Rectal cancer—state of art of laparoscopic versus open surgery
Introduction
Since its introduction, laparoscopy has gained more and more consent in colorectal surgery, becoming the Gold Standard for the surgical treatment of colon cancer (1). On the contrary, its role in rectal cancer surgery is still controversial and widely debated. In fact rectal cancer surgery results more technically difficult than the colonic one, due to the narrow space of the pelvis, which gets laparoscopic surgery particularly challenging. For this reason laparoscopic rectal surgery gets performed only in specialized centers worldwide.
In the last decade accumulating evidence has demonstrated that recovery after laparoscopy is faster and better, moreover laparoscopic rectal resection has been proven equivalent to the traditional technique in terms of short-terms outcomes. Nevertheless, its oncologic safety remains unclear and doubts about pathologic outcomes are still open and worsened by new evidence reported by the most recent international studies. With this study we aim to present the ongoing situation of laparoscopic treatment for rectal cancer by reviewing the current literature.
Materials and methods
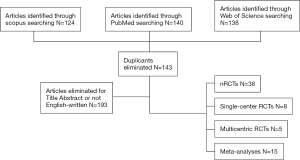
To identify all possible studies regarding the comparison between laparoscopic and open rectal resection for rectal cancer and to make the state of art of laparoscopic rectal resection, we performed a systematic search in the electronic databases (PubMed, Web of Science, Scopus, EMBASE) according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (2). We limited the search until 31 March 2017 and used the following search terms in all possible combinations: rectal cancer, laparoscopy, minimally invasive and open surgery. We included only English-written articles comparing laparoscopic surgery to the open technique for rectal cancer treatment.
Results
The search produced 402 articles; 143 were duplicates and were removed. Two independent Authors evaluated the remaining articles excluding the ones that were not pertinent (not comparing laparoscopy to the traditional technique in rectal cancer treatment) or not English-written. Reviews were excluded too resulting in 66 articles, of which 38 are non-randomized trials, 8 are randomized controlled trials (RCTs) performed in a single center, 5 are multicentric RCTs and 15 are meta-analyses (Figure 1).
Articles included in this review have been divided in four categories: non RCTs, single-center RCT, multicentric RCTs, meta-analyses; and chronologically ordered in Tables 1-4.
Table 1
| Author | Title | Year | Journal | Type | Patients | Lap | Open |
|---|---|---|---|---|---|---|---|
| Fleshman et al. (3) | Laparoscopic versus open abdominoperineal resection for cancer | 1999 | Diseases of the Colon & Rectum | Retrospective | 194 | 42 | 152 |
| Leung et al. (4) | Laparoscopic-assisted abdominoperineal resection for low rectal adenocarcinoma | 2000 | Surgical Endoscopy | Study-control | 59 | 25 | 34 |
| Anthuber et al. (5) | Outcome of laparoscopic surgery for rectal cancer in 101 patients | 2003 | Diseases of the Colon & Rectum | Retrospective | 435 | 101 | 334 |
| Feliciotti et al. (6) | Long-term results of laparoscopic versus open resections for rectal cancer for 124 unselected patients | 2003 | Surgical Endoscopy | Retrospective | 86 | 52 | 34 |
| Hu et al. (7) | Comparative evaluation of immune response after laparoscopical and open total mesorectal excisions with anal sphincter preservation in patients with rectal cancer | 2003 | World Journal of Gastroenterology | Retrospective | 45 | 20 | 25 |
| Wu et al. (8) | Laparoscopic versus conventional open resection of rectal carcinoma: a clinical comparative study | 2004 | World Journal of Gastroenterology | Retrospective | 36 | 18 | 18 |
| Morino et al. (9) | Laparoscopic versus open surgery for extraperitoneal rectal cancer: a prospective comparative study | 2005 | Surgical Endoscopy | Retrospective | 191 | 98 | 93 |
| Law et al. (10) | Laparoscopic and open anterior resection for upper and mid rectal cancer: an evaluation of outcomes | 2006 | Diseases of the Colon & Rectum | Retrospective | 265 | 98 | 167 |
| Lelong et al. (11) | Short-term outcome after laparoscopic or open restorative mesorectal excision for rectal cancer: a comparative cohort study | 2007 | Diseases of the Colon & Rectum | Retrospective | 172 | 104 | 68 |
| Veenhof et al. (12) | Laparoscopic versus open total mesorectal excision: a comparative study on short-term outcomes: a single-institution experience regarding anterior resections and abdominoperineal resections | 2007 | Digestive Surgery | Retrospective | 100 | 50 | 50 |
| Staudacher et al. (13) | Laparoscopic versus open total mesorectal excision in unselected patients with rectal cancer: impact on early outcome | 2007 | Diseases of the Colon & Rectum | Retrospective | 187 | 108 | 79 |
| Mirza et al. (14) | Long-term outcomes for laparoscopic versus open resection of nonmetastatic colorectal cancer | 2008 | Journal of Laparoendoscopic & Advanced Surgical Techniques | Retrospective | 92 | 54 | 38 |
| Ströhlein et al. (15) | Comparison of laparoscopic versus open access surgery in patients with rectal cancer: a prospective analysis | 2008 | Diseases of the Colon & Rectum | Prospective | 389 | 114 | 275 |
| Yu et al. (16) | Laparoscopic versus open total mesorectal excision for the middle-lower rectal cancer: a clinical comparative study | 2009 | Chinese Journal of Gastrointestinal Surgery | Retrospective | 198 | 93 | 105 |
