
Myxedema pseudovolvulus: case series and review of the literature
Case 1 presentation
A male in his late thirties presented to our institution with a chief complaint of abdominal pain. The patient reported three days of worsening, generalized abdominal pain with constipation that had progressed to obstipation. The patient also admitted to increased lethargy over the past 6 months. He denied nausea, vomiting, depressed mood, and any other psychiatric or neurologic complaints. Past medical history was significant for gastrointestinal reflux and chronic constipation. The patient denied taking any medications regularly and his social and family histories were noncontributory.
On presentation, the patient had blood work drawn with the following results: white blood cell count was 5.1 k/µL, hemoglobin 9.6 g/dL, hematocrit 28.2%, platelet count 167 k/µL, total bilirubin 1.0 mg/dL, amylase 55 µ/L, lipase 27 µ/L, lactate 2.0 mmol/L.
The patient’s chest X-ray showed gaseous distention of the colon prompting further investigation. He was then sent for CT scan of his abdomen, which revealed findings consistent with sigmoid volvulus.
The patient was then taken emergently to the operative theater for decompression and exploration. Intraoperatively, there was a finding of a large dilated sigmoid colon with point of torsion at a dense adhesion of the colon with small bowel mesentery. The colonic diameter was greater than 10 cm with collapse of the proximal and distal segments. Colonic ischemia was present prior to untwisting the volvulus. Following detorsion, warm soaked laparotomy pads were applied to the affected sigmoid colon however there were no signs of reperfusion. As a result, the patient then underwent a sigmoid resection with primary anastomosis of the descending colon and the rectum. The resected specimen can be seen in Figure 1. No other intraoperative abnormalities were found. Post-operatively, the patient’s diet was slowly advanced with return of normal bowel function on the third postoperative day. As part of an evaluation to the cause of the patient’s chronic constipation, a thyroid panel was sent with the following results: TSH >150 mc/mL, free T3: <0.2 pg/mL, free T4: 0.12 ng/dL.
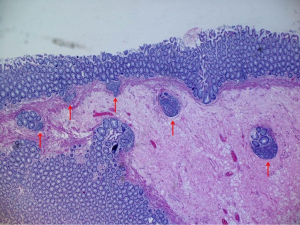
The patient was newly diagnosed with hypothyroidism, and was started on thyroid hormone replacement therapy using levothyroxine sodium. The patient had an uncomplicated hospital course during which lethargy improved. The patient was sent home tolerating a regular diet, having regular bowel movements, and was prescribed continuing thyroid hormone replacement. The final histopathology on the surgically resected specimen revealed benign colonic mucosa with edema and lymphoid aggregates along with diverticulosis coli, which can be seen in Figure 2.
Case 2 presentation
An Asian male in his thirties presented with a two-week history of increasing abdominal pain and distention. At the time of presentation, the pain had increased to an 8/10 severity. The patient admitted to a past medical history significant for hypothyroidism. On physical exam, there was significant distention and the abdomen was tympanic to percussion. The patient underwent X-ray and CT scan of the abdomen/pelvis, which showed sigmoid dilatation and volvulus (Figures 3,4). His laboratory findings confirmed a diagnosis of hypothyroidism with a TSH of 24.6 mc/mL and a free T4 of 0.71 ng/dL. His other lab works showed a white blood cell count was 6.9 k/µL, hemoglobin 15.1 g/dL, hematocrit 45.6%, and platelet count 400 k/µL.

The team elected to treat this patient conservatively and performed a colonoscopic decompression after administering bowel prep. The patient subsequently underwent a second colonoscopy, confirming the absence of any mechanical obstruction. He was then started on thyroid hormone replacement therapy with levothyroxine at 35 mcg IV daily. The patient’s volvulus resolved and he had return of normal bowel function. He was subsequently discharged to home with medical and surgical follow-up.
