Single-access laparoscopic rectal resection: up-to-down and down-to-up
Introduction
Single-access laparoscopy (SAL) took interest in the last decade (1), due to the attraction to perform minimally invasive surgery (MIS) through the natural orifices (2). The main scope was to add enhanced cosmetic outcomes to the general benefits of MIS. The umbilicus, since its embriological scar, has been considered as the main single-access to perform SAL (3). On the other way, in front a large specimen’s removal or a temporary stoma’s placement, other abdominal sites have been considered, like the suprapubic (4-6) and the right flank (7) accesses.
SAL for rectal resection has been described as feasible and safe (8). It makes sense because it permits to reduce the abdominal wall trauma due to the less number of the trocars, and also to place the temporary stoma at the site of single-access, maintaining improved the cosmetic outcomes. Obviously the patients’ selection is mandatory and, especially at the begining of the surgeon’s experience, low body mass index and female patients are the favorite candidates for this technique.
Moreover, thanks to the natural orifices translumenal endoscopic surgery (NOTES) (9), the application of laparoscopy through the anus took interest in these last years. This approach was already introduced in 1985 by Buess et al. (10) with the transanal endoscopic microsurgery (TEM), and recently it underwent to an evolution with the application of laparoscopy to the surgery of the rectal diseases. Hence, different transanal procedures have been described like the resection of large rectal polyps (11), the total mesorectal excision (TME) (12), and the control of colorectal complications like bleeding, leak and stenosis (13-15). The major benefits of the transanal approach are the exact intraluminal lesion location and the transmural dissection just below, the improved operative field’s exposure, the better exposure of the lateral nerves, the specimen’s removal through the anus with a reduced incisional hernia rate, and the improved surgeon’s ergonomics.
The union between the abdominal SAL and the transanal TME (TaTME) makes sense because the vascular dissection and the colic mobilization can be performed through the SAL, the TME can be realized through the transanal route, and the abdominal access-site can be used for the temporary ileostomy placement at the end of the procedure.
In front of a rectal tumor, the rectal TME is chosen between the only abdominal access (7), the abdominal access plus the transanal access (16), and the pure transanal access (17). The decision is taken considering the tumor’s location, the patient’s characteristics, the surgeon’s familiarity with these techniques. For the cancer of the middle and low rectum, the transanal approach alone or associated to the abdominal access can probably add more benefits. For the cancer of the upper rectum, the abdominal approach alone probably remains the favorite. Anyway so far, proper guidelines have to be still written.
In this chapter, the rectal resection with TME through abdominal SAL or abdominal SAL plus TaTME, is described in details.
Techniques
Up-to-down rectal resection
Patient and team positioning
The patient is placed in a supine position, with the arms alongside the body and the legs apart. The arms, ankles, and legs are secured and protected. These latter are well secured to the operative table, and the left leg is positioned further up.
For the first part of the procedure, the surgeon stands to the patient’s right and the camera assistant to the surgeon’s right. The scrub-nurse stands between the patient’s legs. The video monitor is placed in front of the surgeon and camera assistant.
After the mesocolic mobilization is made, the camera assistant moves to the surgeon’s left, and the scrub-nurse to the surgeon’s right.
Single-access abdominal laparoscopy
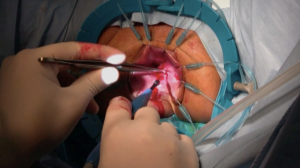
A 3.5-cm transverse skin incision is made in the right flank, adjacent to the right rectus abdominis muscle and between the umbilicus and the superior right iliac spine. The underlying fascia is divided in a pararectal fashion for 1.5 cm, which exposes the rectus abdominis muscle. The muscle is medially retracted and a purse-string suture using PDS 1 is placed in the fascia, going inside and outside respectively at the 5, 7, 9, 11, 1, and 3 o’clock positions. The peritoneal sheet is entered through a 1-cm vertical incision, and a new purse-string suture using Vicryl 1 is placed, going inside and outside respectively at the 5, 7, 9, 11, 1, and 3 o’clock positions. Both sutures are kept externally with a Pean-Rochester curved forceps.
An 11-mm reusable trocar (or a 12-mm non-reusable trocar) is introduced into the peritoneal cavity inside the purse-string sutures, and the pneumoperitoneum is created. The 10-mm, 30º scope is advanced through the 11-mm trocar.
