Useful modifications to the robotic posterior retroperitoneoscopic approach to adrenalectomy in severely obese patients
Introduction
In 2014, Berber et al. reported the first robotic posterior retroperitoneoscopic adrenalectomy (RPRA) (1). Laparoscopic or RPRA provides an excellent alternative to the adrenal in patients with prior anterior abdominal procedures (2). However, posterior retroperitoneoscopic adrenalectomy (PRA) has potential limitations (1,3-5) including: small working space, straight instruments, copious retroperitoneal adipose tissue, patient’s anatomic characteristics such as a thick or obese back and the surgeon’s lack of familiarity with the retroperitoneal anatomy.
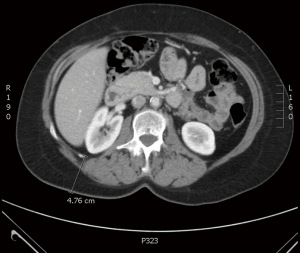
A 12-mm blunt balloon trocar (AutoSuture/Covidien, Mansfield, MA, USA) (Figure 1) has been traditionally used by our group for the camera and has been widely described by others (3,5,6). This blunt balloon trocar is 100 mm in length and underperforms in obese patients and those with thick/deep back wall. The robot arm needs to “snap” into place and utilizes about 1–2 cm of space in the shaft of the port. In many instances, the port is not long enough to dock the robot camera arm and it may become dislodged or it does not hold the pneumoretroperitoneum leading to loss of space and subcutaneous emphysema. In some cases, the balloon can also rupture or pops back into the back muscle wall causing unnecessary delays in the procedure.
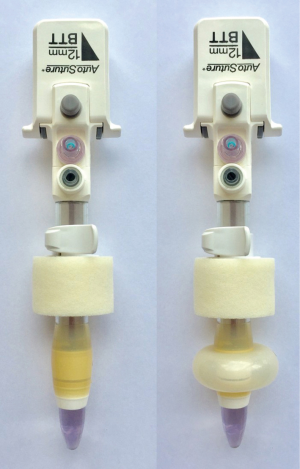
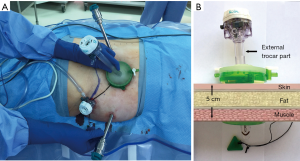
The GelPOINT mini advanced access platform (mini GelPOINT) (Applied Medical, Rancho Santa Margarita, CA) is marketed for single-site laparoscopic surgery (7-11) including transabdominal adrenalectomy (12). GelPOINT comes in three basic sizes with the mini GelPOINT being the smallest (Figure 2A) which includes GelSeal cap, a wound protector/retractor and three low-profile sleeves (Figure 2B). Here we describe a novel use of the GelPOINT mini in RPRA as an alternative to the widely used blunt balloon trocar.

Patient
A 52-year-old female was incidentally found to have a 2 cm right adrenal mass. Her BMI was 36.9 kg/m2. She underwent biochemical evaluation and was found to have a cortisol level of 2.3 after 1 mg overnight dexamethasone suppression and she had an elevated midnight salivary cortisol. She was diagnosed with subclinical Cushing’s syndrome. Her surgical history consisted of an open Roux-en-Y gastric bypass, hysterectomy, C-section, cholecystectomy and multiple abdominal hernia repairs and abdominoplasty. Because of her extensive abdominal surgical history we offered her a RPRA.
Surgical procedure
The patient is positioned prone over a Wilson frame and in jack-knife. Appropriate padding is used and the operative area is prepped and draped.
A 12 mm incision is performed below the tip of 12th rib and the retroperitoneal space is dissected bluntly with the surgeon’s finger. Two 8 mm long robotic trocars are placed, one lateral to the 12th rib port site and one medial about 3 cm below the junction of the 12th rib and the spine. These triangulating trocars are introduced while the surgeon’s finger is inserted at the 12th rib tip port site to receive them and to avoid injury to the kidney and other structures. In this procedure we also add a 5 mm assistant port just lateral and inferior to the tip of the 12th rib port site (Figures 3,4A). A 12-mm blunt balloon trocar (AutoSuture/Covidien, Mansfield, MA, USA) is then placed in the 12th rib access site. The retroperitoneal space is then insufflated with CO2 and the pressure is maintained at 20 mmHg. The laparoscope 30-degree camera is introduced looking up and with the help of a grasper via the lateral 5 mm port site; the loose areolar tissue behind Geroda’s is taken down with care not to injure the lateral peritoneal lining (over liver for this right sided lesion).
