Reduced-port gastrectomy for gastric cancer with similar port arrangement to conventional five-port laparoscopic gastrectomy
Introduction
Ever since the first reported laparoscopy-assisted gastrectomy by Kitano et al. in 1994 (1), the procedure has been widely adopted as a mainstream approach, particularly in patients with early gastric cancer. The most commonly performed laparoscopic gastrectomy (LG) procedures normally use five ports of 5 or 12 mm in diameter. The laparoscope is inserted from the umbilical port, and four laparoscopic instruments are inserted from four ports setup in a reverse trapezoid shape in the upper abdominal region.
In the recent years, approaches such as reduced-port surgery, which includes single-port surgery, have garnered much attention because of their minimally-invasive nature and improved cosmetic outcomes. The technique has widely been used for patients with cholecystitis (2) and colorectal cancer (3). LG with reduced-port surgery approach has been reported to be performed in patients with gastric cancer (4-11). There are many different types of reduced-port gastrectomy (RPG) for gastric cancer. These include single-port gastrectomy (7,8,11), which is performed through an umbilical incision only, and procedures wherein one (5,6), two (4,9,10), or three ports (11) are used in addition to the umbilical incision. Ports of various diameters of range 2–12 mm are used as additional ports. The optimal port size and their arrangement have not yet been established for RPG.
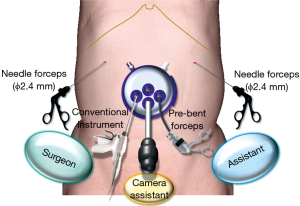
For performing RPG for gastric cancer, we place a multi-channel port (MCP) in the umbilical incision and two needle forceps each of 2.4 mm diameter on the left and right sides of the abdominal wall. For umbilical MCP, we insert a laparoscope and two instruments so that, together with the two needle forceps added to the upper abdominal region, a total of four instruments are available for use. Our RPG procedure is performed using the same technique as that for conventional five-port LG. We hereby report in detail on the RPG procedure that we use for patients with gastric cancer.
Selection of patients
Based on the Japanese gastric cancer treatment guidelines (12), we consider patients with c-stage I gastric cancer (including cT1N0, cT1N1, and cT2N0) to be good candidates for LG, which includes both conventional five-port LG and RPG. For RPG, we insert the instruments that are to be held by the right hand of the surgeon from the umbilical MCP. In patients in whom the distance between the internal operation site and the umbilical region is large and in those in whom the pancreas protrudes in the anterior direction, lymph node dissection in the suprapancreatic area is relatively difficult to perform. Accordingly, patients who have a large physique or are obese are not eligible for RPG. In terms of the resection method, RPG can be performed with the use of this technique for all procedures for which intracorporeal anastomosis is possible after gastrectomy. Thus, RPG is indicated for all types of gastrectomy, including total gastrectomy (TG), proximal gastrectomy (PG), distal gastrectomy (DG), and pylorus-preserving gastrectomy (PPG).
Procedure
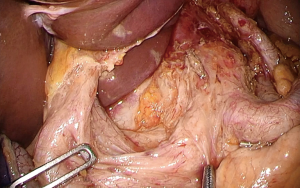
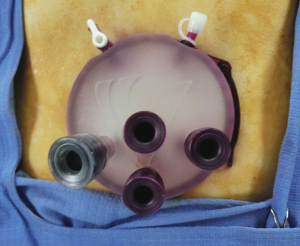
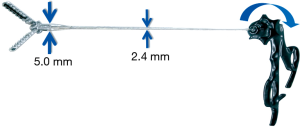
The patient is placed in the supine position with the legs placed wide open. A horizontal or zigzag skin incision (13) of 3.0–3.5 cm is made in the umbilical region. For both these types of incision, a vertical incision is made in the fascia. MCP (GelPOINT access platform; Applied Medical, Rancho Santa Margarita, CA, USA) with four trocars is placed through the umbilical incision (Figure 1), and pneumoperitoneum is performed. Two additional needle forceps (Endo Relief; Hope Denshi Co., Ltd., Chiba, Japan) (14) are inserted into the left and right sides of the upper abdominal wall. Endo Relief forceps have a 2.4-mm diameter shaft and a 5-mm diameter tip (Figure 2). As the tip is thicker than the shaft, these cannot be inserted through the abdominal wall as done with conventional laparoscopic forceps. When setting these up in the abdominal wall, the 2.4-mm shaft is made to pierce the abdominal wall inside out from the peritoneal cavity and outside of the body where it is connected to the handle (Figure 3). In cT1 cases, these are directly setup on the abdominal wall without the use of a trocar. In cT2 cases, a 2.7-mm diameter trocar (Relief Port; Hope Denshi Co., Ltd., Chiba, Japan) made specifically for Endo Relief forceps is used to prevent recurrence at the port site.