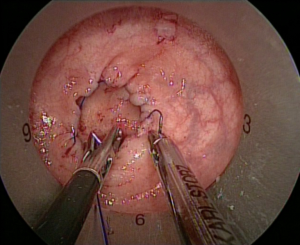
A 6-mm reusable flexible trocar is inserted at 12 o’clock position with the respect to the patient’s head, outside the purse-string sutures and on the same vertical line of the previous trocar, for the insertion of the curved reusable instruments according to DAPRI (Karl Storz-Endoskope, Tuttlingen, Germany) (Figure 1). The first one is the bicurved grasping forceps (Figure 1A), inserted following its curves at 45º with respect to the abdominal wall (Figure 2).
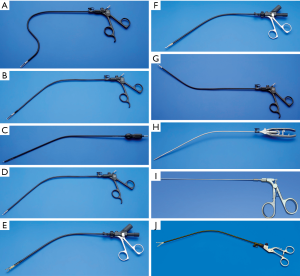

Another 6-mm reusable flexible trocar is inserted at the 6 o’clock position with the respect to the patient’s head, outside the purse-string sutures and on the same vertical line of the previous trocars, for insertion of other instruments (Figure 3), such as the monocurved grasping forceps (Figure 1B), the monocurved coagulating hook (Figure 1C), the monocurved dissecting forceps (Figure 1D), the monocurved bipolar forceps (Figure 1E) and scissors (Figure 1F), the straight 5-mm clip applier, the monocurved scissors (Figure 1G), the monocurved needle holder (Figure 1H), the suction and irrigation cannula, and the straight grasping forceps.

The abdominal cavity is explored and examined to rule out the presence of peritoneal metastases, superficial hepatic lesions and free ascites.
The operative room table is placed in an accentuated Trendelenburg position with right-sided tilt.
The small bowel is moved into the right abdominal quadrants and above the right liver lobe using the bicurved and the monocurved grasping forceps.
The ligament of Treitz is identified in order to expose the root of the inferior mesenteric vein. The peritoneal sheet at the root of this vein is incised with the monocurved coagulating hook (Figure 4) until the Toldt’s fascia is reached. The inferior mesenteric vein is isolated using the monocurved dissecting forceps and clipped by the 5-mm straight clip applier. The left mesocolon is separated from the Toldt’s fascia in an avascular plane using the monocurved coagulating hook or the suction cannula (Figure 5).
Surgeon works with curved instruments without crossed hands and without conflict with the camera assistant’s hand (Figure 6).
The peritoneal sheet is incised along the abdominal aorta with the monocurved coagulating hook, reaching the origin of the inferior mesenteric artery (Figure 7). The root of the artery is freed using the monocurved coagulating hook and the monocurved dissecting forceps, clipped by the 5-mm straight clip applier, and divided by the monocurved scissors (Figure 8).
If necessary to improve the operative field’s exposure, a straight 1.8-mm trocarless grasping forceps (Figure 1I) can be inserted percutaneously via a skin puncture (created by a Veress needle) in the left suprapubic area. At the end of the procedure, this hole can be used for drain placement.
The left mesocolon is freed from the Toldt’s fascia (Figure 9), respecting the left Gerota’s fascia and going in the direction of the pancreatic tail. The sigmoid and left colon are mobilized from the peritoneal attachments, using the monocurved coagulating hook or scissors (Figure 10), until to reach the splenic flexure, which is mobilized by a medial-to-lateral approach.

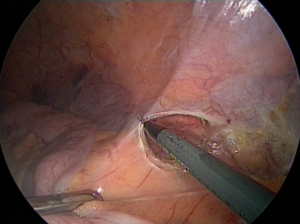
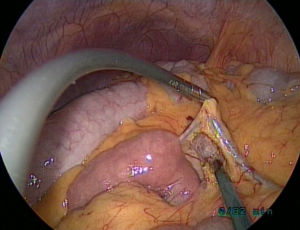
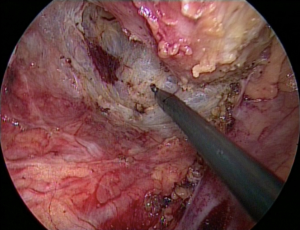
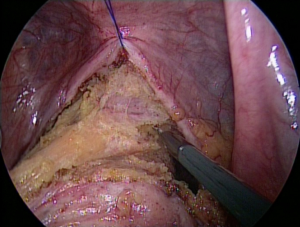
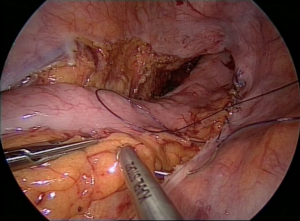
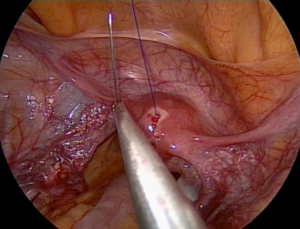
The procedure is continued with the mobilization of the left mesocolon until the promontory is reached. The upper mesorectum is incised and dissected from the presacral fascia in an avascular plane (Figure 11), using the monocurved coagulating hook, and the monocurved bipolar grasping forceps and scissors.
