia published the authors have demonstrated the safe and efficacious ways of performing laparoscopic umbilical hernia repair in the emergency setting (10,40,41).
Shah et al. in New Delhi, India studied retrospectively the 112 cases of incarcerated umbilical hernia performed laparoscopically. They found that 90% of the cases were completed laparoscopically with successful mesh placement, with the majority of the patients staying in the hospital for 2–3 days postoperatively. Two patients required conversion to open due to long-segment bowel injuries and peritoneal contamination. Complications were reported at 20.5% (15 patients developed seroma and other wound complications, 1 had mesh infection with sinus and 3 patients had hernia recurrences) at mean follow-up of 2 years (40).
As for Landau et al. in Tel Aviv, Israel, they reported 25 patients out of which 8 had previous umbilical hernioplasty before. There was one case of enterotomy requiring conversion to open. They reported 3 patients with seroma and 1 patient with trocar site herniation (41).
Another important consideration is the use of mesh in the emergency setting. Careful adhesiolysis and avoidance of enterotomy enables safe use of conventional meshes such as non-absorbable mesh in the pre-peritoneal layer or the composite mesh in the intra-peritoneal manner. This will reduce the chances of hernia recurrence as compared to sutures repair alone. Both authors described the use of mesh in the emergency settings, however there is the risk of mesh infection if there is concomitant bowel repair or anastomosis. Thus, most surgeons would prefer suture repair in cases of bowel anastomosis or bowel contamination during the emergency repair. Summary of the literature published showed that there is a paucity of high-quality evidence on the best practice in emergency umbilical hernia repair, with a handful of retrospective case series forming the majority of published data on this condition.
Conclusions
Surgeons often face multiple dilemma in the management of adult umbilical hernia. Despite being one of the most common surgical condition, there are still many controversies swirling around the best approach in management of umbilical hernia. Most surgeons appear to be comfortable with primary suture repair, especially for small hernias. In view of recent publications including good RCT, we propose that mesh repair is the now considered to be the gold-standard repair for all umbilical hernias with defect size measuring 1 to 4 cm.
Laparoscopic repair carries a higher cost, longer surgical time, involves a steeper learning curve and may increase cardio-pulmonary complications. However, it is also associated with less pain on the post-operative period and appears to demonstrate lower incidence of short-term complications around the world. For these reasons it should be presented as a first option if a surgeon is able to offer laparoscopic mesh repair.
Watchful waiting may be considered as an alternative for small hernias in high risk patients such as pregnant women and cirrhotic patients.
There is still limited data in hernia less than 1 cm in size, and surgeons should approach each case individually, considering their own expertise and the patient’s needs.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Ventral Hernia”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.03.07). The series “Ventral Hernia” was commissioned by the editorial office without any funding or sponsorship. DL served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Panesar K. Managing Abdominal Hernias. US Pharmacist 2017;42:HS10-HS16.
- Ponten JE, Thomassen I, Nienhuijs SW. A Collective Review on Mesh-Based Repair of Umbilical and Epigastric Hernias. Indian J Surg 2014;76:371-7. [Crossref] [PubMed]
- Kaufmann R, Halm JA, Eker HH, et al. Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. Lancet 2018;391:860-9. [Crossref] [PubMed]
- Kulacoglu H. Umbilical Hernia Repair and Pregnancy: Before, during, after… Front Surg 2018. Available online: https://www.frontiersin.org/article/10.3389/fsurg.2018.00001
- Asolati M, Huerta S, Sarosi G, et al. Predictors of recurrence in Veteran patients with umbilical hernia: single center experience. Am J Surg 2006;192:627-30. [Crossref] [PubMed]
- Zens T, Nichol PF, Cartmill R, et al. Management of asymptomatic pediatric umbilical hernias: a systematic review. J Pediatr Surg 2017;52:1723-31. [Crossref] [PubMed]
- Christoffersen MW, Helgstrand F, Rosenberg J, et al. Long-term recurrence and chronic pain after repair for small umbilical or epigastric hernias: a regional cohort study. Am J Surg 2015;209:725-32. [Crossref] [PubMed]
- Strosberg DS, Pittman M, Mikami D. Umbilical hernias: the cost of waiting. Surg Endosc 2017;31:901-6. [Crossref] [PubMed]
- Kokotovic D, Sjølander H, Gögenur I, et al. Watchful waiting as a treatment strategy for patients with a ventral hernia appears to be safe. Hernia 2016;20:281-7. [Crossref] [PubMed]
- Abdel-Baki NA, Bessa SS, Abdel-Razek AH. Comparison of prosthetic mesh repair and tissue repair in the emergency management of incarcerated para-umbilical hernia: a prospective randomized study. Hernia 2007;11:163-7. [Crossref] [PubMed]
- Nguyen MT, Berger RL, Hicks SC, et al. Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy: A systematic review and meta-analysis. JAMA Surg 2014;149:415-21. [Crossref] [PubMed]