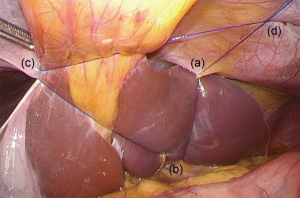
The camera assistant positioned between the patient’s legs inserts a flexible laparoscope through the GelPOINT trocar at the 6 o’clock direction or in the center. The surgeon stands on the right side of the patient and manipulates the conventional laparoscopic instruments from the right trocar on the GelPOINT with his right hand and right abdominal wall needle forceps with his left hand. The first assistant stands on the left side of the patient and uses the pre-bent forceps (Adachi-TANKO forceps; Adachi Industry Co., Ltd., Gifu, Japan) (Figure 4) inserted from the left side of the GelPOINT with his left hand and the left abdominal wall needle forceps with his right hand (Figure 5). The original liver retraction method using 2-0 prolene thread (Ethicon Inc., Cincinnati, OH, USA), which we have named the “Prolene anchoring method”, is used to retract the left lobe of the liver. First, a 2-0 prolene thread attached to a curved needle is passed through the peritoneum at the left subphrenic area, which is considered to be the most appropriate site for retraction, while the left lobe of the liver is lifted using forceps held with the surgeon’s left hand. Next, prolene thread is passed through the peritoneum at the subphrenic area on the right side of the esophageal hiatus and the peritoneum at the right subphrenic area. After detachment of the curved needle, each end of the thread is pulled out through the left upper abdominal wall and fixed for the retraction of the round ligament and the left lobe of the liver (Figures 6,7).

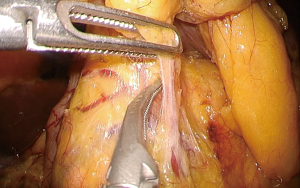
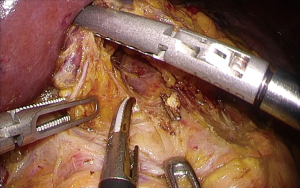
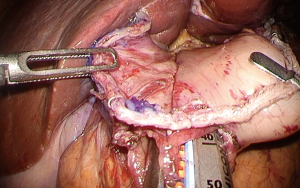
Four instruments are used to retract the organs and tissue and perform lymph node dissection and reconstructive techniques, and the procedure used are similar to those used for the conventional five-port LG (Figures 8,9,10,11,12). Reconstruction is performed with intracorporeal anastomosis. The linear stapler is inserted through the GelPOINT 12-mm trocar, and the circular stapler is inserted directly through the GelPOINT GelSeal cup to be operated by the surgeon. After DG, Roux-en-Y or Billroth-I reconstruction [delta-shaped anastomosis (19)] is performed (Figures 13,14). After PPG, intracorporeal gastro-gastric end-to-end anastomosis is performed with linear staplers. In the case of TG, Roux-en-Y reconstruction is performed, and in the case of PG, jejunal interposition reconstruction is performed. Esophagojejunostomy in cases of TG and PG is performed using the Endo Stitch method (an adapted version of a method for intra-thoracic anastomosis in thoracoscopic esophagectomy that we previously reported (21), which has been modified for use with esophagojejunal anastomosis) or the transorally inserted anvil (OrVil) method (22).