For the rest of the TME, the camera assistant moves to the surgeon’s left, and the scrub-nurse to the surgeon’s right. The TME is performed from up-to-down, alternatively using the monocurved coagulating hook and the monocurved bipolar grasping forceps and scissors.
To improve the pelvic field’s exposure, one or two temporary percutaneous suture using a straight Ethilon 2/0 needle, is passed from the suprapubic area into the uterine fundus (female) (Figure 12). Moreover, for the recto-sigmoid colon resection, if the straight 1.8-mm trocarless grasping forceps is already inserted it can be used, otherwise another straight Ethilon 2/0 needle is passed in the pericolic fatty tissue and kept externally by a Pean-Rochester curved forceps.
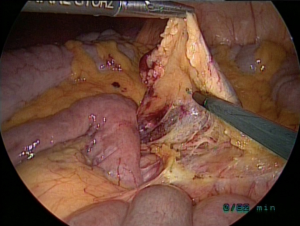
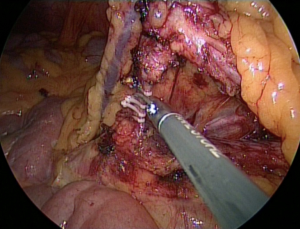
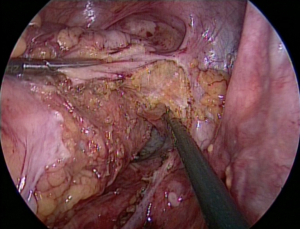
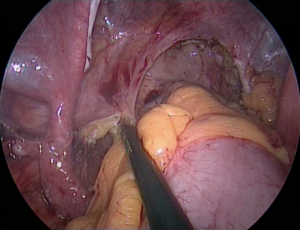
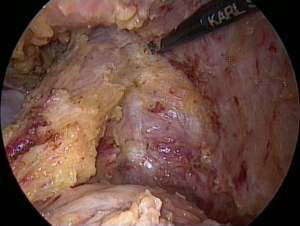
Once the upper mesorectum is freed, the dissection continues with the mobilization of the middle and low mesorectum, going first posteriorly (Figure 13), then laterally (Figures 14,15), and finally anteriorly (Figure 16), using both coagulating hook and bipolar instruments. At this step in both male and female patient, a temporary suprapubic percutaneous suture (straight Ethilon 2/0 needle) is passed into the pelvic peritoneal reflexion (Figure 17). The plane anteriorly to the rectum and posteriorly to the seminal vesicles/rectoprostatic fascia (male) or uterin cervix/vagina (female) (Figure 18) is dissected with the monocurved coagulating hook.
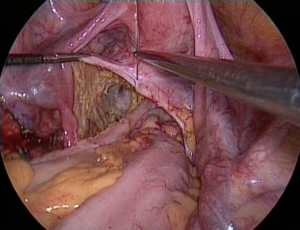
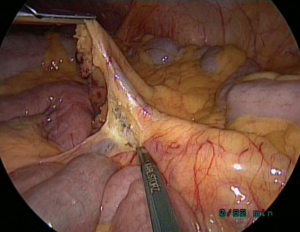
Once the lower mesorectum is reached, the dissection continues first posteriorly to reach both the levator ani muscles, and then laterally and anteriorly (Figure 19). Monocurved bipolar grasping forceps and scissors are contineously used and changed during this step.
The level of the left colon transection is chosen, and the mesocolon is dissected from this level going in the direction of the inferior mesenteric vein root, using the monocurved coagulating hook and bipolar tools.
For the rectal sectioning, the 11-mm trocar is replaced by a reusable 13-mm trocar (if the 12-mm non-reusable trocar is inserted at the beginning, this replacement is not needed), in order to accomodate an articulating linear stapler. The 10-mm scope is switched into a 5-mm, 30º long scope, which is inserted into the 6-mm flexible trocar at the 6 o’clock position (Figure 20). The linear stapler encircles the freed low rectum and is fired (Figure 21). Usually two-three firings are enough to complete the rectal section.
The specimen is held by the straight grasping forceps and the 6-mm flexible trocar at the 6 o’clock position is retrieved together with the 13-mm trocar and both purse-string sutures. The two fascial openings for the trocars are joined together, enlarging the access. A plastic wall protector is inserted into the peritoneal cavity. The specimen is removed inside the plastic protector (Figure 22). The correct level of the left colon transection is found and sectioned by scissors. The anvil of circular stapler is inserted into the lumen, and a Prolene 2/0 purse-string suture is used to close the colic lumen aorund the anvil spike.