- Berger RL, Li LT, Hicks SC, et al. Suture versus preperitoneal polypropylene mesh for elective umbilical hernia repairs. J Surg Res 2014;192:426-31. [Crossref] [PubMed]
- Winsnes A, Haapamäki MM, Gunnarsson U, et al. Surgical outcome of mesh and suture repair in primary umbilical hernia: postoperative complications and recurrence. Hernia 2016;20:509-16. [Crossref] [PubMed]
- Venclauskas L, Jokubauskas M, Zilinskas J, et al. Long-term follow-up results of umbilical hernia repair. Wideochir Inne Tech Maloinwazyjne 2017;12:350-6. [Crossref] [PubMed]
- Christoffersen MW, Helgstrand F, Rosenberg J, et al. Lower Reoperation Rate for Recurrence after Mesh versus Sutured Elective Repair in Small Umbilical and Epigastric Hernias. A Nationwide Register Study. World J Surg 2013;37:2548-52. [Crossref] [PubMed]
- Shankar DA, Itani KMF, O’Brien WJ, et al. Factors Associated with Long-term Outcomes of Umbilical Hernia Repair. JAMA Surg 2017;152:461-6. [Crossref] [PubMed]
- Arroyo A, García P, Pérez F, et al. Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg 2001;88:1321-3. [Crossref] [PubMed]
- Polat C, Dervisoglu A, Senyurek G, et al. Umbilical hernia repair with the prolene hernia system. Am J Surg 2005;190:61-4. [Crossref] [PubMed]
- Eriksen JR, Bisgaard T, Assaadzadeh S, et al. Randomized clinical trial of fibrin sealant versus titanium tacks for mesh fixation in laparoscopic umbilical hernia repair. Br J Surg 2011;98:1537-45. [Crossref] [PubMed]
- Malik AM. Laparoscopic versus open repair of para-umbilical hernia. Is it a good alternative? J Pak Med Assoc 2015;65:865-8. [PubMed]
- Xie Y, Song Y, Jian F, et al. Retrospective analysis of smaller than 3-cm umbilical hernia repair with the lightweight macroporous mesh. Medicine (Baltimore) 2018;97:e12245 [Crossref] [PubMed]
- Funk LM, Perry KA, Narula VK, et al. Current national practice patterns for inpatient management of ventral abdominal wall hernia in the United States. Surg Endosc 2013;27:4104-12. [Crossref] [PubMed]
- Purushotham B, Madhu S. Comparative study between laparoscopic and open repair of umbilical and para umbilical hernia. International Surgery Journal 2015;2:204-13. [Crossref]
- Othman IH, Metwally YH, Bakr IS, et al. Comparative study between laparoscopic and open repair of paraumbilical hernia. J Egypt Soc Parasitol 2012;42:175-82. [Crossref] [PubMed]
- Cassie S, Okrainec A, Saleh F, et al. Laparoscopic versus open elective repair of primary umbilical hernias: short-term outcomes from the American College of Surgeons National Surgery Quality Improvement Program. Surg Endosc 2014;28:741-6. [Crossref] [PubMed]
- Hajibandeh S, Hajibandeh S, Sreh A, et al. Laparoscopic versus open umbilical or paraumbilical hernia repair: a systematic review and meta-analysis. Hernia 2017;21:905-16. [Crossref] [PubMed]
- Lomanto D, Iyer SG, Shabbir A, et al. Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc 2006;20:1030-5. [Crossref] [PubMed]
- Oma E, Henriksen NA, Jensen KK. The American Journal of Surgery Ventral hernia and pregnancy: A systematic review. Am J Surg 2019;217:163-8. [Crossref] [PubMed]
- Jensen KK, Henriksen NA, Jorgensen LN. Abdominal wall hernia and pregnancy: a systematic review. Hernia 2015;19:689-96. [Crossref] [PubMed]
- Haskins IN, Rosen MJ, Prabhu AS, et al. Umbilical hernia repair in pregnant patients: review of the American College of Surgeons National Surgical Quality Improvement Program. Hernia 2017;21:767-70. [Crossref] [PubMed]
- Lappen JR, Sheyn D, Hackney DN. Does pregnancy increase the risk of abdominal hernia recurrence after pre - pregnancy surgical repair? Am J Obstet Gynecol 2016;215:390.e1-390.e5. [Crossref]
- Oma E, Jensen KK, Jorgensen LN. Increased risk of ventral hernia recurrence after pregnancy: A nationwide register-based study. Am J Surg 2017;214:474-8. [Crossref] [PubMed]
- Oma E, Jensen KK, Jorgensen LN. Recurrent umbilical or epigastric hernia during and after pregnancy: A nationwide cohort study. Surgery 2016;159:1677-83. [Crossref] [PubMed]
- Eltokhy EA, Harera IS, Gertallah LM, et al. Simultaneous Repair of Para-Umbilical Hernia during Cesarean Section (CS): A Novel Approach. Surgical Science 2018;9:233-42. [Crossref]
- McKay A, Dixon E, Bathe O, et al. Umbilical hernia repair in the presence of cirrhosis and ascites: results of a survey and review of the literature. Hernia 2009;13:461-8. [Crossref] [PubMed]
- Andraus W, Pinheiro RS, Lai Q, et al. Abdominal wall hernia in cirrhotic patients: emergency surgery results in higher morbidity and mortality. BMC Surg 2015;15:65. [Crossref] [PubMed]
- Eker HH, van Ramshorst GH, de Goede B, et al. A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery 2011;150:542-6. [Crossref] [PubMed]
- Saleh F, Okrainec A, Cleary SP, et al. Management of umbilical hernias in patients with ascites: development of a nomogram to predict mortality. Am J Surg 2015;209:302-7. [Crossref] [PubMed]
- Ammar SA. Management of complicated umbilical hernias in cirrhotic patients using permanent mesh: randomized clinical trial. Hernia 2010;14:35-8. [Crossref] [PubMed]
- Shah RH, Sharma A, Khullar R, et al. Laparoscopic repair of incarcerated ventral abdominal wall hernias. Hernia 2008;12:457. [Crossref] [PubMed]
- Landau O, Kyzer S. Emergent laparoscopic repair of incarcerated incisional and ventral hernia. Surg Endosc 2004;18:1374-6. [Crossref] [PubMed]
Cite this article as: Maia RA, Salgaonkar HP, Lomanto D, Loo L. Umbilical hernia: when and how. Ann Laparosc Endosc Surg 2019;4:37.