A new contrivance of single port and reduced port gastrectomy for gastric cancer
Introduction
The recent development of laparoscopic surgery includes the introduction of single-port laparoscopic surgery. However, various single-port operations are difficult for laparoscopic surgeons to perform because of conflict of some instruments and the laparoscope. Moreover, single-port laparoscopic surgery reduces postoperative pain and has advantages of cosmetic merit (1-3).
To overcome the difficulty from the conflict of some instruments and camera in single-port laparoscopic gastrectomy (SPG), we used special access platform and created the surgical techniques. Moreover, additional ports were inserted for optimal surgical manipulation in reduced-port laparoscopic gastrectomy (RPG). We had used the combination method of pneumoperitoneum and abdominal wall lifting (4,5) to secure the visual field and obtain the proper angle for manipulation in RPG. RPG is favorably accepted by patients with early gastric cancer because the postoperative pain and recovery time are similar with those in conventional laparoscopic gastrectomy (6,7). In this study, we assessed that safety of SPG and RPG performed with our special surgical technique and estimated with benefits of combination of pneumoperitoneum and abdominal wall-lift method.
Methods
Ninety-five patients with preoperative stage IA gastric cancer underwent SPG and RPG with D1+ lymphadenectomy between April 2005 and May 2016 at Hiroshima Prefectural Hospital. All the patients were classified in accordance with the TNM criteria for gastric cancer (8). Thirty patients underwent SPG, and 65 patients underwent RPG.
The surgical procedure
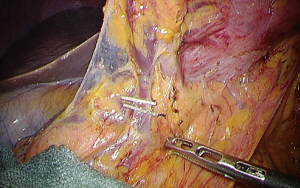
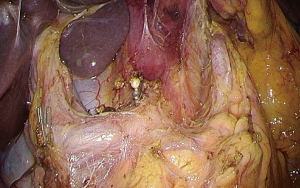
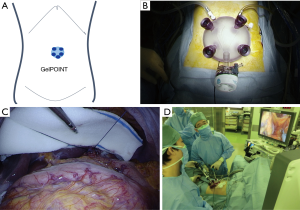
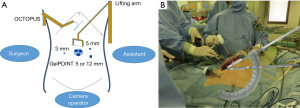
In the operation theater, the patients received general anesthesia and placed in the supine position. The surgeon stood on the right side; the assistant, on the left side; and the camera operator, between the patient’s legs. In SPG, a 3.5 cm umbilical vertical skin incision and fasciotomy were performed on the peritoneal cavity. A multi-channel access platform (GelPOINT; Applied Medical, Rancho Santa Margarita, CA, USA) was set up through the umbilical incision (Figure 1A). A multi-channel access platform was created by attaching four 10-mm trocars and a 12-mm trocar. A flexible laparoscope was introduced through the 12-mm trocar (Figure 1B). Thereafter, pneumoperitoneum of 8-mmHg pressure was established. A water expanding sponge (Endoractor; Kawamoto, Osaka, Japan) was introduced into the abdominal cavity from the umbilical incision and placed under the left lobe of the liver. A straight needle with 2-0 nylon thread was introduced via a percutaneous puncture through the right tendon of the diaphragm and withdrawn percutaneously and by extracorporeal ligation (Figure 1C).
The surgeon dissected the left side of the greater omentum, and the left gastroepiploic artery and vein were isolated and divided (Figure 1D).
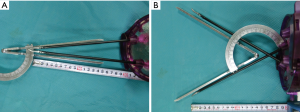
In SPG, manipulation of the tissue is sometimes difficult because of lack of appropriate triangulation (Figure 2A). Therefore, we developed the X-technique by using two straight laparoscopic instruments across through the multi-channel access platform. Figure 2B shows the X-technique, which involves reverse triangulation by using two straight instruments (Figure 3).

In RPG, an abdominal wall-lifting retractor is set up on the left side of the operation table. A 1.2-mm-long Kirschner wire was inserted in the subcutaneous tissue of the upper umbilicus lesion. An additional 3-mm trocar for the surgeon and 3- and 5-mm (or 12-mm) trocars for the assistant were inserted for optimal surgical manipulation.
Abdominal wall lifting can provide a wider intra-abdominal operative field with 8 mmHg of pressure in the pneumoperitoneum (Figure 4A). Passage of several instruments and a flexible scope was possible through three trocars via the multi-access platform with the combination of 8-mmHg pneumoperitoneum and the abdominal wall-lift method, which could provide a 30° proper angle and a wide visual field (Figures 4B,5).

The greater omentum was dissected by using combined laparoscopic ultrasonic coagulating and bipolar sealing shears (Thunderbeat; Olympus Optical, Tokyo, Japan) or laparoscopic ultrasonic coagulating sears (Harmonic A+; Ethicon Endosurgery, Cincinnati, USA) from the left to the right side. For one of the station of lymphadenectomy, the right gastroepiploic vein was isolated and divided (Figure 6). The right gastroepiploic artery was ligated with an endoclip applicator (5-mm Liga Clip; Ethicon Endosurgery, Cincinnati, USA) and divided with No. 6 lymphadenectomy. The right gastric artery was clipped and divided with No. 5 lymphadenectomy. Next, lymph node dissection of the suprapancreatic area was performed with the medial approach (Figures 7,8).

