Single port laparoscopic colorectal surgery: what did we learn from the ECSPECT prospective multicenter registry study?
The development and growth of any new technology or operative procedure brings with it the need for careful scrutiny. First, the concept has to be developed. Then, individual experiences progress and are reported upon, followed by larger experiences and preferably multi-institutional studies. Ultimately, if the question is important enough, a randomized clinical trial is carried out. While it goes without saying that a multi-institutional randomized controlled trial (RCT) represents the most scientifically rigorous approach to address questions in medicine and particularly in the surgical forum, not every question requires or deserves to proceed in this fashion. The ECSPECT trial goes a great distance in terms of addressing questions existing in the surgical community regarding single port (SP) laparoscopic surgery, short of a RCT.
The ECSPECT group must be congratulated for performing and conducting the analysis on such a large number of SP cases. In this British Journal of Surgery article, they present a wonderful experience in a tremendously well-done study. To put this study into perspective, one has to consider the questions that revolve around the innovative technique of SP surgery. Particularly, what serves as a barrier for wide spread adoption of SP colorectal surgery? Can SP surgery be performed safely and effectively? Does it make sense to perform laparoscopic surgery in a SP fashion if SP is harder? Are there benefits to SP surgery? Are there any drawbacks to this approach? Can SP colorectal surgery only be done for right colectomies in highly selected patients or can a variety of colorectal operations be done in a SP fashion? These are the essential and fundamental questions that need to be addressed for wider spread adoption of the SP technique.
With these questions in mind, let us explore what we can learn from the ECSPECT trial. First regarding SP’s safety and efficacy, this study nicely demonstrated a low conversion rate to open surgery of 4.2%. This is better than the conversion rate of 16% in the COLOR II trial (1). Additionally, a low postoperative complication rate of 12.7% is significantly less in comparison to the current norm of 21% of laparoscopic and 20% of open colorectal surgery (2). In terms of predicting which patients might have problems with SP surgery, the study showed a higher complication rate and conversion rate for male sex, ASA grade > I and distal/rectal procedures. However, these findings come as no surprise. Stated differently, hard surgery is hard, especially in high risk patients. Deep pelvic surgery in men with a high ASA will predictably result in worse outcomes. We don’t interpret this as a complication for SP surgery in these patients, but it may help the surgeon to phrase the conversation with the patient regarding expectations around SP surgery. Clearly from this experience, SP surgery has been shown to be safe and effective.
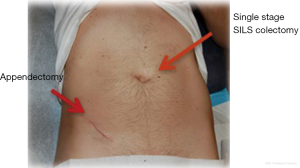
Does it make sense to do colorectal surgery in a SP fashion? If one can repeat the excellent results reported in the ECSPECT trial, the answer is clearly “yes”. With 92% SP surgery completion rate without additional trocars, a low conversion rate and a low postoperative complication rate, SP colorectal surgery makes a lot of sense. Even if there are no clinical differences between SP and multiport (MP) surgery, with a similar safety profile, it is unquestionable that patients prefer to have the improved cosmesis of SP surgery (Figure 1). In terms of the length of hospital stay in this study, it is difficult to interpret the data since this is a European study and mean length of stay is longer in Europe than in the US.
In terms of potential drawbacks of SP surgery, I don’t believe there were any demonstrated. The study shows no increase in morbidity and mortality over what one would expect from MP surgery (Table 1) (1-3). Previously, our research demonstrated that SP colorectal surgery is a safe alternative to MP surgery across an array of procedures in disease-equivalent patients in a case-matched study (N=190) using 7-criteria of age, gender, BMI, previous abdominal surgery, previous XRT, disease process, and procedure. In this study, we showed that SP conversion rates (0% SP versus 1.1% MP; P<0.05) and morbidity rates (10.2% SP versus 16.3% MP; P=0.52) are superior or equivalent to MP without compromising the quality of surgical techniques. We also reported lower EBL in SP surgery, equivalent intraoperative complications, and shorter mean operative time in SP left colectomies compared to the MP approach, with a trend of shorter operating time in all SP procedures (4). All of these findings were similarly reported in the ECSPECT study.