| González et al. (17) | Laparoscopic versus open total mesorectal excision: a nonrandomized comparative prospective trial in a tertiary center in Mexico City | 2009 | The American Journal of Surgery | Prospective | 56 | 28 | 28 |
| Gouvas et al. (18) | Laparoscopic or open surgery for the cancer of the middle and lower rectum short-term outcomes of a comparative non-randomised study | 2009 | International Journal of Colorectal Disease | Retrospective | 88 | 45 | 43 |
| Khaikin et al. (19) | Laparoscopic versus open proctectomy for rectal cancer: patients’ outcome and oncologic adequacy | 2009 | Surgical Laparoscopy Endoscopy & Percutaneous Techniques | Retrospective | 82 | 32 | 50 |
| Koulas et al. (20) | Evaluations of laparoscopic proctocolectomy versus traditional technique in patients with rectal cancer | 2009 | Journal of the Society of Laparoendoscopic Surgeons | Retrospective | 117 | 57 | 60 |
| Laurent et al. (21) | Laparoscopic versus open surgery for rectal cancer: long-term oncologic results | 2009 | Annals of Surgery | Retrospective | 471 | 238 | 233 |
| Baik et al. (22) | Laparoscopic versus open resection for patients with rectal cancer: comparison of perioperative outcomes and long-term survival | 2011 | Diseases of the Colon & Rectum | Case-matched controlled prospective | 162 | 54 | 108 |
| McKay et al. (23) | Improved short-term outcomes of laparoscopic versus open resection for colon and rectal cancer in an area health service: a multicenter study | 2011 | Diseases of the Colon & Rectum | Retrospective | 545 | 157 | 388 |
| Gunka et al. (24) | Long-term results of laparoscopic versus open surgery for nonmetastatic colorectal cancer | 2011 | Acta Chirurgica Belgica | Retrospective | 145 | 75 | 70 |
| Siani et al. (25) | Laparoscopic versus open total mesorectal excision for stage I-III mid and low rectal cancer: a retrospective 5 years analysis | 2012 | Il Giornale di Chirurgia | Retrospective | 60 | 30 | 30 |
| Jefferies et al. (26) | Oncological outcome after laparoscopic abdominoperineal excision of the rectum | 2012 | Colorectal Disease | Retrospective | 41 | 16 | 25 |
| Kellokumpu et al. (27) | Short- and long-term outcome following laparoscopic versus open resection for carcinoma of the rectum in the multimodal setting | 2012 | Diseases of the Colon & Rectum | Retrospective | 191 | 100 | 91 |
| Seshadri et al. (28) | Laparoscopic versus open surgery for rectal cancer after neoadjuvant chemoradiation: a matched case-control study of short-term outcomes | 2012 | Surgical Endoscopy | Retrospective | 144 | 72 | 72 |
| Kang et al. (29) | The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison—open, laparoscopic, and robotic surgery | 2013 | Annals of Surgery | Retrospective | 330 | 165 | 165 |
| Lujan et al. (30) | Laparoscopic versus open surgery for rectal cancer: results of a prospective multicentre analysis of 4,970 patients | 2013 | Surgical Endoscopy | Prospective | 4,405 | 1,387 | 3,018 |
| Wilson et al. (31) | Laparoscopic colectomy is associated with a lower incidence of postoperative complications than open colectomy: a propensity score-matched cohort analysis | 2014 | Colorectal Disease | Retrospective cohort study | 37,249 | 15,643 | 21,606 |
| Moghadamyeghaneh et al. (32) | Outcomes of open, laparoscopic, and robotic Abdominoperineal resections in patients with rectal cancer | 2015 | Diseases of the Colon & Rectum | Retrospective | 17,496 | 4737 | 12759 |
| Midura et al. (33) | The effect of surgical approach on short-term oncologic outcomes in rectal cancer surgery | 2015 | Surgery | Retrospective | 8,272 | 2,337 | 5,935 |
| Dural et al. (34) | The role of the laparoscopy on circumferential resection margin positivity in patients with rectal cancer: long-term outcomes at a single high-volume institution | 2015 | Surgical Laparoscopy Endoscopy & Percutaneous Techniques | Retrospective | 579 | 266 | 313 |
| Cho et al. (35) | Minimally invasive versus open total mesorectal excision for rectal cancer: long-term results from a case-matched study of 633 patients | 2015 | Surgery | Retrospective | 633 | 211 | 422 |
| Kim et al. (36) | Long-term outcomes of laparoscopic versus open surgery for rectal cancer: a single-center retrospective analysis | 2015 | The Korean Journal of Gastroenterology | Retrospective | 307 | 131 | 176 |
| Zaharie et al. (37) | Laparoscopic rectal resection versus conventional open approach for rectal cancer - a 4-year experience of a single center | 2015 | Journal of BUON | Retrospective | 172 | 29 | 143 |
| de Jesus et al. (38) | The circumferential resection margins status: a comparison of robotic, laparoscopic and open total mesorectal excision for mid and low rectal cancer | 2016 | European Journal of Surgical Oncology | Retrospective | 241 | 41 | 200 |
Table 2
| Author | Title | Year | Journal | Type | Patients | Lap | Open |
|---|---|---|---|---|---|---|---|
| Araujo et al. (39) | Conventional approach x laparoscopic abdominoperineal resection for rectal cancer treatment after neoadjuvant chemoradiation: results of a prospective randomized trial | 2003 | Revista do Hospital das Clínicas | Prospective | 28 | 13 | 15 |
| Zhou et al. (40) | Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer | 2004 | Surgical Endoscopy | Prospective | 171 | 82 | 89 |
| Braga et al.(41) | Laparoscopic resection in rectal cancer patients: outcome and cost-benefit analysis | 2007 | Diseases of the Colon & Rectum | Prospective | 168 | 83 | 85 |
