I am your eyes—the reflection of being a camera-holder in laparoscopic gastrointestinal surgery
Introduction
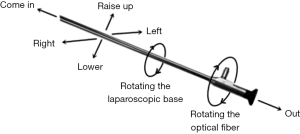
There are two kinds of laparoscopy regarding the direction of view: 0° and 30°. The 30° laparoscopy can provide a wide-field view of operative field in multiple angles by rotating the fiber optics (Figure 1), which it is good for showing the frames of surgery and increasing the safety of surgery. As a result, it is adopted by lots of hospital.
Owing to lack of touch, a high quality of visualization is required in laparoscopic surgery. It is necessary for a camera-holder to provide an optimum visualization of operative view which is stable and clear. Also, the camera-holder should have a good teamwork with other operators. A qualified camera-holder should have the ability to learn and summarize from experiences.
Stable
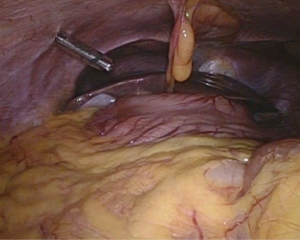
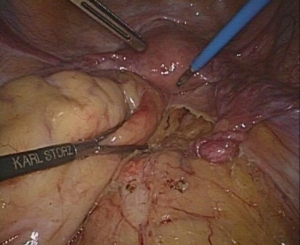
During laparoscopic surgery, the view of operative field should be stable, and the target dissection should be in the center of the screen (Figure 2). The camera-holder needs to avoid the fast-movements and frequent rotations which might cause visual fatigue. This requires the camera-holder to have a clear understanding of the surgical procedures, which helps to cooperate by the operating surgeon with each step in a real-time basis. Generally, the camera follows the operating ongoing direction, and move slowly and exactly, so that the surgeon feel comfortable during surgery.
Clear
Before the surgery, we should test the laparoscopy, including white balance, focus, adjusting the brightness, aperture, wiping lens and so on. Fogging and polluting of the lens is the main reasons to the blurry view in surgeries.
The reason of lens fogging is that the temperature of the lens is lower than that of the enterocoelia. Fogging liquidates the lens, and it leads to dim images. Currently, most hospitals use gauze with iodine to scrub the lens. It can clean the feculence on the lens. Moreover, the iodine can create a protective layer to reduce the surface tension and weaken the ability the fog formation. However, when the lens is close to the harmonic scalpel and the electrotome, the lens would still turn foggy because of the significant temperature difference. In order to minimize the temperature difference and prevent fogging, some surgeons soak the lens in warm saline. In general, the temperature of the saline is between 60–70 °C. Before operation, the lens should be soaked in the saline for 60 seconds. During the operation, this process can be shortened to several seconds. Surgeons use the dry gauze to scrub the lens after taking the lens out from the saline and putting it into the abdomen as soon possible. When fogging or polluting takes place in some emergency situations, and the operation cannot be stopped, camera-holders can wipe the lens on the viscera or the omentum. By this way, it requires that the lens should contact with the viscera completely, briefly, and gently. Once the emergency situation is settled, the lens can be taken to clean. However, sometimes it can be blurrier by doing this, so operators should be cautious to adopt this method. If there is at least one-quarter of the screen being clear, operators should put the operation view at the center of the clear screen. It could save time and the surgery would not be interrupted if camera-holders wipe and soak the lens at the same time when other operators change the appliance.
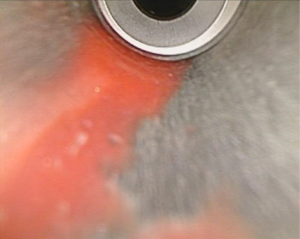
Most lens pollutions are due to narrow space (presacral space, lateral wall of rectum) or getting too close to the surgical site. Especially when the tissue is edematous, bleeding, or adipose, the mist generated by ultrasonic knife, the fragment of tissue, and blood could make the lens dirty. When the ultrasonic knife is working, the lens should be moved backwards to protect the lens, and the lens could be moved forwards after the ultrasonic knife procedure is finished. Meanwhile, the operative field should always be kept in the center of the view. In addition, lens entering trocar is another way to get lens polluted. Because of the pressure difference between enterocoelia and the atmosphere, it pushes out the liquid drop and the tissue from the trocar that causing the lens polluted. Also, the polluted valve can contaminate the lens easily (Figure 3). Therefore, cleaning the trocar before the lens entering the trocar is recommended.
Expose
In general, the camera-holder could use the 30° laparoscopy to display a nice image of surgery for the other operators. The camera-holder should show the operative field sufficiently, but avoid arm collision.
Fully understanding of the construction of the 30° laparoscopy is the basis of effectively using it. It consists of the laparoscopic base and fiber-optics. It has four planes and one deepness (Figure 4), i.e., rotating the optical fiber in 360°, rotating the laparoscopic base in 90°, the laparoscopic base wiggles to left or right in 360°, raise up or lower the laparoscopic base in 90°, and the laparoscopy comes in and out.
