Laparoscopic splenopexy utilizing an extraperitoneal pocket for symptomatic wandering spleen
Introduction
Wandering spleen is a rare clinical entity characterized by an ectopic spleen. There are isolated case reports in the literature but few population studies to study the incidence, giving credence to its rarity (1). It affects both sexes and all ages with reported patients ranging from 3 months to 82 years (2).
The displacement of the wandering spleen from its normal position in the left upper quadrant (LUQ) can occur as a result of laxity in its peritoneal attachments (3). The absence of splenic suspensory ligaments can be due to congenital anomalies of the dorsal mesogastrium (4), malformation of the splenic suspensory ligaments in patients with omphalocele or congenital diaphragmatic hernia or acquired secondary to surgeries such as a Nissen fundoplication (1,3). The lack of suspensory attachments results in a mobile spleen that can easily torse around its vascular pedicle, placing the patient at risk of acute infarction of the organ (5). Patients may be asymptomatic and clinical presentation can be variable; abdominal pain, peritonitis, abscess formation, pancreatitis, or necrosis of the pancreatic tail (6,7). Diagnosis of a wandering spleen is difficult given the non-specific clinical presentations. Imaging modalities have included the use of ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI) (3,8).
The treatment for a wandering spleen is surgical with options including splenopexy or splenectomy. Given the spleen’s role in filtration of red blood cells and mounting immune responses, preservation of the organ is preferable, particularly in children. Several techniques for splenopexy have been described, ranging from the use of mesh; either a single mesh and tacking sutures (9,10) or a sandwich technique using two meshes (11), creation of retroperitoneal pouch (12), or pre-peritoneal pouch with use of adjacent organs to secure kidney to the LUQ (3). Our aim is to report the case of a 10-year-old child with imaging proven wandering spleen successfully treated with splenopexy using a novel technique involving both the creation of a pre-peritoneal pocket and a small mesh.
Case presentation
The patient is a 10-year-old male with history of ventricular septal defect (VSD) who presented to the emergency department with acute onset of transient abdominal pain. On cross-sectional imaging with a CT scan, the spleen was localized in the mid-portion of the abdomen with the splenic hilum oriented towards the posterior aspect of the abdomen. Furthermore, there were areas of splenic tissue that appeared hypointense, concerning for infarction. The patient’s physical exam was notable for a soft, non-distended, non-tender abdomen with a palpable midline abdominal mass.
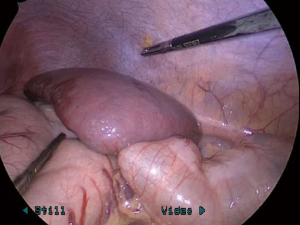
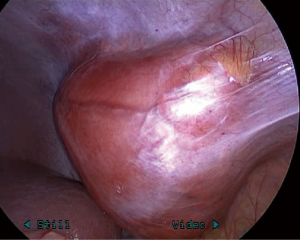
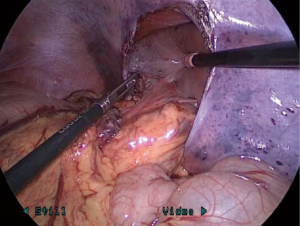
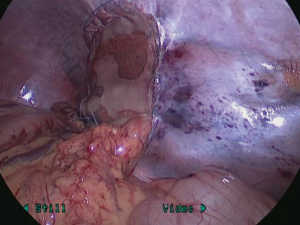
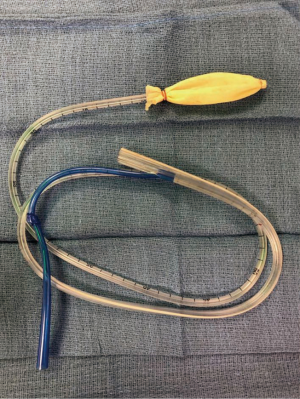
Since the patient was asymptomatic at the time of presentation, he was administered pre-operative vaccinations and subsequently underwent a laparoscopic splenopexy 2 weeks later. He had been cleared for surgery from a cardiac standpoint. At the time of surgery, the patient was placed in the supine position and the spleen was externally manipulated from the mid-abdomen to the LUQ. The patient was prepped and draped in the standard sterile fashion. The abdomen was accessed through an infraumbilical incision and insufflated to a pressure of 12 mmHg through a 5-mm trocar. Two additional 5 mm ports were placed in the left lower and right upper abdomen along the mid-clavicular lines. The spleen was examined and noted to have no ligamentous attachments (Figure 1). Next, a 1.5-cm skin incision was made in the left lateral abdominal wall just inferior to the 11th rib. Blunt dissection was performed down to the peritoneal layer after spreading