The anvil is introduced into the abdominal cavity, and the peritoneal sheet as well as the muscular fascia, are partially closed by Vicryl 1 sutures, permitting introduction of the 11-mm trocar into the abdominal cavity. The 10-mm scope is reused.
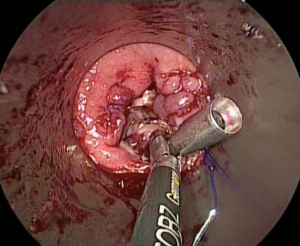
The circular stapler is introduced through the anus into the rectum, and the stapler spike is pushed out the rectal stump, staying in the middle of the previous staple line. The bicurved grasper is used to fit the anvil into the circular stapler; the stapler is closed and fired (Figure 23).
The suction and irrigation cannula is introduced and the pelvis is immersed under physiologic solution. Leak-test of the anastomosis, using insufflated air through the anus, is performed.
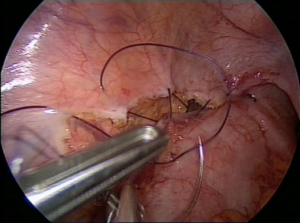
The temporary percutaneous sutures are removed. The parietal pelvic peritoneum is closed and attached to the left colon by Vicryl 2/0 running sutures (Figures 24,25), using the monocurved needle holder and the bicurved grasping forceps. The left mesocolic window is closed as well by a Vicryl 2/0 running suture. If necessary, a suprapubic drain is placed into the pelvis.
The operative room table is positioned without any Trendelenburg and tilt, and the small bowel is gently moved out of the right abdominal quadrants and over the left colon.
The distal bowel loop as well as the ileo-caecal valve are searched. A loop, roughly 20 cm before the ileo-caecal valve, is grasped and extracted at the level of the abdominal access, together with the trocars’ removal. A temporary ileostomy is realized, placing the ileum outside the access (Figure 26), and closing the fascia and the peritoneal sheet by Vicryl 1 sutures. The ileum is open, and muco-cutaneous sutures using Vicryl Rapid 3/0 are positioned. An ileostomy set is finally placed.
Post-operative care
One gram paracetamol is given i.v. at the end of the surgical procedure. Postoperative analgesia is given following the WHO visual analog pain scale (VAS). In the recovery room, the following scheme is followed: for VAS between 1 and 3, 1 g paracetamol i.v. is administered; for VAS between 4 and 8, 100 mg tramadol i.v. is used; for VAS greater than 8, 1 mg piritamide i.v. is incremented.
The arterial catheter is removed in the recovery room.
Once the patient leaves the recovery room, pain is assessed every 6 h, with 1 g paracetamol administered i.v. if VAS is between 1 and 3, and 100 mg tramadol administered i.v. if VAS is between 4 and 8.
Antibiotic prophylaxis is prescribed if necessary and TVP prophylaxis until the discharge of the patient from the hospital. The urinary catheter is removed after 5 days. The patient is allowed to drink water after 24 hours, and to tolerate a light diet from the 3rd postoperative day. The management of the ileostomy is started after 48 hours. If there are no complications, the patient is discharged on the 6th postoperative day, after the abdominal drain (if used) and central line have been removed.
Upon discharge, 1 g paracetamol perorally or 50 mg tramadol perorally are prescribed only if needed.
Office visits are scheduled at 10 days, 1 and 2 months. Usually the patient is scheduled for the closure of the temporary ileostomy after 2 months. Then, the patient is followed-up by the surgeon and the gastroenterologist/oncologist.
Down-to-up rectal resection
Patient and team positioning
The patient is placed in a supine position, with the arms alongside the body and the legs apart. The arms, ankles, and legs are secured and protected. These latter are well secured to the operative table, and the left leg is positioned further up.
For the first part of the procedure, the surgeon stands to the patient’s right and the camera assistant to the surgeon’s right. The scrub-nurse stands between the patient’s legs. The video monitor is placed in front of the surgeon and camera assistant.
After the mesocolic mobilization is made, the camera assistant moves to the surgeon’s left, and the scrub-nurse to the surgeon’s right.
During the perineal resection, the surgeon stands between the patient’s legs, the camera assistant to the surgeon’s right and the scrub-nurse to the surgeon’s left. The video monitor is placed in front of the surgeon and camera assistant.