| Pechlivanides et al. (42) | Lymph node clearance after total mesorectal excision for rectal cancer: laparoscopic versus open approach | 2007 | Digestive Diseases | Prospective | 73 | 34 | 39 |
| Ng et al. (43) | Laparoscopic-assisted versus open abdominoperineal resection for low rectal cancer: a prospective randomized trial | 2008 | Annals of Surgical Oncology | Prospective | 99 | 51 | 48 |
| Lujan et al. (44) | Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer | 2009 | Surgical Endoscopy | Prospective | 204 | 101 | 103 |
| Liang et al. (45) | Effectiveness and safety of laparoscopic resection versus open surgery in patients with rectal cancer: a randomized, controlled trial from China | 2011 | Journal of Laparoendoscopic & Advanced Surgical Techniques | Prospective | 343 | 169 | 174 |
| Ng et al. (46) | Laparoscopic-assisted versus open total mesorectal excision with anal sphincter preservation for mid and low rectal cancer: a prospective, randomized trial | 2014 | Surgical Endoscopy | Prospective | 80 | 40 | 40 |
| Fujii et al. (47) | Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients | 2014 | Surgical Endoscopy | Prospective | 200 | 100 | 100 |
Table 3
| Author | Title | Year | Journal | Type | Patients | Lap | Open |
|---|---|---|---|---|---|---|---|
| Guillou et al. (48) | Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicenter, randomized controlled trial | 2005 | Lancet | Prospective | 794 | 526 | 628 |
| van der Pas et al. (49) | Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial | 2013 | Lancet Oncology | Prospective | 1,103 | 739 | 364 |
| Kang et al. (50) | Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. | 2014 | Lancet Oncology | Prospective | 340 | 170 | 170 |
| Fleshman et al. (51) | Effect of laparoscopic-assisted resection versus open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial | 2015 | JAMA | Prospective | 462 | 240 | 222 |
| Stevenson et al. (52) | Effect of Laparoscopic-Assisted Resection versus open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial | 2015 | JAMA | Prospective | 475 | 238 | 237 |
RCT, randomized controlled trial.
Table 4
| Author | Title | Year | Journal | Patients | Lap | Open |
|---|---|---|---|---|---|---|
| Aziz et al. (53) | Laparoscopic versus open surgery for rectal cancer: a meta-analysis | 2006 | Annals of Surgical Oncology | 2,071 | 909 | 1,162 |
| Gao et al. (54) | Meta-analysis of short-term outcomes after laparoscopic resection for rectal cancer | 2006 | International Journal of Colorectal Disease | 643 | 285 | 358 |
| Bonjer et al. (55) | Laparoscopically assisted versus open colectomy for colon cancer: a meta-analysis | 2007 | Archives of surgery | 1,765 | 796 | 740 |
| Anderson et al. (56) | Oncologic outcomes of laparoscopic surgery for rectal cancer: a systematic review and meta-analysis of the literature | 2008 | European Journal of Surgical Oncology | 2,178 | 1,403 | 1,775 |
| Gong et al. (57) | A meta-analysis of clinical outcomes after laparoscopic operation for rectal cancer | 2010 | Chinese Journal of Gastrointestinal Surgery | 2,850 | 1,145 | 1,705 |
| Ohtani et al. (58) | A meta-analysis of the short- and long-term results of randomized controlled trials that compared laparoscopy-assisted and conventional open surgery for rectal cancer | 2011 | Journal of Gastrointestinal Surgery | 2,095 | 1,096 | 999 |
| Huang et al. (59) | Laparoscopic-assisted versus open surgery for rectal cancer: a meta-analysis of randomized controlled trials on oncologic adequacy of resection and long-term oncologic outcomes | 2011 | International Journal of Colorectal Disease | 1,033 | – | – |
| Ng et al. (60) | Long-term oncologic outcomes of laparoscopic versus open surgery for rectal cancer: a pooled analysis of 3 randomized controlled trials | 2012 | Annals of Surgery | 278 | 136 | 142 |
| Trastulli et al. (61) | Laparoscopic versus open resection |
2012 | Colorectal Disease | 1,544 | 841 | 703 |
| Arezzo et al. (62) | Laparoscopy for rectal cancer reduces short-term mortality and morbidity: results of a systematic review and meta-analysis | 2013 | Surgical Endoscopy | 4,539 | 2,087 | 2,452 |
| Ahmad et al. (63) | A systematic review and meta-analysis of randomized and non-randomized studies comparing laparoscopic and open abdominoperineal resection for rectal cancer | 2013 | Colorectal Disease | 454 | 248 | 206 |
| Vennix et al. (64) | Laparoscopic versus open total mesorectal excision for rectal cancer | 2014 | The Cochrane Database of Systematic Reviews | 4,224 | – | – |
| Zhang et al. (65) | Laparoscopic versus open surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials | 2014 | Asian Pacific Journal of Cancer Prevention | 3,045 | 1,804 | 1,241 |
| Jiang et al. (1) | Laparoscopic versus open surgery for mid-low rectal cancer: a systematic review and meta-analysis on short- and long-term outcomes | 2015 | Journal of Gastrointestinal Surgery | 3,678 | – | – |
| Chen et al. (66) | Laparoscopic versus open surgery for rectal cancer: a meta-analysis of classic randomized controlled trials and high-quality nonrandomized studies in the last 5 years | 2017 | International Journal of Surgery | 4,353 | 2,251 | 2,102 |
Discussion
Rectal cancer is a worldwide disease that constitutes one-third of colorectal cancers (67) and whose incidence has increased significantly in the last decades (68). The main treatment for rectal cancer is the surgical resection, which results have drastically improved since the introduction of total mesorectal excision (TME).
