
Duhamel operation for Hirschsprung’s disease; laparoscopic modified Duhamel procedure with Z-shaped anastomosis
Introduction
Compared with other major surgical techniques for Hirschsprung disease (HD), such as the Soave and Swenson procedure, the original Duhamel procedure has the benefit of less pelvic dissection and less anastomotic stricture formation, but the most common postoperative complication is fecalith formation secondary to a rectal blind pouch or remnant colorectal septum. The Z-shaped colorectal side-to-side anastomosis was introduced in 1967 (1,2) to improve the original Duhamel procedure by eliminating the rectal blind pouch and completely dividing the colorectal septum.
We compared outcome of surgery for total colon aganglionosis (TCA) and classical type recto-sigmoid HD (RS-HD) at our institute and elsewhere focusing on the laparoscopic Duhamel-Z procedure (Lap-DZ).
Surgical technique (TCA): our Lap-DZ
For Lap-DZ, four 5 mm ports were used for dissection of the entire colon beginning from the peritoneal reflection at the sigmoid colon progressing proximally to the ileostomy site following the bowel wall closely using conventional laparoscopic technique. After the ileostomy was taken down under laparoscopic control (3), pull-through ileum was prepared by dissecting the mesentery. At this point, we used to make a small Pfannenstiel incision to create a retrorectal route for the pull-through ganglionic ileum and make a Duhamel-Z anastomosis, but currently, we use the ileostomy site to insert a free access port (Top Corporation, Tokyo, Japan) to continue the rest of the procedure laparoscopically without the Pfannenstiel incision.
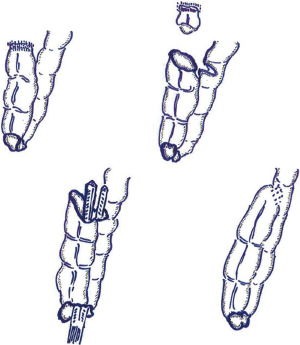
The rectum was resected 2 cm above the peritoneal reflection. (I) The rectum was resected 2 cm above the peritoneal reflection, and a space was created behind the aganglionic rectum; (II) the posterior wall of the rectum was incised full-thickness at a level approximating the anorectal line to access the space created in 1; (III) ganglionic ileum was passed through the space created in 1, and pulled-through the incision made in 2; (IV) the pulled-through ganglionic ileum was anastomosed full-thickness to the incision made in the posterior wall of the rectum; (V) the anterior wall of the ganglionic ileum was incised at a level equivalent to the length of the rectal stump; (VI) the anal edge of the incision in the ganglionic ileum and the posterior wall of the rectal stump were tightly anastomosed; (VII) a surgical stapler was inserted through the anal end of the anastomosis performed in 4 and used to divide the septum that formed during 5 and 6 from the posterior wall of the aganglionic rectum and the anterior wall of the ganglionic ileum; usually requiring 2 cartridges of 60 mm staples to completely resect the septum; (VIII) the ventral side of the ganglionic rectal stump and the rostral edge of the incision in the ganglionic ileum are sutured and closed, in two layers to complete a Z-shaped colorectal side-to-side anastomosis without a blind pouch (Figure 1).
Our postoperative follow-up (TCA)
Postoperative bowel function was managed according to our standard protocol with daily administration of an antiflatulent (and/or antidiarrheal) medication and regular enemas supervised strictly by experienced nursing stuff until discharge from hospital. The frequency of daily enemas was reduced postoperatively. Continence evaluation was assessed with a standardized questionnaire covering growth, stool frequency, stool consistency, fecal soiling and incontinence, and severity of enterocolitis which we defined as the simultaneous presence of diarrhea, fever and bowel distention. A scoring system [0–2] was used for the assessment of responses to each criterion to give a maximum score of 10 (Table 1).
Table 1
| Score | Stool frequency (motions/day) | Stool consistency | Fecal staining | Enterocolitis (episodes/year) | Growth |
|---|---|---|---|---|---|
| 0 | >6 | Watery | (+) | >2 | Weight <−2 SD |
| 1 | 3–5 | Soft | (+/−) | 1 | −2 SD > weight >−1 SD |
| 2 | 0–2 | Normal | (−) | 0 | Weight >−1 SD |
TCA, total colon aganglionosis; SD, standard deviation.