Single-access abdominal laparoscopy
A 3.5-cm transverse skin incision is made in the right flank, adjacent to the right rectus abdominis muscle and between the umbilicus and the superior right iliac spine. The underlying fascia is divided in a pararectal fashion for 1.5 cm, which exposes the rectus abdominis muscle. The muscle is medially retracted and a purse-string suture using PDS 1 is placed in the fascia, going inside and outside respectively at the 5, 7, 9, 11, 1, and 3 o’clock positions. The peritoneal sheet is entered through a 1 cm vertical incision, and a new purse-string suture using Vicryl 1 is placed, going inside and outside respectively at the 5, 7, 9, 11, 1, and 3 o’clock positions. Both sutures are kept externally with Pean-Rochester curved graspers.
An 11-mm trocar is inserted into the peritoneal cavity inside the purse-string sutures, and the pneumoperitoneum is created. The 10-mm, 30° scope is advanced through the 11-mm trocar.
A 6-mm reusable flexible trocar is inserted at the 12 o’clock position with respect to the patient’s head, outside the purse-string sutures and on the same vertical line as the previous trocar, for insertion of the bicurved grasping forceps (Figure 1A). This grasping forceps is inserted following its curves at 45° with respect to the abdominal wall (Figure 2).
Another 6-mm reusable flexible trocar is inserted at the 6 o’clock position with respect to the patient’s head, outside the purse-string sutures and on the same vertical line as the previous trocars, for the insertion of other instruments (Figure 3), such as the monocurved grasping forceps (Figure 1B), the monocurved coagulating hook (Figure 1C), the monocurved dissecting forceps (Figure 1D), the monocurved bipolar forceps (Figure 1E) and scissors (Figure 1F), the straight 5-mm clip applier, the monocurved scissors (Figure 1G), the monocurved needle-holder (Figure 1H), the suction and irrigation cannula, and the straight grasping forceps.
The abdominal cavity is explored and examined to rule out the presence of peritoneal metastases, superficial hepatic lesions and free ascites.
The operating room table is placed in an accentuated Trendelenburg position with right-sided tilt.
The small bowel is moved into the right abdominal quadrants and above the right liver lobe using the bicurved and monocurved grasping forceps.
The ligament of Treitz is identified in order to expose the root of the inferior mesenteric vein. The peritoneal sheet at the root of this vein is incised with the monocurved coagulating hook (Figure 4) until the Toldt’s fascia is reached. The inferior mesenteric vein is isolated using the monocurved dissecting forceps and clipped by the 5-mm straight clip applier. The left mesocolon is separated from the Toldt’s fascia in an avascular plane using the monocurved coagulating hook or the suction cannula (Figure 5).
The surgeon works with curved instruments without crossing hands and without interference with the camera assistant’s hand (Figure 6).
The peritoneal sheet is incised along the abdominal aorta using the monocurved coagulating hook (Figure 7), until the origin of the inferior mesenteric artery is reached. The root of the artery is freed using the monocurved coagulating hook and the monocurved dissecting forceps, clipped by the 5-mm straight clip applier, and divided using the monocurved scissors (Figure 8).
If necessary to improve the operative field’s exposure, a straight 1.8-mm trocarless grasping forceps (Figure 1I) can be inserted percutaneously via a skin puncture (created by a Veress needle) in the left suprapubic area. At the end of the procedure, this hole can be used for drain placement.
The left mesocolon is freed from the Toldt’s fascia (Figure 9), respecting the left Gerota’s fascia and going in the direction of the pancreatic tail. The sigmoid and left colons are moved away from the peritoneal attachments (Figure 10) using the monocurved coagulating hook or scissors until reaching the splenic flexure, which is downloaded using a medial-to-lateral approach.
The procedure is continued by moving the left mesocolon until the promontory is reached. The upper mesorectum is incised and dissected from the presacral fascia in an avascular plane until 1 cm down the promontory (Figure 27), using the monocurved coagulating hook and the monocurved bipolar grasping forceps and scissors. The level of the left colon transection is chosen and the mesocolon is dissected from this level going in the direction of the inferior mesenteric vein root, using the monocurved coagulating hook and bipolar tools.
In female patients, a temporary percutaneous suture, using a straight Ethilon 2/0 needle, is placed in the uterine fundus to improve the operative field’s exposure (Figure 12).
The procedure continues with the TME performed from down-to-up. The operating room table is placed in a reduced Trendelenburg position and reduced right-sided tilt.