Thanks to accumulating evidence indicating that laparoscopic treatment of colon carcinoma is considered equivalent to the open technique, the laparoscopic technique is widely accepted and performed in the treatment of colon carcinoma. On the contrary, the role of laparoscopy in the treatment of rectal cancer is still not clear. Laparoscopic rectal surgery is more difficult than colonic one, due to the narrow space of pelvic cavity and the oncological safety remains unclear. Therefore, laparoscopy in rectal cancer is still not recommended as the gold standard treatment by international guidelines.
Anyhow the open approach too presents several limitations, especially in terms of oncologic outcomes, as it has been demonstrated by Rickles et al. (69) who reported a 22% less risk of positive circumferential resection margin (CRM) after laparoscopic surgery compared to an open approach.
All these reasons led to the current interest of surgeons towards new techniques, such as the use of robotics, transanal approach (taTME) or the combination of laparoscopy and transanal approach for rectal cancer surgery.
During the last decade many studies have been performed to prove the safety and feasibility of laparoscopic-assisted resection for rectal cancer. In order to demonstrate the non-inferiority of the laparoscopic approach against the open surgery, Authors all over the world have compared the two techniques in terms of short- and long-term outcomes.
Most of these studies are non-randomized comparative (3-20) trials (NRCTs) (21-38). The findings of these studies were extremely encouraging, showing the non-inferiority of laparoscopy compared to the open technique in terms of oncological outcomes (like disease-free survival and local recurrence) and intraoperative and postoperative factors. Moreover the laparoscopic group presented advantages regarding antibiotic and analgesic therapy, early mobilization, hospital stay, intraoperative blood loss, resuming oral nutrition, bowel transit resumption, postoperative complications and wound complications, concluding that laparoscopic resection for rectal cancer is feasible, safe and effective.
To collect more accurate evidence about short- and long-term outcomes after laparoscopic surgery for rectal cancer compared to open surgery, a large number of randomized control trials (RCTs) have been produced in the last few years (39-47). Most of these studies focused on postoperative morbidity, length of hospital stay, quality of life, long-term survival, and local recurrences, finding no significant difference between the groups.
For an example, a recent study was developed by Ng et al. (43) who performed a single-center, prospective, randomized trial on 80 patients with mid and low rectal cancer, focusing on oncologic outcomes (in particular quality of the TME specimen, circumferential resection margin (CRM) involvement, and number of lymph nodes removed), which were found similar between both groups.
The results assessed with these randomized trials seem to suggest that laparoscopic surgery for rectal cancer could improve short-term results while not jeopardizing the oncological outcomes compared with open surgery. The major limitation of these studies is that, being single-centered they are based on an exiguous number of patients.
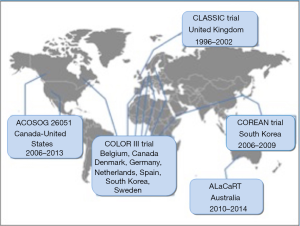
To reach a wider number of patients multicentric studies have been designed and performed all over the world in the last 20 years (Figure 2).
In the CLASICC trial (48) 794 patients with colorectal cancer from 27 UK centers were enrolled to be treated by either laparoscopic or open surgery. Primary short-term end-points were positivity rates of circumferential and longitudinal resection margins and in-hospital mortality. In the CLASICC trial, regarding the cancer of the rectum, no significant difference in CRM positivity was detected in patients who underwent a rectal resection in both laparoscopic and open group. CRM positivity, instead, was significantly greater in laparoscopic than in the open surgery group for patients who underwent anterior resection. It is important to highlight that positive CRM is a strong predictor of both local recurrence and overall survival, since it is associated with a high rate of local recurrence and poor morbidity and mortality for rectal cancer patients (69). As a first conclusion, at the time of its first publication, the impair short-term outcomes after a laparoscopic approach in an anterior resection of the rectum did not justify its routine use. Further studies about long-term outcomes of patient enrolled in the CLASICC trial, have been recently published focusing on the local recurrence, overall survival and disease-free survival (70,71). No significant differences between the laparoscopic and open approach were found in local recurrence, overall survival and disease-free survival after 3, 5 and 10 years follow-up. However, it is worth mentioning that the CLASICC trial (48) enrolled not only patients with rectal cancer but also patients with colon cancer, which may cause confusion on conclusions about rectal cancer.
Two other multicentric studies, aimed to compare laparoscopic and open surgery in patients with rectal cancer, were the COLOR II trial (49) and the COREAN trial (50), enrolling respectively 1,103 patients with rectal cancer within 15 cm from the anal verge and 340 patients with II and III mid- and low rectal cancer. Both studies demonstrated similar results in oncologic outcomes, disease-free survival and recurrence, confirming the safety and feasibility of the laparoscopic approach for rectal cancer. COLOR II trial was performed in 30 centers and hospitals from eight countries from 2004 to 2010. As expected, blood loss and recovery resulted better after the laparoscopic approach, even if it was connected to longer operative time. In terms of safety, completeness of the resection, positive CM (<2 mm) and median tumor distance to distal resection margin did not differ significantly between the groups. Also morbidity and mortality within 28 days after surgery were similar. So the authors concluded that laparoscopic surgery resulted in similar safety to open surgery and associated to a better recovery, if performed in selected patients treated by skilled surgeons.
The COREAN trial (50) was performed in three centers from 2006 to 2009 in South Korea. Its conclusions were similar to the COLOR II trial (49): although surgery time was longer in the laparoscopic group, no significant difference was found in the involvement of the CRM, macroscopic quality of the TME specimen, number of harvested lymph nodes, and perioperative morbidity, once again stating the efficacy and safety of laparoscopic rectal resection.