Discussion
Hypothyroidism is one of the most common diagnoses in the United States. It increases in prevalence with increasing age and affects as much as 10% of the population over the age of 65. Hypothyroidism can present in a number of different ways. The presenting signs and symptoms can range from minor, such as fatigue, thinning hair, or constipation, to life threatening and severe presentations including pseudovolvulus, seizures, neurological dysfunction, and myxedema coma (1). The diagnosis should always be considered when patients present with a number of vague complaints as it can manifest in a multitude of ways.
Vague abdominal symptoms such as constipation or nonspecific abdominal pain are commonplace in the setting of hypothyroidism. However, if unrecognized or untreated, these symptoms can progress to a severe complication of hypothyroidism, myxedema pseudovolvulus.
Colonic volvulus ranks as the third most common cause of large-bowel obstruction in the United States following cancer and diverticulitis respectively. It is estimated that volvulus is responsible for approximately 5% of all cases of intestinal obstructions and 10–15% of large bowel obstructions. Colonic volvulus is defined as torsion of the bowel around its own mesentery, which, if untreated, can interfere with the blood supply to that section of bowel and progress to ischemia, gangrene, or possibly death (2). The sigmoid colon is the most common site of large bowel torsion followed by the cecum, transverse colon, and the splenic flexure (3). It is an extremely common presentation and can is further characterized by the presence or absence of a mechanical obstruction.
Colonic volvulus is characterized as dynamic; it is secondary to a mechanical obstruction. In contrast, the volvulus associated with hypothyroidism is referred to as a pseudovolvulus, or an adynamic obstruction, secondary to a lack of intestinal motility (4). There are several case reports in the literature describing pseudoobstruction precipitated by hypothyroidism, termed myxedema pseudovolvulus (5-12). Despite these reports, the condition remains exceedingly rare in clinical practice. Treating physicians should always consider it as a possible differential diagnosis especially if the patient presents with signs and symptoms corresponding to hypothyroidism. Commonly reported signs and symptoms can be as subtle as thinning hair, increased fatigue, and decreased deep tendon reflexes, to as severe as altered mental status and myxedema coma. Other unique presentations have been described such as dementia (6) and urinary retention (11). Occasionally, the only clue that can lead to this diagnosis is a distant history of thyroidectomy or a decrease in the dose of levothyroxine. As always, history plays a key role in correctly identifying and diagnosing these patients.
Many attempts have been made to understand the myxedema pseudovolvulus. Since many cases are treated conservatively, there has been limited examination of surgical specimens. Grossly, there have been many observations made about the appearance of the affected bowel. The loss of colonic haustra has been noted, likely secondary to the lack of motility (12). One of the leading theories is that the decreased colonic motility is a peripheral neuropathy of the myenteric plexus, which is related to the polyneuropathy commonly seen with myxedema (13). Mucopolysaccharide deposition causes the polyneuropathy in these patients, however, it generally disappears with the administration of thyroid hormone. Further backing up this idea is data from one study conducted on rats. Researchers found that hypothyroidism does in fact lead to impaired colonic motility (14). Rats whose thyroids were removed showed a relative dilatation of the colon as well as increased colonic transit times. When researchers gave the rats thyroid replacement treatment, they found improvements in transit times. This shows that nonsurgical intervention can be successful in the treatment of myxedema pseudovolvulus. The administration of levothyroxine can restore colonic motility and can treat an adynamic obstruction.
Another study performed autopsies on 10 patients with myxedema pseudovolvulus to better characterize the pathology in which several distinct patterns were noted. The most common finding in this study was mast cell accumulation throughout the muscularis propria and the submucosa. In addition to this, PAS positive metachromatic granules were found in perivascular areas in the specimens. Furthermore, there was deposition of a mucopolysaccharide and hyaluronic acid rich mucoid substance in the bowel. These findings were a very important breakthrough in the pathological characterization of myxedema pseudovolvulus. Mast cell accumulation is a hallmark finding in myxedema. The mast cells can then produce hyaluronic acid that progresses to the mucopolysaccharide mucoid substance that gathers in the perivascular areas (15). This further supports other hypotheses that the mucopolysaccharide aggregation causes the polyneuropathy associated with hypothyroidism. In the bowel this can lead to constipation, which can progress to ileus and eventually pseudovolvulus.