After reconstruction, a 5-mm diameter drain is placed through the umbilical incision. In some cases, such as DG with D1+ dissection or PPG, we do not place a drain postoperatively. After removal of the needle forceps and GelPOINT, the umbilical incision is sutured with absorbable sutures. The needle forceps wound is not sutured, but simply closed with wound-closure tape.
Tips, tricks and pitfalls
Owing to the fewer number of ports used, the RPG technique is more challenging than the conventional five-port LG as fewer instruments are available for organ and tissue manipulation. When a surgeon inserts the two instruments held in his/her left and right hands from a single incision, such as the umbilical incision, manipulation of the instruments is typically challenging and appropriate triangulation is difficult to achieve (23).
To address these shortcomings associated with RPG technique, we adjusted the port arrangement and the devices to develop a new RPG technique, which we have successfully used in over 60 patients with gastric cancer since 2011. Key aspects of our RPG technique are summarized below:
- The technique allows the use of four instruments (two instruments inserted from MCP and additional two needle forceps). Because the same number of instruments can be used as in conventional five-port LG, the method confers the same leverage for organ and tissue manipulation as in the case of conventional five-port LG.
- The surgeon is not required to insert two instruments held by both of his/her hands from a single port, but rather from individual ports, which helps avoid collision between the instruments and allows for similar appropriate triangulation as in conventional five-port LG.
- Because the port arrangement is similar to the reverse trapezoid shape used for conventional five-port LG, organ retraction and lymph node dissection/organ resection can be performed with almost the same technique as used in conventional LG. Since the reconstruction technique is similar to that used in conventional LG, this RPG technique can be used for all types of gastrectomy for which post-gastrectomy intracorporeal anastomosis is possible.
- Because the tip of general needle forceps is small, it does not offer enough tissue holding strength and may cause damage to the tissues if not held deftly. However, because the tip of the Endo Relief forceps is of the same shape and size as that of the conventional 5-mm diameter forceps, it offers sufficient tissue holding strength, and the rotatable shaft can be operated intraoperatively in essentially the same manner as that in conventional 5-mm forceps. As the shaft diameter is extremely thin (2.4 mm), it minimizes postoperative pain. As the postoperative scar becomes invisible after a few months, the cosmetic outcomes of our technique are comparable to those of single-port gastrectomy (Figure 15).
However, a limitation of this technique needs to be taken into account. The surgeon inserts right hand instruments including energy devices such as ultrasonically activated devices and electric cautery, forceps and clip appliers from the umbilical MCP. As already stated in the section on patient selection, patients who have a large physique or those who are obese have a large distance between the umbilical region and the internal site of operation and the pancreas tends to protrude in the anterior direction, which makes it relatively difficult to perform lymph node dissection in the suprapancreatic area in particular. Accordingly, RPG with our technique is not recommended for such patients.