the muscle layer. A large extraperitoneal subfascial pocket was created (Figure 2) mostly superior and slightly inferior to the incision first with the index finger then with an insufflated balloon (thumb portion of sterile glove) attached to an 18-Fr nasogastric tube (Figure 3). Once the peritoneal pocket was of adequate size to accommodate the spleen, the peritoneum was incised and the spleen placed carefully into the pocket, ascertaining that the hilum was correctly positioned and not torsed (Figure 4). As the peritoneal edges of the pocket came together under some tension, a small Vicryl mesh patch was placed to relieve this tension. The patch was sewn with running 3-0 Vicryl along each edge of the peritoneal opening so that the spleen lay in the peritoneal pocket without tension on the peritoneal closure (Figure 5). The hilum of the spleen was intact and not constricted in any way. The ports were removed the under direct visualization and the incisions were closed in layers.
The patient had an uneventful post-operative course and was discharged home on post-operative day 2. He has since been seen in clinic and is currently asymptomatic.
Discussion
The management of a wandering spleen remains primarily a surgical one. While patients with this condition may be asymptomatic, the inherent risks, which include torsion, rupture, and/or infarction, mandate a surgical intervention. The historical procedure of choice had been a splenectomy (13,14). However, given the spleen’s role in immunologic function and risk of developing overwhelming post-splenectomy infection (OPSI) from encapsulated organisms, every attempt should be made for splenic preservation (15). Hence, splenopexy is now the advocated surgical procedure of choice for a wandering spleen.
The presence of and/or degree of infarction at time of splenopexy is a point of divergence amongst surgeons on whether to perform total splenectomy, partial splenectomy, or continue with splenopexy. In the presence of active torsion, the spleen is commonly found to be congested and enlarged, posing obvious difficulties in performing a splenopexy. Upon detorsion, it can be difficult to predict whether the spleen will recover or whether there will be progression of necrosis. Known complications of acute splenic torsion include splenic abscess, hemorrhage from gastric varices, necrosis of the pancreatic tail, gastric outlet obstruction (16-18). In the presence of these findings, the decision to perform a splenectomy or splenopexy should be made on an individual basis. Intra-operative findings in our patient were notable for small patchy infarcts but no obvious evidence of necrosis or abscesses and the decision was made to proceed with a splenopexy.
Numerous techniques for splenopexy have been described. These have included the extremes of suturing the spleen directly to the diaphragm (19), as well as using various intra-abdominal contents to pexy the spleen. These include pexying the spleen either by its pedicle (20), suturing an omental pouch and colophrenic ligament to the lateral diaphragm (21) to create a pouch for the inferior part of the spleen, or transposing the colonic flexure and gastrocolic ligaments to the anterior diaphragm to create a pouch for the upper splenic pole (22,23). More recently, creations of peritoneal pouches have been utilized. These include dissection of posterolateral retroperitoneal pouch during a laparotomy (24) or an extraperitoneal pouch during laparoscopy (25). Use of various types of mesh have been described in various techniques; sandwich technique of using two sheets of mesh to wrap in the spleen using absorbable (26) and non-absorbable (11), laparoscopic splenopexy using absorbable Vicryl mesh using laparoscopy (10) and hand-assisted laparoscopy (27), or insertion of the spleen into a Vicryl mesh bag and fixating it to the LUQ (22). Each of the aforementioned techniques have their own advantages and disadvantages.