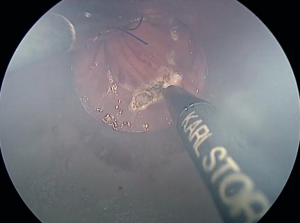
Transanal dissection, specimen’s extraction & colorectal anastomosis
Both patient’s legs are positioned upwards (gynecologic positioning). The D-port (Figure 28) is inserted into the anal canal and fixed to the skin by four silk 0 sutures. A 10-mm, 30° scope is inserted in the middle opening of the D-port (Figure 29), and the rectal lumen is checked to identify the rectal tumor. A gauze pad is pushed beyond the rectal tumor. The monocurved grasping forceps (Figure 1A) and the monocurved anvil grasping forceps (Figure 1J) are inserted at the 9 o’clock opening of the D-port (Figure 30). The other instruments, such as the straight grasping forceps, the monocurved needle-holder (Figure 1H), the monocurved scissors (Figure 1G), the monocurved coagulating hook (Figure 1C), the monocurved bipolar forceps and scissors (Figure 1E,F), the suction and irrigation cannula, are inserted at the 3 o’clock opening of the D-port (Figure 31).




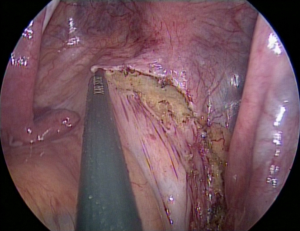
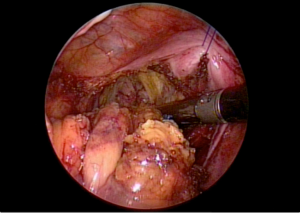
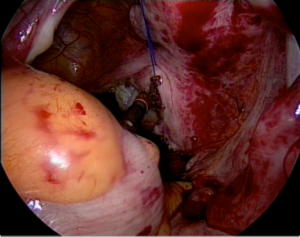
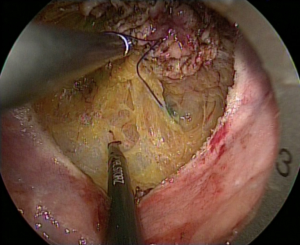
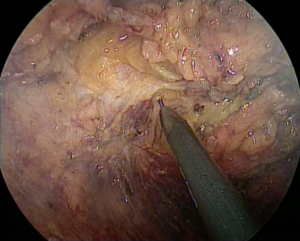
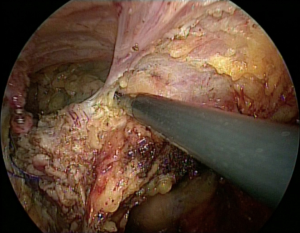
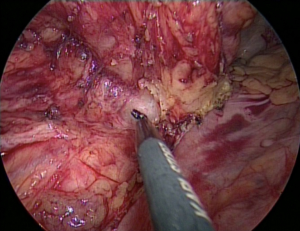
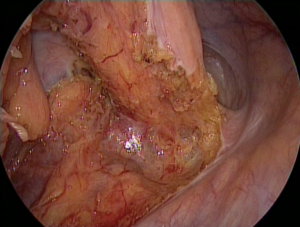
A safe margin distally from the tumor is chosen, and a purse-string suture using Prolene 2/0 is placed into the rectal mucosa, using the monocurved grasping forceps and the monocurved needle holder (Figure 32). The suture is tight extracorporeally, the knot is pushed intraluminally and cut by the monocurved scissors. Then, the mucosa just under the purse-string suture is incised until to pass the entire rectal wall (Figure 33). The TME is performed from bottom to top, going first posteriorly (Figure 34). Then, the mobilization of the rectum is completed, going laterally on the left (of the patient) (Figure 35) and right side (of the patient) (Figure 36). The dissection is finally performed anteriorly, taking care to dissect the correct plane between the rectum and the prostate (male), or the vagina (female) (Figure 37). The dissection is continued up, respecting the presacral fascia posteriorly, until reaching the seminal vesicles (male) or the uterin cervix (female) anteriorly, using both monocurved coagulating hook and monocurved bipolar scissors. Finally, the transanal dissection joins the previous dissection started at the level of the promontory through the laparoscopic abdominal access, opening the Douglas’ pouch (Figure 38).

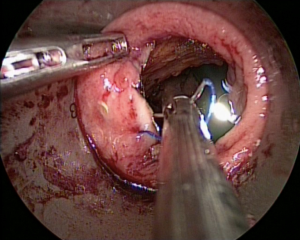
The rectal-sigmoid colon is encircled by a plastic protector and removed transanally, after having removed the D-port (Figure 39). The level of the colic transection is found, the left colon is sectioned, and the specimen removed. The anvil of the circular stapler is introduced into the colic lumen, closing this latter with a Prolene 2/0 purse-string suture. The colon and anvil are pushed inside the pelvis and the D-port is repositioned. The rectal stump is closed transanally with a Prolene 2/0 purse-string suture, using the monocurved grasping forceps and the monocurved needle-holder (Figure 40). Then, the monocurved anvil grasping forceps keeps the anvil transanally (Figure 41), while the suture is tight by extracorporeal knot, pushed intraluminally and cut by the monocurved scissors. The D-port is removed again, and the circular stapler is introduced transanally (Figure 42). The anvil is attached to the circular stapler by the monocurved anvil grasping forceps, under abdominal laparoscopic control. The stapler is closed and fired.