Gastrectomy was performed by using an endolinear stapler (60-mm Powered Echelon Flex; Ethicon Endosurgery Co., Ltd., USA). Reconstruction was performed with functional end-to-end anastomosis; gastroduodenostomy, with the Billroth-I method (Figure 9); gastrojejunostomy with Roux-Y after distal gastrectomy (DG); gastrogastrostomy with pylorus-preserving gastrectomy (PPG) and esophagojejunostomy, with total gastrectomy (TG).

Statistical analysis
Continuous data were expressed as mean ± SD. The statistical analyses were performed with the JMP 13.0 software (SAS Institute Inc., Cary, USA). Data comparison was performed by using Fisher and Student’s t-tests. Statistical significance was established at P<0.05.
Results
The characteristics of the 95 patients are summarized in Table 1. The surgical results of the 95 patients are summarized in Table 2.
Table 1
| Characteristics | SPG group (n=30) (%) | RPG group (n=65) (%) | P value |
|---|---|---|---|
| Age (years) | 0.887 | ||
| Range | 49–90 | 42–93 | |
| Mean | 69.4 | 66.3 | |
| Gender, n (%) | |||
| Male | 11 (36.7) | 45 (69.2) | |
| Female | 19 (63.3) | 20 (30.8) | 0.0036 |
| Platform | GelPOINT | GelPOINT: +3 mm, +5 mm (+12 mm) | |
| Type of operation | B-I: 11; DG-RY: 6; PPG: 13 | B-I: 26; DG-RY: 15; PPG: 15; PG: 1; TGRY: 9 |
SPG, single port laparoscopic gastrectomy; RPG, reduced port laparoscopic gastrectomy.
Table 2
| Variables | SPG (n=30) | RPG (n=65) | P value |
|---|---|---|---|
| Operation time [mean], min | 218–471 [323] | 238–467 [320] | 0.595 |
| Blood loss [mean], g | 10–357 [67] | 4–470 [63] | 0.591 |
| Complication, Clavien Dindo < III | Intra-abdominal abscess: 1 | Anastomotic bleeding: 1; leakage of duodenal stump: 1 |
SPG, single port laparoscopic gastrectomy; RPG, reduced port laparoscopic gastrectomy.
No significant differences in amount of blood loss [10–357 (mean: 67) vs. 4–470 (mean: 63) mg, P=0.591] and operation time [218–471 (mean: 323) and 238–467 (mean: 320) min, P=0.595] were found between the SPG and RPG groups. Intra-abdominal abscess occurred in one patient (3.3%) in the SPG group.
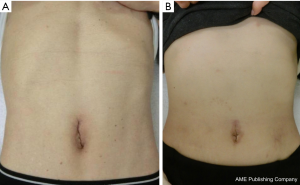
Anastomotic bleeding and leakage of duodenal stump occurred in 2 patients (3.1%) in the RPG group. Conversion to open surgery was not necessary in all the cases. All the patients who underwent SPG and RPG successfully were satisfied because of the less pain and cosmetic operation scar (Figure 10A: after SPG, Figure 10B: after RPG).
Discussion
Laparoscopic-assisted distal gastrectomy (LADG) was first performed by Kitano et al. in 1994 with the abdominal wall-lift method by using U-shaped retractor elevation (13). The usefulness of LADG for patients with early gastric cancer was investigated because it was associated with less surgical trauma, less pain and rapid return to normal activity without decrease in surgical curability (14). Patients who underwent LADG had better quality of life than those who underwent open DG (15). As we previously reported (16), laparoscopic-assisted PPG was indicated for patients with cancer in the middle third of the stomach. Single-incision laparoscopic gastrectomy was first reported by Omori et al. in 2011 (17). SPG is difficult for many laparoscopic surgeons to perform because of conflict of some instrument and the laparoscope. Therefore, surgical techniques should be considered for performing SPG when conflict of the endoscopic forceps, energy device, and flexible endoscopy is expected. In many procedures in single-port surgery, handling the forceps and the camera without clashing is difficult. Owing to the loss of triangulation by parallel entry of the two instruments used by the surgeon, the operation becomes more difficult to perform than conventional laparoscopic surgery. Articulated or curved instruments were developed for single-port surgery, but a crossover setting is still necessary (18). While surgical outcomes depend on the surgeon’s skill in single-port laparoscopic surgery, the surgeon’s effort is needed to improve the technique. Parallel movement in the same direction limit the movement range and is more difficult to manipulate. On the other hand, fulcrum movement allows instruments to diverge from the target point. Without switching hands, we used the chopstick effect to switch between the right and left sides.
Therefore, we developed a technique called the X-technique, in which two endoscopic conventional straight forceps or energy device was crossed over through the platform to make a reverse triangulation. The X-technique provides an optimal countertraction of the target tissue and a moving wide angle without using articulated or curved instruments. We performed SPG safety by using the X-technique.