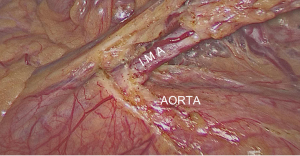
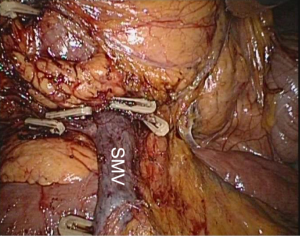
The laparoscopic base is similar to a human body (Figure 5). When operating, the operator should put it in a flat plane to provide the same angle of view as the open operation. No matter how to change the position during operation, the viscera should be in a horizontal position and the base should be parallel to the operative field, or the vertical axis lens barrel and base should be vertical to the operative field. When the patient is at the left lateral position, the base should rotate to left to maintain the angle, and so as to the right lateral position. During operation, operators can make reference to the viscera. For example, when having an operation at upper abdomen, operators should keep the liver and pancreas horizontal (Figure 6); when having an operation at lower abdomen, operators should keep the uterus and the urinary bladder at 12 o’clock position (Figure 7); when dissociating the inferior mesenteric vessels, operators should keep the abdominal aorta horizontal (Figure 8); when dissociating the right colon vascular, operators should keep the superior mesenteric vein (SMV) vertical (Figure 9). In brief, operators should rotate the base on the basis of the different operating plane.
The laparoscopy could go forward and backward to achieve the best view. When it goes forward, the view becomes smaller and displays more details of the target dissection; when it goes backward, the view becomes bigger and the image of target dissection is shrunken. In most cases, operators would choose a perfect visual to have a better knowledge of the overall structure including the target and the surrounding dissection. When having a micro or dangerous operation, operators should use close-up viewing. When trying to recognize the anatomical position or searching, a distanced viewing would be more effective. In addition, camera-holders should timely adjust the laparoscopy (i.e., wiggle to left or right, raise and lower the laparoscopy) to coordinate with rotated fiber optics and keep the operating dissection at the middle of screen.
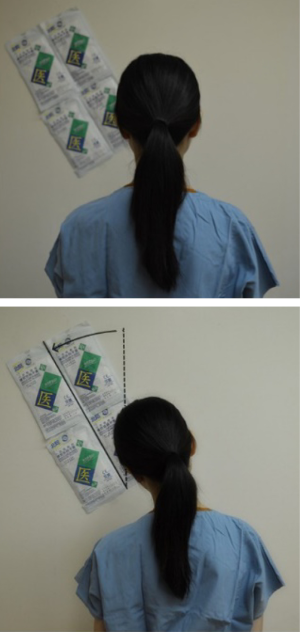
Rotating the fiber optics can provide another plane for 30° laparoscopy. To rotate the fiber optics’ mirror surface is similar to rotate human head with long braid, and the fiber optics moves in opposite direction as the surface goes. The displayed image would not be bottom up. For example, when the fiber-optic is rotated to the left, it will show the right. When it is rotated by 180°, it will show the top, which is called “looking at the ceiling”. This is an important method in radical proctectomy for rectal cancer when dissecting the anterior sacral ligament.
It is important to understand when to rotate the 30° laparoscopy camera. First of all, the aim of rotating the 30° laparoscopy is to provide an optimum view that we can observe the target dissection and operating apparatus. During an operation, there are many situations that may cause poor viewing (not showing the overall structure or only showing the end of the operating apparatus), such as limited operating space, inappropriate angle, or the unsatisfied trocar location. If operators force to operate, other tissue may be injured. Especially when denudating the vessel, it leads to bleed easily. Therefore, we rotate the fibers to adjust the angle of view to avoid unnecessary injury. Second, rotating the 30° laparoscopy can provide an excellent angle of view for other operators. Some camera-holders may keep the operative field at the middle of screen, but they are unable to show a clear image of the tissue around or behind because of an inappropriate angle. By adjusting the angle of the optic fiber, coordinating with the wiggling laparoscopy, and maintaining vertical angle to operating position, so that operators can obtain the better view and recognize the anatomy, and avoid injury. At last, to rotate 30° laparoscopy can reduce the problem causing by wide-angle wiggling laparoscopy. Wide-angle of wiggling may disturb the operator. Rotating 30° laparoscopy can decrease the angle of wiggling. Since the body of laparoscopy and fiber optics are not independent sections, rotating the fiber optics should coordinate with the body of laparoscopy.
Cooperation
A successful surgery requires that the operator, camera-holder and nurse should cooperate with each other. As a camera-holder, one should not only understand the basic principle of control the camera, but also try to understand every operation, every step of the operation, and the habit of every operator, so that the camera-holder can better predict the operator’s intention in advance, and provide the best view for the operator. Holding the laparoscopy is not only a physical work, but also a technical work. Only when we practice and make summarization constantly, can we master the skill of holding the laparoscopy and make the operation fluent.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.23). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Zheng J, Wang J, Li Y. I am your eyes—the reflection of being a camera-holder in laparoscopic gastrointestinal surgery. Ann Laparosc Endosc Surg 2017;2:62.