Perhaps, most salient is whether or not this is just a special operation for right colon resections in thin patients. Clearly this does not seem to be the case as there were 1,769 total operations in the ECSPECT trial: 519 right colectomies, 868 left colectomies, 214 rectal resections, 48 APRs, 120 restorative proctocolectomies. Conversion rates as low as 4.2% and even in pelvic cases, a conversion rates of 8.1% is lower in comparison to 11.3% of ACOSOG Z6051, 16% of Color II and 9% of ALaCaRT (1-4). With regard to the patients in which SP surgery can be utilized, is this done in a variety of patients? In looking at the percentage of cases done in a SP fashion over this time, the largest accrual centers were doing between 50–65% cases in SP fashion. This is truly quite impressive and correlates well with our experience (4). Said differently this study shows excellent results for SP surgery over a wide variety of procedures with the approaches used quite well within general colorectal practice.
Of course, as with any study, there are things we would like clarified. One element would be oncologic outcomes of SP surgery. Although the authors mentioned that overall oncologic outcomes were not their targeted-questions, further data upon long-term clinical outcomes (>30 days) and oncologic outcomes of SP surgery would further add strength to this paper. In this regard, we previously demonstrated that SP surgery is not only equivalent in perioperative morbidity but also local recurrence, distant metastasis, and overall 5-year survival rate (4). This clinical evidence would further build the positive SP feasibility and safety profile.
Additionally, while this study shows high utilization of SP technique, there is no explanation of what the indicators were for selecting SP versus MP laparoscopy, which would be quite helpful. Another significant omission in this paper has to do with incision and hernia rates. There has been a large amount written regarding incisional hernia rate, which might be higher in SP cases. This is a significant question for SP cholecystectomy where the extraction site is enlarged to do the operation in SP versus MP fashion. For SP colon surgery, we believe this is not an issue, as there will always be an incision greater than 2.5 cm in order to exteriorize a specimen. Incisional hernia rates of 5% in SP colon surgery and 3–8% in SP cholecystectomy are the currently reported norm in the literature (5). It also would be of interest to see the average size of incisions and number of incisions made. These all would add to the strength of the paper. Perhaps, in a subsequent publication the authors will explore these issues.
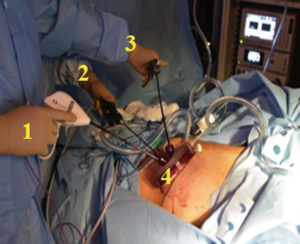
Lastly, from a technical standpoint, questions that were not addressed in this paper that would be very helpful to the surgical community have to do with how the operation was carried out. In particular, what optical systems were used? Was it a flexible tip camera or a straight rod lens system? Were the lenses 0/30/45 degree? Did they use normal length or bariatric length camera? What was the role of curved instrumentation? In our experience, we found either an instrument or camera is needed to be curved in order to get a hand away from operative field to allow two hands operate freely. In our opinion, the easiest most producible way to do this is with flexible tip camera. This will allow camera operators to have their hands well away from the hands of the surgeon. With a single bariatric length in one hand and normal length instrument in the other hand, the operation is able to be carried out through a small opening without a great deal of interference between the hands (Figure 2).
That being said, the authors should again be congratulated for this ECSPECT trial. Certainly, this paper adds justification and support for practitioners of SP surgery as to why and how this can be utilized. Hopefully it will excite others to enter into the field as this is a wonderful option for selected patients. Of course, no arguments have been made that this is for every patient and every surgeon. With proper patient selection and an experienced operative team, this trial shows, without questions, that the patients can be cared for in an effective and safe fashion with good results and argues for SP colorectal surgery to be within the toolbox of all minimal invasive colorectal surgeons.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.05.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015;372:1324-32. [Crossref] [PubMed]
- Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050-9. [Crossref] [PubMed]
- Podda M, Saba A, Porru F, et al. Systematic review with meta-analysis of studies comparing single-incision laparoscopic colectomy and multiport laparoscopic colectomy. Surg Endosc 2016;30:4697-720. [Crossref] [PubMed]
- Marks JH, Montenegro GA, Shields MV, et al. Single-port laparoscopic colorectal surgery shows equivalent or better outcomes to standard laparoscopic surgery: results of a 190-patient, 7-criterion case-match study. Surg Endosc 2015;29:1492-9. [Crossref] [PubMed]
- Julliard O, Hauters P, Possoz J, et al. Incisional hernia after single-incision laparoscopic cholecystectomy: incidence and predictive factors. Surg Endosc 2016;30:4539-43. [Crossref] [PubMed]
Cite this article as: Marks JH, Nagatomo K. Single port laparoscopic colorectal surgery: what did we learn from the ECSPECT prospective multicenter registry study? Ann Laparosc Endosc Surg 2017;2:106.