The technique described in this case report utilized laparoscopy over hand-assisted laparoscopy and laparotomy with the potential to minimize intra-abdominal adhesions and post-operative pain. Given the wide use of minimally invasive surgery in both the pediatric and adult population, this should be considered the preferred management option.
The use of an extra-peritoneal pouch poses the benefits of minimizing intra-abdominal dissection that would be required in some of the techniques described above, including utilization of the colophrenic or gastrocolic ligaments or mobilizing the omentum for pouch creation. We were able to create the extraperitoneal window with relative ease and required little to no intra-peritoneal dissection of planes. The skin incision was just large enough to fit a dissecting finger. The addition of the fabricated expansion balloon allowed further blunt dissection of the subfascial layer. We think this combination technique is advantageous for several reasons. Firstly, it allows for a completely blunt dissection of the pouch without the use of laparoscopic graspers. Also, the creation of the pouch is in line with the layers of the abdominal wall rather than at an angle with them. In this fashion, the integrity of the peritoneum is maintained without weakening it or tearing it. Furthermore, this technique offers relative ease and speed since the surface area of the tools used is wider and less traumatic than laparoscopic instruments. Finally, the incision is slightly larger than a port site incision and is less obvious on the lateral aspect of the abdomen. The large size of the patient’s spleen did require the use of a mesh patch to avoid placing tension upon closure of the peritoneal pocket around the spleen. We chose a Vicryl mesh, which would adhere to the surrounding spleen and peritoneum and further ensure fixation of the spleen in the pocket. In patients with normal size spleens, it may be possible to forego the use of any synthetic mesh with the described technique.
Conclusions
While wandering spleen remains an uncommon diagnosis amongst pediatric and adult patients, its prompt diagnosis and awareness of various surgical management options remains imperative for clinicians and surgeons. We propose that laparoscopic splenopexy utilizing an extraperitoneal pocket for asymptomatic wandering spleen is a safe and efficacious surgical option.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.05.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients’ parents, given his status as a minor, for publication of this case report and all accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fiquet-Francois C, Belouadah M, Ludot H, et al. Wandering spleen in children: multicenter retrospective study. J Pediatr Surg 2010;45:1519-24. [Crossref] [PubMed]
- Lane TM, South LM. Management of a wandering spleen. J R Soc Med 1999;92:84-5. [Crossref] [PubMed]
- Soleimani M, Mehrabi A, Kashfi A, et al. Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surg Today 2007;37:261-9. [Crossref] [PubMed]
- Bouassida M, Sassi S, Chtourou MF, et al. A wandering spleen presenting as a hypogastric mass: case report. Pan Afr Med J 2012;11:31. [PubMed]
- Cohen MS, Soper NJ, Underwood RA, et al. Laparoscopic splenopexy for wandering (pelvic) spleen. Surg Laparosc Endosc 1998;8:286-90. [Crossref] [PubMed]
- Sodhi KS, Saggar K, Sood BP, et al. Torsion of a wandering spleen: acute abdominal presentation. J Emerg Med 2003;25:133-7. [Crossref] [PubMed]