By contrast, the choice of RPG is reasonable from the standpoint of patient safety.
An additional 3-mm trocar by the surgeon and 3- and 5-mm (or 12-mm) trocars by the assistant were inserted for optimal surgical manipulation without hesitation. In addition, we acquired a wide workspace and elevated the cranial side by additional abdominal wall lifting. Cranial elevation of the platform enabled us to manipulate the tissue owing to the smooth manipulation of the instruments with proper manipulation angle.
In this study, we assessed the safety of performing RPG with additional trocars and workspace provided by the combination of pneumoperitoneum and abdominal wall-lift method. Based on our retrospective study, no significant difference was found between SPG and RPG. The choice between SPG and RPG by the patient should be made with consideration of patient safety. RPG offers less invasiveness and cosmetic advantage for patients with early gastric cancer.
Conclusions
SPG was safely and feasibly performed with our special surgical technique, and RPG was safely and easily performed in the wide working space provided by the combination of pneumoperitoneum and abdominal wall-lift method in the patients with early gastric cancer.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chikara Kunisaki) for the series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.20). The series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. Institutional ethical approval was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Navarra G, Pozza E, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg 1997;84:695. [Crossref] [PubMed]
- Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 1999;9:361-4. [Crossref] [PubMed]
- Kala Z, Hanke I, Neumann C. A modified technic in laparoscopy-assisted appendectomy--a transumbilical approach through a single port. Rozhl Chir 1996;75:15-8. [PubMed]
- Nagai H, Kondo Y, Yasuda T, et al. An abdominal wall-lift method of laparoscopic cholecystectomy without peritoneal insufflation. Surg Laparosc Endosc 1993;3:175-9. [PubMed]
- Banting S, Shimi S, Vander Velpen G, et al. Abdominal wall lift. Low-pressure pneumoperitoneum laparoscopic surgery. Surg Endosc 1993;7:57-9. [Crossref] [PubMed]
- Kim SM, Ha MH, Seo JE, et al. Comparison of Reduced Port Totally Laparoscopic Distal Gastrectomy (Duet TLDG) and Conventional Laparoscopic-Assisted Distal Gastrectomy. Ann Surg Oncol 2015;22:2567-72. [Crossref] [PubMed]
- Kunisaki C, Makino H, Kimura J, et al. Application of reduced-port laparoscopic total gastrectomy in gastric cancer preserving the pancreas and spleen. Gastric Cancer 2015;18:868-75. [Crossref] [PubMed]
- Sano T, Coit DG, Kim HH, et al. Proposal of a new stage grouping of gastric cancer for TNM classification: International Gastric Cancer Association staging project. Gastric Cancer 2017;2:217-25. [PubMed]
- Urushihara T, Tokumoto N, Takakura Y, et al. X-technique, in which two straight forceps are crossed over through the platform to make a reverse triangulation. Asvide 2017;4:156. Available online: http://www.asvide.com/articles/1464
- Urushihara T, Tokumoto N, Takakura Y, et al. Set up of a multi-channel platform and abdominal wall lifting, and lymphadenectomy of No. 4sb, No. 6 and No. 5 in RPG. Asvide 2017;4:157. Available online: http://www.asvide.com/articles/1465
- Urushihara T, Tokumoto N, Takakura Y, et al. Lymph node dissection of the suprapancreatic area was performed with the medial approach. Asvide 2017;4:158. Available online: http://www.asvide.com/articles/1466
- Urushihara T, Tokumoto N, Takakura Y, et al. Reconstruction was performed with functional end-to-end anastomosis; gastroduodenostomy, with the Billroth-I method by using an endolinear stapler. Asvide 2017;4:159. Available online: http://www.asvide.com/articles/1467
- Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 1994;4:146-8. [PubMed]
- Huscher CG, Mingoli A, Sgarzini G, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 2005;241:232-7. [Crossref] [PubMed]
- Adachi Y, Shiraishi N, Shiromizu A, et al. Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg 2000;135:806-10. [Crossref] [PubMed]
- Urushihara T, Sumimoto K, Shimokado K, et al. Gastric motility after laparoscopically assisted distal gastrectomy, with or without preservation of the pylorus, for early gastric cancer, as assessed by digital dynamic x-ray imaging. Surg Endosc 2004;18:964-8. [Crossref] [PubMed]
- Omori T, Oyama T, Akamatsu H, et al. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc 2011;25:2400-4. [Crossref] [PubMed]
- Botden S, Strijkers R, Fransen S, et al. The use of curved vs. straight instruments in single port access surgery, on standardized box trainer tasks. Surg Endosc 2011;25:2703-10. [Crossref] [PubMed]
Cite this article as: Urushihara T, Tokumoto N, Takakura Y, Oshita A, Ikeda S, Matsugu Y, Nakahara H, Itamoto T. A new contrivance of single port and reduced port gastrectomy for gastric cancer. Ann Laparosc Endosc Surg 2017;2:72.