More recently, two multicentric studies have been published, introducing controversial conclusions about the non-inferiority of laparoscopic surgery compared with open surgery. In the ALaCaRT Randomized Clinical Trial conducted between 2010 and 2014, 475 randomized patients with T1–T3 rectal adenocarcinoma, underwent either laparoscopic [237] or open [238] rectal resection (52). The primary end point was several oncological factors selected to an adequate surgical resection. A successful resection was achieved in 194 patients (82%) who underwent laparoscopic surgery and 208 patients (89%) who received open surgery. CRM was clear in 93% of patients in the laparoscopy group and in 97% who underwent open surgery. Distal margin was clear in 99% of cases in both groups, and TME was complete in 87% of patients in the laparoscopic surgery group and 92% in the open surgery group. Based on these findings the Authors concluded that, among patients with T1–T3 rectal tumors, there was not sufficient evidence to establish the non-inferiority of laparoscopic surgery compared to open surgery, so the choice of a laparoscopic approach for a patient with rectal cancer should be made with caution.
Similar evidence was found by Fleshman et al. in the ACOSOG Z6051 randomized clinical trial (51). A multicenter randomized trial enrolling patients from 35 institutions across United States and Canada, between 2008 and 2013. A total of 486 patients with a stage II or III rectal cancer within 12 cm from the anal verge were randomized after neoadjuvant therapy to receive a laparoscopic [240] or an open [222] resection. The aim of the study was to assess whether laparoscopic resection was not inferior to open resection, based on pathologic and histologic evaluation of the resected specimen. Successful resection occurred in 81.7% of laparoscopic resection cases and 86.9% of open resection cases and did not support the non-inferiority. These results too do not support the use of laparoscopic resection in patients with stage II or III rectal cancer.
It’s important to notice that the chosen outcome to assess the efficacy of laparoscopic surgery in rectal cancer was a composite of a CRM greater than 1 mm, distal margin without tumor, and completeness of TME. This combination of short-terms outcomes has been arbitrarily chosen by the Authors and it still has to be proven its real impact on recurrence and long-term survival. So, both studies share the main limitation: the non-inferiority of laparoscopy compared to open surgery is based on the combination of completeness of TME and the positivity of CRM which, as short-terms outcomes, are only predictors of local recurrence. Long-terms outcomes are needed to define laparoscopy inferior compared to the traditional approach.
Moreover, although the results of the comparison between laparoscopy and open technique in terms of successful resection do not support the non-inferiority of laparoscopy, taken singularly, CRM and TME in the ALaCaRT trial are very close to be significant (P=0.06) and then equivalent in open and laparoscopic surgery.
Finally both studies do not take under consideration short-terms outcomes, like recovery, which has been worldwide demonstrated faster and associated with a lower rate of incidence of complications after laparoscopic surgery.
In the past 10 years meta-analytic studies have been performed to be able to give definitive results by pooling together a wide number of patients. Studies before the publication of ACOSOG and ALaCaRT protocols (51,52) stated the non-inferiority of laparoscopy compared to the open approach for rectal resection. Although their optimistic conclusions, we must underline how these studies share some limitations. Many of them, in fact, included non-RCT studies in the analysis that can lead to misleading results due to a selection bias.
The most recent meta-analytic study (72) has been published in February 2017, including ASOCOG and ALaCaRT trials (51,52), as well as 12 other unique RCTs with a total of 4,034 patients.
Including ALaCaRT e ACOSOG (51,52) the Authors came to the conclusion that the risk for achieving an incomplete mesorectal excision is significantly higher in patients undergoing laparoscopic rectal resection compared to the open technique, dampening the enthusiasm in support of laparoscopy for rectal surgery.
In conclusion, due to its impressing outcomes in terms of post-operative recovery and low rate of complication, laparoscopy has been seen for many years as the answer for rectal surgery. For the first time, after decades of certain advantages of laparoscopy, we are now witnessing the questioning of its equivalence to the traditional technique in terms of oncologic outcomes (Table 5). So the answers is yet to be found: to assess if the results of ongoing multicentric RCTs have a real impact on the disease-free and overall survival of patients undergoing rectal surgery performed with laparoscopic technique, thus we will have to wait for their long-term results. Only in the next future, in fact, we will be able to assess if the failure of laparoscopy in these trials in terms of pathologic outcomes will bring to an actual increase of recurrence and mortality, alongside a shortage of the disease-free survival. This should give the rationale to perform new meta-analyses based on the new evidence produced. Moreover, even more multicentric RCTs studies, hypothetically designed on new pathological outcomes, should be performed to finally assess if laparoscopy is a valid choice for the treatment of rectal cancer.
Table 5
| Author | Protocol | Countries | Years | Number of patients | Distal margin | Completeness of TME | CRM | Long-term recurrence |
|---|---|---|---|---|---|---|---|---|
| Guillou et al. (48) | CLASICC | UK | 1996–2002 | 794 | Yes | No | Yes | Yes |
| van der Pas et al. (49) | COLOR II | Belgium, Canada, Denmark, Germany, Netherland, Spain, South Korea, Sweden | 2004–2010 | 1,103 | Yes | Yes | Yes | Yes |
| Kang et al. (50) | COREAN | South Korea | 2006–2009 | 340 | No | Yes | Yes | Yes |
| Fleshman et al. (51) | ACOSOG Z6051 | United States, Canada | 2008–2013 | 486 | Yes | Yes | Yes | No |
| Stevenson et al. (52) | ALaCaRT | Australia | 2010–2014 | 475 | Yes | Yes | Yes | No |
CRM, circumferential resection margin; TME, total mesorectal excision.