- Lebron R, Self M, Mangram A, et al. Wandering spleen presenting as recurrent pancreatitis. JSLS 2008;12:310-3. [PubMed]
- Allen KB, Gay BB Jr, Skandalakis JE. Wandering spleen: anatomic and radiologic considerations. South Med J 1992;85:976-84. [Crossref] [PubMed]
- Morgan S, Glenn I, Soldes O. Laparoscopic splenopexy for wandering spleen, a video demonstration of technique by encircling the spleen with polyglactin 910 woven mesh. Surg Endosc 2017;31:5427-8. [Crossref] [PubMed]
- Haj M, Bickel A, Weiss M, et al. Laparoscopic splenopexy of a wandering spleen. J Laparoendosc Adv Surg Tech A 1999;9:357-60. [Crossref] [PubMed]
- Palanivelu C, Rangarajan M, Senthilkumar R, et al. Laparoscopic mesh splenopexy (sandwich technique) for wandering spleen. JSLS 2007;11:246-51. [PubMed]
- Schaarschmidt K, Lempe M, Kolberg-Schwerdt AS, et al. The technique of laparoscopic retroperitoneal splenopexy for symptomatic wandering spleen in childhood. J Pediatr Surg 2005;40:575-7. [Crossref] [PubMed]
- Gigot JF, Legrand M, Cadiere GB, et al. Is laparoscopic splenectomy a justified approach in hematologic disorders? Preliminary results of a prospective multicenter study. Belgian Group for Endoscopic Surgery. Int Surg 1995;80:299-303. [PubMed]
- Sarimurat N, Tekant GT, Huseyin S, et al. Wandering spleen in childhood: a report of three cases. Surg Today 1997;27:1086-8. [Crossref] [PubMed]
- Theilacker C, Ludewig K, Serr A, et al. Overwhelming Postsplenectomy Infection: A Prospective Multicenter Cohort Study. Clin Infect Dis 2016;62:871-8. [Crossref] [PubMed]
- Brown CV, Virgilio GR, Vazquez WD. Wandering spleen and its complications in children: a case series and review of the literature. J Pediatr Surg 2003;38:1676-9. [Crossref] [PubMed]
- Sheflin JR, Lee CM, Kretchmar KA. Torsion of wandering spleen and distal pancreas. AJR Am J Roentgenol 1984;142:100-1. [Crossref] [PubMed]
- Lin CH, Wu SF, Lin WC, et al. Wandering spleen with torsion and gastric volvulus. J Formos Med Assoc 2005;104:755-8. [PubMed]
- Bar-Maor JA, Sweed Y. Treatment of Intermittent Splenic Torsion in Polysplenia Syndrome and Wandering Spleen by Splenopexy. Pediatr Surg Int 1989;4:130-3. [Crossref]
- Stringel G, Soucy P, Mercer S. Torsion of the Wandering Spleen - Splenectomy or Splenopexy. J Pediatr Surg 1982;17:373-5. [Crossref] [PubMed]
- Maxwell-Armstrong CA, Clarke ED, Tsang TM, et al. The wandering spleen. Arch Dis Child 1996;74:247-8. [Crossref] [PubMed]
- Peitgen K, Majetschak M, Walz MK. Laparoscopic splenopexy by peritoneal and omental pouch construction for intermittent splenic torsion ("wandering spleen"). Surg Endosc 2001;15:413. [Crossref] [PubMed]
- Caracciolo F, Bonatti PL, Castrucci G, et al. Wandering spleen: treatment with colonic displacement. J R Coll Surg Edinb 1986;31:242-4. [PubMed]
- Steinberg R, Karmazyn B, Dlugy E, et al. Clinical presentation of wandering spleen. J Pediatr Surg 2002;37:E30 [Crossref] [PubMed]
- Martínez-Ferro M, Elmo G, Laje P. Laparoscopic pocket splenopexy for wandering spleen: a case report. J Pediatr Surg 2005;40:882-4. [Crossref] [PubMed]
- Nomura H, Haji S, Kuroda D, et al. Laparoscopic splenopexy for adult wandering spleen: sandwich method with two sheets of absorbable knitted mesh. Surg Laparosc Endosc Percutan Tech 2000;10:332-4. [Crossref] [PubMed]
- Cripps M, Svahn J. Video. Hand-assisted laparoscopy for wandering spleen. Surg Endosc 2011;25:312. [Crossref] [PubMed]
Cite this article as: Shakoor A, DeFazio J, Zenilman A, Li L, Duron VP. Laparoscopic splenopexy utilizing an extraperitoneal pocket for symptomatic wandering spleen. Ann Laparosc Endosc Surg 2018;3:53.