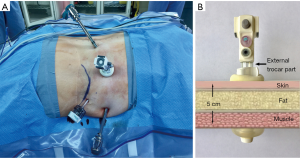
Once the medial musculature and the lateral peritoneal layer have been clearly identified (6) the da Vinci robot is docked (Intuitive Surgical, Sunnyvale, CA, USA). The robotic camera arm could not be docked on the 10–12 mm blunt balloon trocar because it was too short due to the thickness of the back wall (Figures 3,4A,4B).
A mini GelPort was introduced instead using the 12 mm port site. A 10–12 mm extra-long trocar (Ethicon Endo-Surgery, Guaynabo, Puerto Rico, USA) was then inserted through the gel port for the robotic camera (Figure 5A,B). Once this was achieved, the 8 mm robotic cardiere forceps were used on the left sided and the 8 mm robotic cautery hook was used in the right-sided port. The 30-degree camera was then introduced looking down and dissection is carried from lateral to medial removing all the tissue above the kidney. The kidney is retracted caudad by the assistant. The right adrenal vein is dissected, clipped with 5 mm Hem-o-lok clips (Teleflex Medical, Morrisville, NC, USA) and then divided by the first assistant through the assistant port. The entire adrenal gland is then placed in an Endopouch retriever (Ethicon Endo-surgery, Cincinnati, OH, USA) and removed via the mini GelPOINT site. After making sure the area is hemostatic, the CO2 is removed and the camera port site closed at the fascia level. All other port sites are closed at the skin level.
Results
Total operation time was 95 minutes, docking and console times were 20 and 75 minutes and blood loss was minimal. Final pathology was consistent with a 2.2 cm cortical adenoma. The gland weighed 16.3 g. The patient was discharged after one night stay in the hospital and there were no complications.
Discussion
The PRA is a safe and effective minimally invasive technique that avoids the abdominal cavity in patients who have had extensive abdominal procedures (2). Robotic technology can potentially improve some of the limitations of the laparoscopic PRA (1).
A 12-mm blunt balloon trocar (AutoSuture/Covidien, Mansfield, MA, USA) (Figure 1) was used in RPRA for the robotic camera, and has been described by prior investigators (3,5,6). This blunt balloon trocar is only 100 mm in length and often not long enough to dock the robotic camera arm particularly in severely obese patients or those with thick/deep back wall. The blunt balloon trocar is recommended for the retroperitoneal approach to adrenalectomy because the balloon allows retention of the pneumoretroperitoneum, which is held at higher pressures (20–30 mmHg) than during transabdominal approaches. In severely obese patients or in those with thick or deep back walls the balloon trocar falls short and may “pop” out of position failing to sustain the required retroperitoneal pressures. This happens more often when the robot technique is being used because the camera arm of the robot requires approximate 2 cm of docking space and the trocar may not be long enough to achieve this (Figures 3,4B). In some of our severely obese patients (BMI >35 kg/m2), the thickness of the back wall can be >45 to 50 mm and the balloon has ruptured or popped back into the back muscle wall leading to unnecessary delays in the procedure as well as increased subcutaneous air due to poor seal.
Since 2010, the mini GelPOINT has been used for single-site laparoscopic cholecystectomy (7), colectomy (8), gastrectomy (9), nephrectomy (10,11) and trans-abdominal adrenalectomy (12). The mini GelPOINT platform includes GelSeal cap, a wound protector/retractor and three low-profile sleeves (Figure 2B) and can be used in small incisions 1.5 to 3 cm in size. The GelSeal Cap offers a pseudo abdomen platform for triangulation of standard laparoscopic instrumentation and provides a flexible fulcrum for easy instrument articulation and movement. The Alexis wound protector/retractor offers atraumatic retraction and specimen retrieval as well as wound protection.