Furthermore, the controversial findings we are facing could be explained by the fact that TME is challenging at baseline, working in the deep pelvis, with rigid instruments, from angles that require complicated maneuvers results even more difficult. It is possible that future developing of instruments, the introduction of different technologies such as robotics and the introduction of new techniques like taTME will improve efficacy of minimally invasive techniques and exceed the limitations of laparoscopy (12).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Minimally Invasive Treatment of Low Rectal Cancer”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.08.10). The series “Minimally Invasive Treatment of Low Rectal Cancer” was commissioned by the editorial office without any funding or sponsorship. Milone M served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Aug 2016 to Jul 2018. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jiang JB, Jiang K, Dai Y, et al. Laparoscopic Versus Open Surgery for Mid-Low Rectal Cancer: a Systematic Review and Meta-Analysis on Short- and Long-Term Outcomes. J Gastrointest Surg 2015;19:1497-512. [Crossref] [PubMed]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [Crossref] [PubMed]
- Fleshman JW, Wexner SD, Anvari M, et al. Laparoscopic vs. open abdominoperineal resection for cancer. Dis Colon Rectum 1999;42:930-9. [Crossref] [PubMed]
- Leung KL, Kwok SP, Lau WY, et al. Laparoscopic-assisted abdominoperineal resection for low rectal adenocarcinoma. Surg Endosc 2000;14:67-70. [Crossref] [PubMed]
- Anthuber M, Fuerst A, Elser F, et al. Outcome of laparoscopic surgery for rectal cancer in 101 patients. Dis Colon Rectum 2003;46:1047-53. [Crossref] [PubMed]
- Feliciotti F, Guerrieri M, Paganini AM, et al. Long-term results of laparoscopic vs. open resections for rectal cancer for 124 unselected patients. Surg Endosc 2003;17:1530-5. [Crossref] [PubMed]
- Hu JK, Zhou ZG, Chen ZX, et al. Comparative evaluation of immune response after laparoscopical and open total mesorectal excisions with anal sphincter preservation in patients with rectal cancer. World J Gastroenterol 2003;9:2690-4. [Crossref] [PubMed]
- Wu WX, Sun YM, Hua YB, et al. Laparoscopic vs. conventional open resection of rectal carcinoma: A clinical comparative study. World J Gastroenterol 2004;10:1167-70. [PubMed]
- Morino M, Allaix ME, Giraudo G, et al. Laparoscopic vs. open surgery for extraperitoneal rectal cancer: a prospective comparative study. Surg Endosc 2005;19:1460-7. [Crossref] [PubMed]
- Law WL, Lee YM, Choi HK, et al. Laparoscopic and open anterior resection for upper and mid rectal cancer: an evaluation of outcomes. Dis Colon Rectum 2006;49:1108-15. [Crossref] [PubMed]
- Lelong B, Bege T, Esterni B, et al. Short-Term Outcome After Laparoscopic or Open Restorative Mesorectal Excision for Rectal Cancer: A Comparative Cohort Study. Dis Colon Rectum 2007;50:176-83. [Crossref] [PubMed]
- Veenhof AAFA, Engel AF, Craanen ME, et al. Laparoscopic versus open total mesorectal excision: a comparative study on short-term outcomes. A single-institution experience regarding anterior resections and abdominoperineal resections. Dig Surg 2007;24:367-74. [Crossref] [PubMed]
- Staudacher C, Vignali A, Saverio DP, et al. Laparoscopic vs. open total mesorectal excision in unselected patients with rectal cancer: impact on early outcome. Dis Colon Rectum 2007;50:1324-31. [Crossref] [PubMed]
- Mirza MS, Longman RJ, Farrokhyar F, et al. Long-term outcomes for laparoscopic vs. open resection of nonmetastatic colorectal cancer. J Laparoendosc Adv Surg Tech A 2008;18:679-85. [Crossref] [PubMed]
- Ströhlein MA, Grützner KU, Jauch KW, et al. Comparison of laparoscopic vs. open access surgery in patients with rectal cancer: a prospective analysis. Dis Colon Rectum 2008;51:385-91. [Crossref] [PubMed]
- Yu J, Zhang C, Wang Y, et al. Laparoscopic vs. open total mesorectal excision for the middle-lower rectal cancer: a clinical comparative study. Zhonghua Wei Chang Wai Ke Za Zhi 2009;12:573-6. [PubMed]
- González QH, Rodríguez-Zentner HA, Moreno-Berber JM, et al. Laparoscopic versus open total mesorectal excision: a nonrandomized comparative prospective trial in a tertiary center in Mexico City. Am Surg 2009;75:33-8. [PubMed]
- Gouvas N, Tsiaoussis J, Pechlivanides G, et al. Laparoscopic or open surgery for the cancer of the middle and lower rectum short-term outcomes of a comparative non-randomised study. Int J Colorectal Dis 2009;24:761-9. [Crossref] [PubMed]
- Khaikin M, Bashankaev B, Person B, et al. Laparoscopic vs. open proctectomy for rectal cancer: patients’ outcome and oncologic adequacy. Surg Laparosc Endosc Percutan Tech 2009;19:118-22. [Crossref] [PubMed]
- Koulas SG, Pappas-Gogos G, Spirou S, et al. Evaluations of laparoscopic proctocolectomy vs. traditional technique in patients with rectal cancer. JSLS 2009;13:564-73. [Crossref] [PubMed]
- Laurent C, Leblanc F, Wütrich P, et al. Laparoscopic versus open surgery for rectal cancer: long-term oncologic results. Ann Surg 2009;250:54-61. [Crossref] [PubMed]