Other studies have shown various other findings in myxedematous bowel. Infiltration of lymphocytes and plasma cells into the submucosa is commonly seen as well as diffuse atrophy of the stroma. These plasma cells and lymphocytes are deposited in Auerbach’s plexus and can lead to a decrease in elasticity and contractility in the muscle (16). We noted this lymphocytic infiltrate in the specimen resected from our first patient. Lymphoid aggregates were noted in the colonic wall of the specimen when it was examined microscopically. This correlates with the changes shown in literature for myxedema pseudovolvulus.
Treatment of these patients is highly depended on the clinical scenario. In most cases, surgical management should be coupled with thyroid hormone replacement. One important factor to note in the initial decision making process is that subjecting a severely hypothyroid patient to a stressor like laparotomy can precipitate a myxedema coma state (17,18). Though the patient’s vitals and clinical presentation may warrant an emergent trip to the operating room, the treating team should bear in mind the possible after effects of this treatment modality. It is in these situations that close clinical monitoring and multidisciplinary discussion should help guide the treatment decisions.
Numerous other reports have examined the role of surgery in these patients and have made strong arguments against initial trips to the operating room in the absence of mechanical obstruction. One study evaluated nontoxic megacolon and the role of colonoscopic decompression in these patients. In their sample they had two patients with myxedema pseudovolvulus, both of whom were successfully decompressed colonoscopically (19). While this is a small sample size, it shows there are other modalities to treatment of these patients without mechanical obstructions. This can be an initial first step in management to relieve immediate symptoms. Once this is performed, patients can be managed more conservatively without need for emergent laparotomy and possible precipitation of myxedema coma. The future resection can be performed on a more elective basis, which can ultimately improve outcomes and allow for more expectant management of the patient.
Medical management with readily available medications has been shown to be successful in the treatment of hypothyroid volvulus as either an adjunct to invasive treatment or as a separate treatment modality entirely. Some early descriptions of the disease report conservative treatment with thyroid hormone replacement by mouth (4,7,20). These cases both describe complete resolution of the symptoms solely with oral medication administration. Other cases have been described in which IV T4/Levothyroxine have been used for more severely ill patients (19). This should be used in the acute phase of the patient’s presentation, along with bowel rest and IV hydration, in order to return the patient to a euthyroid state and resolve the volvulus. Other scant reports have described using IV T3 hormone replacement for the same purposes (21). Though this is an acceptable alternative, levothyroxine is more readily available and therefore can be used in these situations.
After resolution of the initial volvulus and stabilization, these patients should undergo endocrinology evaluation and should be started on oral thyroid hormone replacement therapy. The dose should be tapered while still in the hospital in order to reach a steady state in the blood and to determine on which dose the patient should be discharged to treat their underlying hypothyroidism. These patients should be counseled on the importance of adhering their prescribed medication dose and frequency in order to prevent recurrence of symptoms.
Conclusions
Myxedema pseudovolvulus is an uncommon presentation and complication of profound hypothyroidism. Despite this, a high degree of suspicion should be maintained while evaluating patients with abdominal pain and distension and a history of hypothyroidism. Questions about the hypothyroid constellation of symptoms, as well as history of thyroid surgery, should always be asked in the initial evaluation of these patients. Treatment of these patients can range from invasive laparotomy with bowel resection to bowel rest with thyroid hormone replacement. Any evaluating surgeon should be suspicious and wary of this condition while evaluation a patient with a suspected volvulus.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.29). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tachman ML, Guthrie GP Jr. Hypothyroidism: diversity of presentation. Endocr Rev 1984;5:456-65. [Crossref] [PubMed]
- Fry R, Mahmoud N, Maron D, et al. Colon and rectum. In: Townsend C Jr, Beauchamp R, Evers B, et al. editors. Sabiston textbook of surgery: The biological basis of modern surgical practice. 19th ed. Philadelphia: Elsevier, 2012:1294-80.