In conclusion, our technique for RPG employs the same number of instruments and similar port arrangement as used in conventional five-port LG. We believe that our technique is a safe and feasible method for RPG that can be performed by all laparoscopic surgeons owing to the similarity in the methods. Our technique can also achieve almost the same postoperative pain reduction and excellent cosmetic outcomes as observed with single-port gastrectomy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chikara Kunisaki) for the series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.03.14). The series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 1994;4:146-8. [PubMed]
- Hernandez JM, Morton CA, Ross S, et al. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg 2009;75:681-5; discussion 685-6. [PubMed]
- Bucher P, Pugin F, Morel P. Single-port access laparoscopic radical left colectomy in humans. Dis Colon Rectum 2009;52:1797-801. [Crossref] [PubMed]
- Omori T, Oyama T, Akamatsu H, et al. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc 2011;25:2400-4. [Crossref] [PubMed]
- Kunisaki C, Ono HA, Oshima T, et al. Relevance of reduced-port laparoscopic distal gastrectomy for gastric cancer: a pilot study. Dig Surg 2012;29:261-8. [Crossref] [PubMed]
- Kawamura H, Tanioka T, Kuji M, et al. The initial experience of dual port laparoscopy-assisted total gastrectomy as a reduced port surgery for total gastrectomy. Gastric Cancer 2013;16:602-8. [Crossref] [PubMed]
- Omori T, Masuzawa T, Akamatsu H, et al. A simple and safe method for Billroth I reconstruction in single-incision laparoscopic gastrectomy using a novel intracorporeal triangular anastomotic technique. J Gastrointest Surg 2014;18:613-6. [Crossref] [PubMed]
- Ahn SH, Park DJ, Son SY, et al. Single-incision laparoscopic total gastrectomy with D1+beta lymph node dissection for proximal early gastric cancer. Gastric Cancer 2014;17:392-6. [Crossref] [PubMed]
- Usui S, Tashiro M, Haruki S, et al. Triple-incision laparoscopic distal gastrectomy for the resection of gastric cancer: comparison with conventional laparoscopy-assisted distal gastrectomy. Asian J Endosc Surg 2014;7:197-205. [Crossref] [PubMed]
- Misawa K, Ito S, Ito Y, et al. Reduced-port distal gastrectomy for gastric cancer using two needle devices, a GelPOINT device, and an umbilical zigzag incision. J Laparoendosc Adv Surg Part B Videoscopy 2014;24: [Crossref]
- Inaki N. Reduced port laparoscopic gastrectomy: a review, techniques, and perspective. Asian J Endosc Surg 2015;8:1-10. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017;20:1-19. [Crossref] [PubMed]
- Hachisuka T, Kinoshita T, Yamakawa T, et al. Transumbilical laparoscopic surgery using GelPort through an umbilical zigzag skin incision. Asian J Endosc Surg 2012;5:50-2. [Crossref] [PubMed]
- Ishii M, Nishiyama T, Naganuma H, et al. Development of new small diameter forceps for reduced-port surgery. J Jpn Soc Endosc Surg 2012;17:267-71.
- Misawa K, Ito S, Ito Y, et al. Setup of Endo Relief needle forceps. Asvide 2017;4:160. Available online: http://www.asvide.com/articles/1468
- Misawa K, Ito S, Ito Y, et al. “Prolene anchoring method” for liver retraction. Asvide 2017;4:161. Available online: http://www.asvide.com/articles/1469
- Misawa K, Ito S, Ito Y, et al. No. 6 lymph node dissection in the infra-pyloric area. Asvide 2017;4:162. Available online: http://www.asvide.com/articles/1470
- Misawa K, Ito S, Ito Y, et al. Lymph node dissection in the supraduodenal area and suprapancreatic area. Asvide 2017;4:163. Available online: http://www.asvide.com/articles/1471
- Kanaya S, Gomi T, Momoi H, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 2002;195:284-7. [Crossref] [PubMed]
- Misawa K, Ito S, Ito Y, et al. B-I reconstruction (delta-shaped anastomosis). Asvide 2017;4:164. Available online: http://www.asvide.com/articles/1472
- Misawa K, Hachisuka T, Kuno Y, et al. New procedure for purse-string suture in thoracoscopic esophagectomy with intrathoracic anastomosis. Surg Endosc 2005;19:40-2. [Crossref] [PubMed]
- Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 2009;23:2624-30. [Crossref] [PubMed]
- Kodera Y. Reduced port surgery for gastric cancer: another giant leap for mankind? Gastric Cancer 2013;16:457-9. [Crossref] [PubMed]
Cite this article as: Misawa K, Ito S, Ito Y, Shigeyoshi I, Komori K, Shimizu Y, Kinoshita T. Reduced-port gastrectomy for gastric cancer with similar port arrangement to conventional five-port laparoscopic gastrectomy. Ann Laparosc Endosc Surg 2017;2:73.