Because the blunt balloon trocar did not hold well in our severely obese patient, we switched to the mini GelPOINT with its GelSeal Cap and wound protector (Figure 5B). Because the 10–12 mm long trocar was inserted through the GelSeal Cap, this long camera trocar was used alone through the GelCap with the other two long robotic trocars at different sites to effectively allow robotic docking and minimize external robotic arm collisions (6). We observed no air leak around the camera trocar site during the procedure. The mini GelPOINT port never became dislodged and allowed us to easily manipulate the camera without issue.
In our previous laparoscopic and RPRA cases, we observed minor subcutaneous emphysema. This has been previously described and is an expected observation in RPAs, particularly as procedure time and insufflation pressure increases (13). During and after the described case, the patient had no subcutaneous emphysema. We believe that the wound protector of the mini GelPOINT provides a very effective seal through the back wall around the camera port site and effectively prevents air leaking and infiltrating the subcutaneous tissues. This may be useful to the surgeon when he or she expects a longer procedure time.
Conclusions
In this case study, the mini GelPOINT appeared to be a feasible, safe and effective alternative for RPRA procedures in severely obese patients. Its use helped prevent dislodging of the camera port, loss of retroperitoneal pressure and the accumulation of subcutaneous emphysema.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.08.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Berber E, Mitchell J, Milas M, et al. Robotic posterior retroperitoneal adrenalectomy: operative technique. Arch Surg 2010;145:781-4. [Crossref] [PubMed]
- Walz MK, Alesina PF, Wenger FA, et al. Posterior retroperitoneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 2006;140:943-8; discussion 948-50. [Crossref] [PubMed]
- Dickson PV, Alex GC, Grubbs EG, et al. Robotic-assisted retroperitoneoscopic adrenalectomy: making a good procedure even better. Am Surg 2013;79:84-9. [PubMed]
- Karabulut K, Agcaoglu O, Aliyev S, et al. Comparison of intraoperative time use and perioperative outcomes for robotic versus laparoscopic adrenalectomy. Surgery 2012;151:537-42. [Crossref] [PubMed]
- Ludwig AT, Wagner KR, Lowry PS, et al. Robot-assisted posterior retroperitoneoscopic adrenalectomy. J Endourol 2010;24:1307-14. [Crossref] [PubMed]
- Feng Z, Feng MP, Levine JW, et al. Robotic retroperitoneoscopic adrenalectomy: useful modifications of the described posterior approach. J Robot Surg 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Petrotos AC, Molinelli BM. Single-incision multiport laparoendoscopic (SIMPLE) surgery: early evaluation of SIMPLE cholecystectomy in a community setting. Surg Endosc 2009;23:2631-4. [Crossref] [PubMed]
- Ramos-Valadez DI, Patel CB, Ragupathi M, et al. Single-incision laparoscopic colectomy: outcomes of an emerging minimally invasive technique. Int J Colorectal Dis 2011;26:761-7. [Crossref] [PubMed]
- Farías C, Fernández JI, Ovalle C, et al. Transumbilical sleeve gastrectomy with an accessory lateral port: surgical results in 237 patients and 1-year follow-up. Obes Surg 2013;23:325-31. [Crossref] [PubMed]
- Featherstone NC, De Win G, Undre S, et al. Single incision prone retroperitoneoscopic paediatric nephrectomy. J Pediatr Urol 2015;11:283-4. [Crossref] [PubMed]
- Gimenez E, Leeser DB, Wysock JS, et al. Laparoendoscopic single site live donor nephrectomy: initial experience. J Urol 2010;184:2049-53. [Crossref] [PubMed]
- Sasaki A, Nitta H, Otsuka K, et al. Laparoendoscopic single site adrenalectomy: initial results of cosmetic satisfaction and the potential for postoperative pain reduction. BMC Urol 2013;13:21. [Crossref] [PubMed]
- Mercan S, Seven R, Ozarmagan S, et al. Endoscopic retroperitoneal adrenalectomy. Surgery 1995;118:1071-5; discussion 1075-6. [Crossref] [PubMed]
Cite this article as: Feng Z, Feng DP, Solórzano CC. Useful modifications to the robotic posterior retroperitoneoscopic approach to adrenalectomy in severely obese patients. Ann Laparosc Endosc Surg 2017;2:145.