Through the abdomen, the suction and irrigation cannula is introduced and the pelvis is immersed under physiologic solution. A leak-test of the anastomosis, using insufflated air through the anus, is performed.
Transanal dissection, specimen’s extraction and coloanal anastomosis
Both patient’s legs are positioned upwards (gynecologic positioning). A gauze pad is inserted in the anal canal to avoid potential fecal contamination. The anal retractor is positioned and the anal mucosa is injected with Lidocaine 1%. The pectineal line is incised using the monopolar electrode (Figure 43). Once freed circumferentially, the anal mucosa is closed by a silk 0 purse-string suture. The anal canal is dissected until to reach the low rectum into the pelvis.
The D-port is inserted and fixed to the skin by four silk 0 sutures. A 10-mm, 30º scope is inserted in the middle opening of the D-port (similar to Figure 29). The monocurved grasping forceps (Figure 1B) is inserted at the 9 o’clock opening of the D-port (similar to Figure 30). The other instruments, such as the monocurved coagulating hook (Figure 1C), the monocurved bipolar forceps and scissors (Figure 1E,F), the suction and irrigation cannula are inserted at the 3 o’clock opening of the D-port (similar to Figure 31).
The lower rectum is mobilized circumferentially from down-to-up, going first posteriorly (similar to Figure 34), to the left side (of the patient) (similar to Figure 35), to the right side (of the patient) (similar to Figure 36) and, finally anteriorly (similar to Figure 37), using the monocurved coagulating hook and the monocurved grasping forceps. The dissection is performed anteriorly finding the correct plane between the rectum and the prostate (male), or the vagina (female).
The middle rectum is freed, taking care to respect the presacral fascia posteriorly, and to find the correct plane between the rectum and the seminal vesicles (male), or uterin cervix (female) anteriorly. Both the monocurved coagulating hook and the monocurved bipolar scissors are used. Finally, the transanal dissection joins the previous dissection started at the level of the promontory through the laparoscopic abdominal access, opening the Douglas’ pouch (similar to Figure 38).
The rectal-sigmoid colon is encircled by a plastic protector and removed transanally, after having removed the D-port (similar to Figure 39). The level of the colic transection is found and the left colon is sectioned, removing the specimen. A coloanal anastomosis is created using Vicryl Rapid 3/0 sutures (Figure 44). The anal retractor is taken out.
End of both procedures and temporary ileostomy
Through the abdomen, the pelvic parietal peritoneum is closed and attached to the left colon by Vicryl 2/0 running sutures (Figures 24,25), using the monocurved needle holder and the bicurved grasping forceps. Then, the temporary percutaneous suture (female) is removed. The left mesocolic window is closed as well by a Vicryl 2/0 running suture. If necessary, a suprapubic drain is placed into the pelvis.
The operating room table is positioned without any Trendelenburg and tilt, and the small bowel is gently moved out of the right abdominal quadrants and over the left colon.
The distal bowel loop together with the ileo-caecal valve are searched. A loop, roughly 20 cm before the ileo-caecal valve, is grasped and extracted at the level of the abdominal access, together with the trocars’ removal and purse-string sutures. A temporary ileostomy is performed, placing the ileum outside the access (Figure 26), and closing the fascia and the peritoneal sheet by Vicryl 1 sutures. The ileum is open, and muco-cutaneous sutures using Vicryl Rapid 3/0 are positioned. An ileostomy set is finally placed.
Post-operative care
One gram paracetamol is given i.v. at the end of the surgical procedure. Post-operative analgesia is given following the WHO visual analog pain scale (VAS). In the recovery room, the following scheme is followed: for VAS between 1 and 3, 1 g paracetamol i.v. is administered; for VAS between 4 and 8, 100 mg tramadol i.v. is used; for VAS greater than 8, 1 mg piritamide i.v. is incremented.
The arterial catheter is removed in the recovery room.
Once the patient leaves the recovery room, pain is assessed every 6 h, with 1 g paracetamol administered i.v. if VAS is between 1 and 3, and 100 mg tramadol administered i.v. if VAS is between 4 and 8.