Outcome (TCA): our Lap-DZ
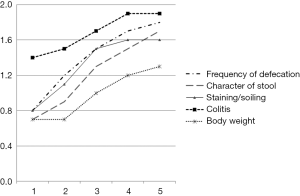
We evaluated 11 TCA cases we treated with Lap-DZ, followed-up more than 5 years with annual bowel function assessment. There were 6 males and 5 females; mean age at Lap-DZ was 10.2 months (range, 7–16 months); mean weight at Lap-DZ was 8.4 kg (range, 6.5–9.7 kg); mean length of the segment of aganglionic ileum resected was 19.5 cm; mean operative time was 6.2 hours; mean annual continence evaluation scores improved gradually during follow-up from 4.4 after one year to 5.4, 7.0, 7.9, and 8.3, respectively (Figure 2).
There were no intraoperative complications. One subject died from congenital heart disease 2 years after Lap-DZ. Another subject with chronic lower gastrointestinal tract bleeding causing iron deficiency anemia required blood transfusion 4 months postoperatively. There were no anastomotic leaks, strictures, or intestinal obstructions recorded, and no patient required redo surgery. No subject was constipated during the follow-up period.
Outcome (RS-HD): Lap-DZ performed elsewhere
Lap-DZ performed elsewhere (4) for 25 cases of RS-HD in children using a similar approach to ours but with 3 trocars and no stoma access. They reported that while frequency of defecation gradually decreased postoperatively, 21/25 patients (84%) experienced episodes of constipation during the early follow-up period and were prescribed laxatives or enemas, but the need for medication decreased as the children grew older. Of 14 patients older than 4 years at the time of assessment, all achieved normal defecation without fecal incontinence, excluding one patient with trisomy 21. Of the cases achieving normal defecation, 5 required occasional laxatives for mild constipation. Similar results have been reported from other centers (5).
Outcome (RS-HD): our laparoscopic soave procedure
We assessed the mid-term outcomes of 33 patients we treated using our laparoscopic Soave transanal pull-through for classical rectosigmoid type HD between 2007 and 2011 followed-up for at least 4 years postoperatively. Because we did not establish common definitions for constipation, incontinence etc., there may be discrepancies between centers but assuming that most centers use terminology broadly in the general sense, then we experienced 2 cases of postoperative colitis (6.1%); both were treated successfully as outpatients by colonic decompression and intravenous antibiotics. None of our cases have reported constipation. Mean annual postoperative fecal continence scores (factors including frequency of motions, severity of staining/soiling, severity of perineal erosions, anal appearance, requirement of medications, sensation of rectal fullness, ability to distinguish flatus from stools, etc., 0–14, as total score) have improved gradually, from 9.7 at 4 years, 10.1 at 5 years, 10.6 at 6 years, and 11.3 at 7 years, postoperatively (6).
Discussion
Although, several laparoscopic Duhamel-like procedures have been reported, when these procedures were performed, there was usually a short blind pouch or the upper colorectal septum was left intact (7-9). Enterocolitis is a well-known complication of TCA, and previous studies have reported incidence rates ranging from 30% to 75% (10-13). In our series of Lap-DZ for TCA, mid-term postoperative annual bowel function evaluation scores, which include the incidence of enterocolitis, improved gradually for each criterion over time. The favorable postoperative course followed by our cases with acceptable incidence of enterocolitis could be attributed to the blind pouch being eliminated with Lap-DZ. Our cases also appear to have relatively less postoperative fecal incontinence compared with other reports in the literature (13-15), although our postoperative bowel function evaluation scores for TCA are still not fully acceptable, the overall trend is to improvement, possibly because of a sufficient and appropriate volume reservoir created by the aganglionic rectum and ganglionic ileum, as well as the lower incidence of enterocolitis, mentioned above.
Peña et al. (16) reported that fecal incontinence after surgical management of HD should not occur in theory because patients have anatomically intact continence mechanisms, such as intact urge sensation, voluntary sphincter control, and appropriate colonic motility, but, sensation and sphincter control may be damaged during primary surgical repair, compromising colonic motility. We agree with this theory, especially in RS-HD, so our postoperative fecal continence evaluation for RS-HD cases is more thorough than our evaluation for TCA cases (6). Some centers in Japan (17) use a Duhamel Z-shaped anastomosis preferentially with excellent clinical results, and recently, laparoscopic Duhamel Z-shaped anastomosis was reported for RS-HD (4). They recommend Duhamel Z-shaped anastomosis for RS-HD; however, we currently recommend Duhamel Z-shaped anastomosis only for TCA, and Soave procedure for RS-HD (6). Centers preferring Soave-like procedures, tend to regard constipation as a possible cause of enterocolitis, and if severe, or recurrent, enterocolitis can precipitate a critical irreversible situation, while incontinence is generally expected to improve gradually or resolve spontaneously over time. On the contrary, centers preferring Duhamel-like procedures do not readily acknowledge any relevant relationship between constipation and enterocolitis, so treat constipation with laxatives, and regard incontinence and soiling regarded as being problematic and difficult to control. There is no consensus about the optimal procedure/approach for RS-HD, with pros and cons constantly being discussed for both Soave and Duhamel procedures.