- Halabi WJ, Jafari MD, Kang CY, et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg 2014;259:293-301. [Crossref] [PubMed]
- Abbasi AA, Douglass RC, Bissell GW, et al. Myxedema ileus. A form of intestinal pseudo-obstruction. JAMA 1975;234:181-3. [Crossref] [PubMed]
- Patel R, Hughes RW Jr. An unusual case of myxedema megacolon with features of ischemic and pseudomembranous colitis. Mayo Clin Proc 1992;67:369-72. [Crossref] [PubMed]
- Bentley RJ, Browne RJ. Paralytic ileus and dementia in a case of myxoedema. Postgrad Med J 1969;45:779-81. [Crossref] [PubMed]
- Tran HA, Foy A. Myxedema pseudovolvulus. J Clin Endocrinol Metab 2006;91:2819-20. [Crossref] [PubMed]
- Yanamandra U, Kotwal N, Menon A, et al. Ogilvie's syndrome in a case of myxedema coma. Indian J Endocrinol Metab 2012;16:447-9. [Crossref] [PubMed]
- Khan R, Ahmed A, Tulpule S, et al. Severe Hypothyroidism-Induced Volvulus. J Clin Med Res 2015;7:995-7. [Crossref] [PubMed]
- Kumar N, Wheeler MH. Hypothyroidism presenting as acute abdomen. Postgrad Med J 1997;73:373-4. [Crossref] [PubMed]
- Nathan AW, Havard CW. Paralytic ileus and urinary retention due to hypothyroidism. Br Med J (Clin Res Ed) 1982;285:477. [Crossref] [PubMed]
- Boruchow IB, Miller LD, Fitts WT Jr. Paralytic ileus in myxedema. Arch Surg 1966;92:960-3. [Crossref] [PubMed]
- Wells I, Smith B, Hinton M. Acute ileus in myxoedema. Br Med J 1977;1:211-2. [Crossref] [PubMed]
- Goto S, Billmire DF, Grosfeld JL. Hypothyroidism impairs colonic motility and function. An experimental study in the rat. Eur J Pediatr Surg 1992;2:16-21. [Crossref] [PubMed]
- Douglass RC, Jacobson SD. Pathologic changes in adult myxedema: survey of 10 necropsies. J Clin Endocrinol Metab 1957;17:1354-64. [Crossref] [PubMed]
- Bastenie PA. Paralytic ileus in severe hypothyroidism. Lancet 1946;1:413-6. [Crossref] [PubMed]
- Solano FX Jr, Starling RC, Levey GS. Myxedema megacolon. Arch Intern Med 1985;145:231. [Crossref] [PubMed]
- Salerno N, Grey N. Myxedema pseudoobstruction. AJR Am J Roentgenol 1978;130:175-6. [Crossref] [PubMed]
- Starling JR. Treatment of nontoxic megacolon by colonoscopy. Surgery 1983;94:677-82. [PubMed]
- Hohl RD, Nixon RK. Myxedema ileus. Arch Intern Med 1965;115:145-50. [Crossref] [PubMed]
- Batalis T, Muers M, Royle GT. Treatment with intravenous triiodothyronine of colonic pseudo-obstruction caused by myxoedema. Br J Surg 1981;68:439. [Crossref] [PubMed]
Cite this article as: Schulberg SP, Meytes V, Morin N, Ferzli G, Adler E, Kopatsis A, Glinik G. Myxedema pseudovolvulus: case series and review of the literature. Ann Laparosc Endosc Surg 2017;2:56.