- Baik SH, Gincherman M, Mutch MG, et al. Laparoscopic vs open resection for patients with rectal cancer: comparison of perioperative outcomes and long-term survival. Dis Colon Rectum 2011;54:6-14. [Crossref] [PubMed]
- McKay GD, Morgan MJ, Wong SK, et al. Improved short-term outcomes of laparoscopic vs. open resection for colon and rectal cancer in an area health service: a multicenter study. Dis Colon Rectum 2012;55:42-50. [Crossref] [PubMed]
- Gunka I, Dostalik J, Martinek L, et al. Long-term results of laparoscopic vs. open surgery for nonmetastatic colorectal cancer. Acta Chir Belg 2012;112:139-47. [Crossref] [PubMed]
- Siani LM, Ferranti F, Benedetti M, et al. Laparoscopic vs. open total mesorectal excision for stage I-III mid and low rectal cancer: a retrospective 5 years analysis. G Chir 2012;33:404-8. [PubMed]
- Jefferies MT, Evans MD, Hilton J, et al. Oncological outcome after laparoscopic abdominoperineal excision of the rectum. Colorectal Dis 2012;14:967-71. [Crossref] [PubMed]
- Kellokumpu IH, Kairaluoma MI, Nuorva KP, et al. Short- and long-term outcome following laparoscopic vs. open resection for carcinoma of the rectum in the multimodal setting. Dis Colon Rectum 2012;55:854-63. [Crossref] [PubMed]
- Seshadri RA, Srinivasan A, Tapkire R, et al. Laparoscopic vs. open surgery for rectal cancer after neoadjuvant chemoradiation: a matched case-control study of short-term outcomes. Surg Endosc 2012;26:154-61. [Crossref] [PubMed]
- Kang J, Yoon KJ, Min BS, et al. The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison--open, laparoscopic, and robotic surgery. Ann Surg 2013;257:95-101. [Crossref] [PubMed]
- Lujan J, Valero G, Biondo S, et al. Laparoscopic versus open surgery for rectal cancer: results of a prospective multicentre analysis of 4,970 patients. Surg Endosc 2013;27:295-302. [Crossref] [PubMed]
- Wilson MZ, Hollenbeak CS, Stewart DB. Laparoscopic colectomy is associated with a lower incidence of postoperative complications than open colectomy: a propensity score-matched cohort analysis. Colorectal Dis 2014;16:382-9. [Crossref] [PubMed]
- Moghadamyeghaneh Z, Phelan M, Smith BR, et al. Outcomes of Open, Laparoscopic, and Robotic Abdominoperineal Resections in Patients With Rectal Cancer. Dis Colon Rectum 2015;58:1123-9. [Crossref] [PubMed]
- Midura EF, Hanseman DJ, Hoehn RS, et al. The effect of surgical approach on short-term oncologic outcomes in rectal cancer surgery. Surgery 2015;158:453-9. [Crossref] [PubMed]
- Dural AC, Keskin M, Balik E, et al. The role of the laparoscopy on circumferential resection margin positivity in patients with rectal cancer: long-term outcomes at a single high-volume institution. Surg Laparosc Endosc Percutan Tech 2015;25:129-37. [Crossref] [PubMed]
- Cho MS, Kim CW, Baek SJ, et al. Minimally invasive vs. open total mesorectal excision for rectal cancer: Long-term results from a case-matched study of 633 patients. Surgery 2015;157:1121-9. [Crossref] [PubMed]
- Kim JH, Ahn BK, Park SJ, et al. Long-term Outcomes of Laparoscopic vs. Open Surgery for Rectal Cancer: A Single-center Retrospective Analysis. Korean J Gastroenterol 2015;65:273-82. [Crossref] [PubMed]
- Zaharie F, Ciorogar G, Zaharie R, et al. Laparoscopic rectal resection vs. conventional open approach for rectal cancer - a 4-year experience of a single center. J BUON 2015;20:1447-55. [PubMed]
- de Jesus JP, Valadão M, de Castro Araujo RO, et al. The circumferential resection margins status: A comparison of robotic, laparoscopic and open total mesorectal excision for mid and low rectal cancer. Eur J Surg Oncol 2016;42:808-12. [Crossref] [PubMed]
- Araujo SE. Conventional approach x laparoscopic abdominoperineal resection for rectal cancer treatment after neoadjuvant chemoradiation: results of a prospective randomized trial. Rev Hosp Clin Fac Med Sao Paulo 2003;58:133-40. [Crossref] [PubMed]
- Zhou ZG, Hu M, Li Y, et al. Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 2004;18:1211-5. [Crossref] [PubMed]
- Braga M, Frasson M, Vignali A, et al. Laparoscopic Resection in Rectal Cancer Patients: Outcome and Cost-Benefit Analysis. Dis Colon Rectum 2007;50:464-71. [Crossref] [PubMed]
- Pechlivanides G, Gouvas N, Tsiaoussis J, et al. Lymph node clearance after total mesorectal excision for rectal cancer: laparoscopic vs. open approach. Dig Dis 2007;25:94-9. [Crossref] [PubMed]
- Ng SS, Leung KL, Lee JFY, et al. Laparoscopic-assisted vs. open abdominoperineal resection for low rectal cancer: a prospective randomized trial. Ann Surg Oncol 2008;15:2418-25. [Crossref] [PubMed]
- Lujan J, Valero G, Hernandez Q, et al. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg 2009;96:982-9. [Crossref] [PubMed]
- Liang X, Hou S, Liu H, et al. Effectiveness and safety of laparoscopic resection versus open surgery in patients with rectal cancer: a randomized, controlled trial from China. J Laparoendosc Adv Surg Tech A 2011;21:381-5. [Crossref] [PubMed]