Antibiotic prophylaxis is prescribed if necessary and TVP prophylaxis until the discharge of the patient from the hospital. The urinary catheter is removed after 5 days. The patient is allowed to drink water after 24 hours, and to tolerate a light diet from the 3rd post-operative day. The management of the ileostomy is started after 48 hours. If there are no complications, the patient is discharged on the 6th post-operative day, after having removed the abdominal drain (if used) and the central line.
Upon discharge, 1 g paracetamol perorally or 50 mg tramadol perorally are prescribed only if needed.
Office visits are scheduled at 10 days, and 1, 2 months. Usually the patient is scheduled for closure of temporary ileostomy after 2 months. Then, the patient is followed-up by the surgeon and gastroenterologist/oncologist.
Conclusions
SAL rectal resection with TME can be performed with safety, although the patients’ selection and the surgeon’s experience remain mandatory. For the middle and low rectal cancer, SAL has to be joined to the transanal approach, getting the other benefits.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Marco Milone) for the series “Minimally Invasive Treatment of Low Rectal Cancer” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.06.05). The series “Minimally Invasive Treatment of Low Rectal Cancer” was commissioned by the editorial office without any funding or sponsorship. GD serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Aug 2016 to Jul 2018 and consultant for Karl Storz- Endoskope, Tuttlingen, Germany. The author has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed Consent: Written informed consent was obtained from the patients for publication of this article and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dapri G. Single-incision laparoscopy: a review of the indications, techniques and results after more than 700 procedures. Asian J Endosc Surg 2014;7:102-16. [Crossref] [PubMed]
- Mathias JM. NOTES: a new way of performing surgery using natural body orifices. OR Manager 2007;23:12-3. [PubMed]
- Canes D, Desai MM, Aron M, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol 2008;54:1020-9. [Crossref] [PubMed]
- Dapri G, Carandina S, Mathonet P, et al. Suprapubic single-incision laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Innov 2013;20:484-92. [Crossref] [PubMed]
- Dapri G. Suprapubic single-incision laparoscopic left hemicolectomy: an alternative non-visible scar. Ann Surg Oncol 2014;21:841-2. [Crossref] [PubMed]
- Dapri G, Cardinali L, Cadenas Fabres A, et al. Suprapubic single-incision laparoscopic splenic flexure resection with handsewn intracorporeal anastomosis. Colorectal Dis 2017;19:209-10. [Crossref] [PubMed]
- Dapri G, Antolino L, Bachir N, et al. Up-to-down rectal resection with total mesorectal excision through single-incision laparoscopy. Colorectal Dis 2016;18:627-8. [Crossref] [PubMed]
- Lolle I, Rosenstock S, Bulut O. Single-port laparoscopic rectal surgery - a systematic review. Dan Med J 2014;61:A4878. [PubMed]
- Rattner D. Introduction to NOTES white paper. Surg Endosc 2006;20:185. [Crossref] [PubMed]
- Buess G, Theiss R, Gunther M, et al. Transanal endoscopic microsurgery. Leber Magen Darm 1985;15:271-9. [PubMed]
- McLemore EC, Coker A, Jacobsen G, et al. eTAMIS: endoscopic visualization for transanal minimally invasive surgery. Surg Endosc 2013;27:1842-5. [Crossref] [PubMed]
- Sylla P, Rattner DW, Delgado S, et al. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 2010;24:1205-10. [Crossref] [PubMed]
- Dapri G, Guta D, Grozdev K, et al. Colorectal anastomotic leakage corrected by transanal laparoscopy. Colorectal Dis 2016;18:O210-3. [Crossref] [PubMed]
- Dapri G, Degueldre M. Pure transanal laparoscopic repair of early rectovaginal fistula. Colorectal Dis 2017;19:304-5. [Crossref] [PubMed]
- Dapri G, VanGossum M, Muls V, et al. Trasanal endolaparoscopic circumferential mucosectomy for symptomatic benign rectal stenosis. Colorectal Dis 2017;19:210-11. [Crossref] [PubMed]
- Dapri G, Grozdev K, Guta D, et al. Down-to-up transanal rectal resection with total mesorectal excision assisted by single-incision laparoscopy. Colorectal Dis 2016;18:517-8. [Crossref] [PubMed]
- Leroy J, Barry BD, Melani A, et al. No-scar transanal total mesorectal excision: the last step to pure NOTES for colorectal surgery. JAMA Surg 2013;148:226-30. [Crossref] [PubMed]
Cite this article as: Dapri G. Single-access laparoscopic rectal resection: up-to-down and down-to-up. Ann Laparosc Endosc Surg 2017;2:135.