Based on our limited assessment of outcome, we currently recommend Lap-DZ only for TCA. Longer term follow-up and larger series will provide more clinical data to allow a recommendation to be made for treating HD in the future. Unfortunately, at this stage, we have no additional evidence to make a recommendation for treating HD.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kenneth K. Y. Wong and Patrick Ho Yu Chung) for the series “Paediatric Minimally Invasive Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.11.04). The series “Paediatric Minimally Invasive Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ikeda K. New techniques in the surgical treatment of Hirschsprung’s disease. Surgery 1967;61:503-8. [PubMed]
- Livaditis A. Hirschsprung’s disease: long-term results of the original Duhamel operation. J Pediatr Surg 1981;16:484-6. [Crossref] [PubMed]
- Miyano G, Yanai T, Okazaki T, et al. Laparoscopy-assisted stoma closure. J Laparoendosc Adv Surg Tech A 2007;17:395-8. [Crossref] [PubMed]
- Urushihara N, Fukumoto K, Fukuzawa H, et al. Outcome of laparoscopic modified Duhamel procedure with Z-shaped anastomosis for Hirschsprung’s disease. Surg Endosc 2012;26:1325-31. [Crossref] [PubMed]
- Travassos DV, Bax NM, Van der Zee DC. Duhamel procedure: a comparative retrospective study between an open and a laparoscopic technique. Surg Endosc 2007;21:2163-5. [Crossref] [PubMed]
- Miyano G, Koga H, Okawada M, et al. Rectal mucosal dissection commencing directly on the anorectal line versus commencing above the dentate line in laparoscopy-assisted transanal pull-through for Hirschsprung’s disease: Prospective medium-term follow-up. J Pediatr Surg 2015;50:2041-3. [Crossref] [PubMed]
- Ghirardo V, Betalli P, Mognato G, et al. Laparotomic versus laparoscopic Duhamel pull-through for Hirschsprung disease in infants and children. J Laparoendosc Adv Surg Tech A 2007;17:119-23. [Crossref] [PubMed]
- van der Zee DC, Bax NM. Duhamel-Martin procedure for Hirschsprung’s disease in neonates and infants: one-stage operation. J Pediatr Surg 1996;31:901-2. [Crossref] [PubMed]
- Smith BM, Steiner RB, Lobe TE. Laparoscopic Duhamel pullthrough procedure for Hirschsprung’s disease in childhood. J Laparoendosc Surg 1994;4:273-6. [Crossref] [PubMed]
- Wildhaber BE, Teitelbaum DH, Coran AG. Total colonic Hirschsprung’s disease: a 28-year experience. J Pediatr Surg 2005;40:203-6; discussion 206-7. [Crossref] [PubMed]
- Escobar MA, Grosfeld JL, West KW, et al. Long-term outcomes in total colonic aganglionosis: a 32-year experience. J Pediatr Surg 2005;40:955-61. [Crossref] [PubMed]
- Menezes M, Pini Prato A, Jasonni V, et al. Long-term clinical outcome in patients with total colonic aganglionosis: a 31-year review. J Pediatr Surg 2008;43:1696-9. [Crossref] [PubMed]
- Tsuji H, Spitz L, Kiely EM, et al. Management and long-term follow-up of infants with total colonic aganglionosis. J Pediatr Surg 1999;34:158-61; discussion 162. [Crossref] [PubMed]
- Blackburn S, Corbett P, Griffiths DM, et al. Total colonic aganglionosis: a 15-year single center experience. Eur J Pediatr Surg 2014;24:488-91. [Crossref] [PubMed]
- Laughlin DM, Friedmacher F, Puri P. Total colonic aganglionosis: a systematic review and meta-analysis of long-term clinical outcome. Pediatr Surg Int 2012;28:773-9. [Crossref] [PubMed]
- Peña A, Levitt MA. Colonic inertia disorders in pediatrics. Curr Probl Surg 2002;39:666-730. [PubMed]
- Suita S, Taguchi T, Ieiri S, Nakatsuji T. Hirschsprung’s disease in Japan: analysis of 3852 patients based on a nationwide survey in 30 years. J Pediatr Surg 2005;40:197-201; discussion 201-2. [Crossref] [PubMed]
Cite this article as: Miyano G, Yazaki Y, Ochi T, Shibuya S, Miyake Y, Murakami H, Lane GJ, Koga H, Okazaki T, Yamataka A. Duhamel operation for Hirschsprung’s disease; laparoscopic modified Duhamel procedure with Z-shaped anastomosis. Ann Laparosc Endosc Surg 2018;3:96.


