
Co-existent appendicitis and cholecystitis
Introduction
Appendicitis and cholecystitis are two of the most common causes of abdominal pain, but rarely do the two disease processes present concurrently. We present a case of a healthy male, treated at our institution who presented in septic shock with the complaint of upper and lower abdominal pain on the right.
Case presentation
A 40-year-old, Hispanic male presented to the Emergency Department at our facility with the chief complaint of abdominal pain. During examination, he admitted to multiple episodes of nausea and non-bilious vomiting over the past 18 hours. His pain was described as painful along the right side of his abdomen, and most severe in the right upper and lower quadrants. The discomfort began in the mid-epigastric region, and then migrated to the lower right abdomen. He denied any past medical history, as well as any previous surgeries. He did not smoke, and he only drank alcohol occasionally.
Initial vital signs showed a temperature of 102.5 F. The patient was hypotensive and tachycardic with a BP of 92/50 mmHg. The heart rate was 115 bpm. On physical exam, he was lethargic, and had yellowed sclera. Lungs were clear to auscultation. The abdominal exam was significant for diffuse tenderness to palpation with rebound and guarding. There was exquisite tenderness to the right upper and lower quadrants, including a positive Murphy’s and Rovsing’s signs. There was mild abdominal distention noted, no previous surgical scars appreciated.
Laboratory evaluation found a WBC count that was normal at 5.1 k/µL with Hgb 16.7 g/dL, HCT 47.2% and platelets of 182 k/µL. Chemistry values were consistent with multiple episodes of vomiting and dehydration. The was potassium on 2.9 mmol/L. Liver function tests showed hyperbilirubinemia with total bilirubin of 2.7 mg/dL and direct bilirubin of 1.2 mg/dL. The transaminases were normal, however the alkaline phosphatase and GGT were elevated with levels of 178 and 67 IU/L respectively. Lactic acid was 6.9 mmol/L.
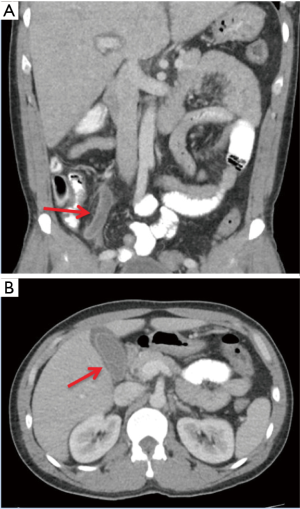
Initially, a computed tomography (CT) of the abdomen and pelvis with IV contrast was obtained. This imaging study revealed acute appendicitis with surrounding inflammatory changes (Figure 1), however, the CT also revealed diffuse gallbladder wall thickening. Biliary sonogram findings showed a diffusely thickened gallbladder wall, and moderate pericholecystic fluid, consistent with acalculous cholecystitis (Figure 1).
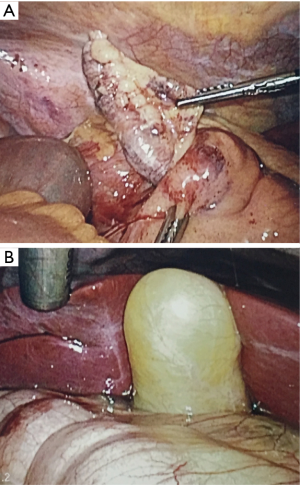
Based on these findings the patient was taken to the operating room for a laparoscopic appendectomy and possible cholecystectomy. During the procedure, a non-perforated, hyperemic and distended appendix was found, consistent with acute appendicitis (Figure 2). A laparoscopic appendectomy was subsequently performed. After removal of the appendix, attention was turned to the gallbladder. The wall of the gallbladder was edematous and distended (Figure 2). With some difficulty due to the inflamed wall, the gallbladder was successfully removed after identification of the critical view of safety.
The patient was taken to the SICU post-operatively for continued hypotension. Over the next 12 hours, the vital signs improved and the patient was downgraded from the SICU. The remaining post-operative course was uncomplicated, and the patient was discharged home on post op day 2. On follow up visit, he was found to be doing well, and had returned to normal activity.
The pathology report showed severe acute appendicitis and acute on chronic cholecystitis with mucosal congestion.
Discussion
Cholecystectomy for acute cholecystitis is the most common surgery performed in America with numbers eclipsing 500,000 annually (1). It is estimated that more than 20 million Americans have gallstones and 1–2% will become symptomatic every year (2,3). A subset of acute cholecystitis is acalculous cholecystitis, which represents 5–10% of all cases (4,5).
Appendicitis is another very common surgical malady with an estimated incidence of 233/100,000 population and is highest in the 10- to 19-year-old age group (6). Simultaneous presentation of appendicitis and cholecystitis is a very rare entity. The true incidence has not been described in the literature, and only a few case reports have been published to date (5). Our patient presented with these two separate, but common acute disease processes’ concurrently.
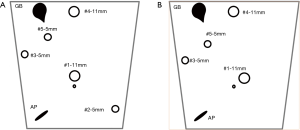
In treating these simultaneous problems, the laparoscopic approach was found to be ideal. Some surgeons are proponents of an interval cholecystectomy to reduce the risk of open conversion (5), while others performed a combined operation (7). We were able to successfully complete the combined procedure using a total of 5 ports, as detailed in Figure 3. From these ports, we were able to access both the right lower and upper quadrants efficiently and effectively. In retrospect, minor adjustments to port placement could have improved the triangulation in accessing the gallbladder. Our recommendations for altered four port placement are seen in Figure 3, and are felt to provide improved access and ease in reaching both the appendix and the gallbladder.
In conclusion, appendicitis presenting with cholecystitis is a rare phenomenon that can be safely and efficiently managed via the laparoscopic approach saving the patient a potentially more morbid procedure.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.30). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gallstones and laparoscopic cholecystectomy. NIH Consens Statement 1992;10:1-28. [PubMed]
- Thistle JL, Cleary PA, Lachin JM, et al. The natural history of cholelithiasis: the National Cooperative Gallstone Study. Ann Intern Med 1984;101:171-5. [Crossref] [PubMed]
- Friedman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol 1989;42:127-36. [Crossref] [PubMed]
- Gu MG, Kim TN, Song J, et al. Risk factors and therapeutic outcomes of acute acalculous cholecystitis. Digestion 2014;90:75-80. [Crossref] [PubMed]
- Sahebally SM, Burke JP, Nolan N, et al. Synchronous presentation of acute acalculous cholecystitis and appendicitis: a case report. J Med Case Rep 2011;5:551. [Crossref] [PubMed]
- Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132:910-25. [Crossref] [PubMed]
- Demuro JP. Simultaneous acute cholecystitis and acute appendicitis treated by a single laparoscopic operation. Case Rep Surg 2012;2012:575930.
Cite this article as: Victory J, Meytes V, Parizh D, Ferzli G, Nemr R. Co-existent appendicitis and cholecystitis. Ann Laparosc Endosc Surg 2017;2:54.