- Ng SS, Lee JF, Yiu RY, et al. Laparoscopic-assisted versus open total mesorectal excision with anal sphincter preservation for mid and low rectal cancer: a prospective, randomized trial. Surg Endosc 2014;28:297-306. [Crossref] [PubMed]
- Fujii S, Ishibe A, Ota M, et al. Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 2014;28:466-76. [Crossref] [PubMed]
- Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional vs. laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718-26. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic vs. open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- Kang SB, Park JW, Jeong SY, et al. Open vs. laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 2010;11:637-45. [Crossref] [PubMed]
- Fleshman J, Branda M, Sargent DJ, et al. Effect of Laparoscopic-Assisted Resection vs Open Resection of Stage II or III Rectal Cancer on Pathologic Outcomes: The ACOSOG Z6051 Randomized Clinical Trial. JAMA 2015;314:1346-55. [Crossref] [PubMed]
- Stevenson AR, Solomon MJ, Lumley JW, et al. Effect of Laparoscopic-Assisted Resection vs Open Resection on Pathological Outcomes in Rectal Cancer: The ALaCaRT Randomized Clinical Trial. JAMA 2015;314:1356-63. [Crossref] [PubMed]
- Aziz O, Constantinides V, Tekkis PP, et al. Laparoscopic vs. open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol 2006;13:413-24. [Crossref] [PubMed]
- Gao F, Cao YF, Chen LS. Meta-analysis of short-term outcomes after laparoscopic resection for rectal cancer. Int J Colorectal Dis 2006;21:652-6. [Crossref] [PubMed]
- Bonjer HJ, Hop WC, Nelson H, et al. Laparoscopically Assisted vs Open Colectomy for Colon Cancer. Arch Surg 2007;142:298-303. [Crossref] [PubMed]
- Anderson C, Uman G, Pigazzi A. Oncologic outcomes of laparoscopic surgery for rectal cancer: A systematic review and meta-analysis of the literature. Eur J Surg Oncol 2008;34:1135-42. [Crossref] [PubMed]
- Gong T, Zhou X, Dou H, et al. A meta-analysis of clinical outcomes after laparoscopic operation for rectal cancer. Zhonghua Wei Chang Wai Ke Za Zhi 2010;13:831-5. [PubMed]
- Ohtani H, Tamamori Y, Azuma T, et al. A meta-analysis of the short- and long-term results of randomized controlled trials that compared laparoscopy-assisted and conventional open surgery for rectal cancer. J Gastrointest Surg 2011;15:1375-85. [Crossref] [PubMed]
- Huang MJ, Liang JL, Wang H, et al. Laparoscopic-assisted versus open surgery for rectal cancer: a meta-analysis of randomized controlled trials on oncologic adequacy of resection and long-term oncologic outcomes. Int J Colorectal Dis 2011;26:415-21. [Crossref] [PubMed]
- Ng SS, Lee JF, Yiu RY, et al. Long-term oncologic outcomes of laparoscopic vs. open surgery for rectal cancer: a pooled analysis of 3 randomized controlled trials. Ann Surg 2014;259:139-47. [Crossref] [PubMed]
- Trastulli S, Cirocchi R, Listorti C, et al. Laparoscopic vs open resection for rectal cancer: a meta-analysis of randomized clinical trials. Colorectal Dis 2012;14:e277-96. [Crossref] [PubMed]
- Arezzo A, Passera R, Scozzari G, et al. Laparoscopy for rectal cancer reduces short-term mortality and morbidity: results of a systematic review and meta-analysis. Surg Endosc 2013;27:1485-502. [Crossref] [PubMed]
- Ahmad NZ, Racheva G, Elmusharaf H. A systematic review and meta-analysis of randomized and non-randomized studies comparing laparoscopic and open abdominoperineal resection for rectal cancer. Colorectal Dis 2013;15:269-77. [Crossref] [PubMed]
- Vennix S, Pelzers L, Bouvy N, et al. Laparoscopic vs. open total mesorectal excision for rectal cancer. In: Breukink S. editor. Cochrane Database of Systematic Reviews. Vol Chichester, UK: John Wiley & Sons, Ltd, 2014.
- Zhang FW, Zhou ZY, Wang HL, et al. Laparoscopic vs. open surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Asian Pac J Cancer Prev 2014;15:9985-96. [Crossref] [PubMed]
- Chen K, Cao G, Chen B, et al. Laparoscopic vs. open surgery for rectal cancer: A meta-analysis of classic randomized controlled trials and high-quality Nonrandomized Studies in the last 5 years. Int J Surg 2017;39:1-10. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Zhang Q, Yang J, Qian Q. Evidence-based treatment of patients with rectal cancer Oncol Lett 2016;11:1631-4. (Review). [PubMed]
- Rickles AS, Dietz DW, Chang GJ, et al. High Rate of Positive Circumferential Resection Margins Following Rectal Cancer Surgery: A Call to Action. Ann Surg 2015;262:891-8. [Crossref] [PubMed]
- Jayne DG, Thorpe HC, Copeland J, et al. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 2010;97:1638-45. [Crossref] [PubMed]
- Green BL, Marshall HC, Collinson F, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 2013;100:75-82. [Crossref] [PubMed]
- Martínez-Pérez A, Carra MC, Brunetti F, et al. Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer. JAMA Surg 2017;152:e165665 [Crossref] [PubMed]
Cite this article as: Milone M, Manigrasso M, Burati M. Rectal cancer—state of art of laparoscopic versus open surgery. Ann Laparosc Endosc Surg 2017;2:147.