Reduced-port surgery aided by the newly developed free jaw clip and free loop plus for local resection of gastric submucosal tumors
Introduction
Laparoscopic surgery is being applied increasingly as an alternative to conventional surgery for gastric lesions, and reports have confirmed patient safety and good outcomes (1-3). Further, outcomes comparable to those achieved by open surgery have been reported even in patients with advanced gastric cancer requiring total gastrectomy and D2 dissection (4,5). With expansion of the scope and complexity of laparoscopic surgery, there has been increased interest in the possibility of further improving cosmesis and the minimal invasiveness. Thus, single-port surgery (SPS) and reduced-port surgery (RPS) techniques have been developed, techniques that further reduce the size of the wound. SPS and RPS were first applied to cholecystectomy (6,7) and appendectomy (8,9), these procedures are now widely performed, and applications of RPS and SPS have been expanded to the treatment of malignant tumors, such as colorectal cancer (10,11). Gastric cancer requiring lymph node dissection is not often approached laparoscopically because of the surgical difficulty (12,13). However, in cases of gastric submucosal tumor, such as gastrointestinal stromal tumor (GIST), lymph node dissection is not usually necessary. Local resection is generally sufficient, and GIST, then, is a good indication for RPS (14,15). We describe RPS performed through two ports—one in the umbilicus and one in the left epigastric region. Two devices have been developed for this procedure: the free jaw (FJ) clip, which is used to grasp organs in the abdominal cavity, and the free loop plus, which is used pull suture threads from inside the abdominal cavity to outside the body. Herein, the new devices and their use in RPS for GIST are described in detail.
Device development, specifications, and characteristics
The FJ clip and free loop plus were both developed in collaboration with Charmant Inc., which is located in Sabae city, Fukui Prefecture, Japan. Sabae city is home to the manufacture of 95% of eyeglass frames sold in Japan and of many eyeglass frames that are exported. One of the Sabae city eyewear manufacturers, Charmant Inc., is an enterprise capable of executing upwards of 200 manufacturing processes, and the company now also excels in the development of microsurgery devices.
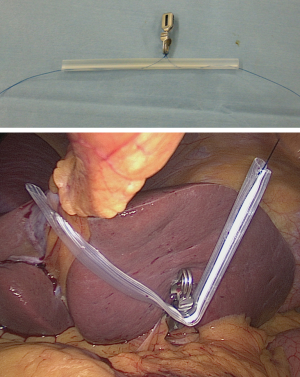
FJ clip
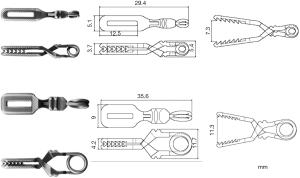
The FJ clip is available in two sizes, one for use in a 5-mm port and the other for use in a 12-mm port. Both clips are made of stainless steel (SUS 304, SUS 304 WPB), and they can be easily maneuvered with commonly-used laparoscopy forceps. The FJ clips are 29.4 and 35.6 mm in length, respectively. Because they are short, they are very practical for organ elevation.
The FJ clip has undergone repeated trial manufacture and has been tested experimentally on animal organs. The clips have a powerful grasping force (200±20 and 300±30 gf, respectively) but cause no or only negligible organ damage. The jaw surface is textured in a lattice-like relief to resist slippage. Regulatory approval was granted in Japan, and the FJ clip is now in clinical use (Figure 1).
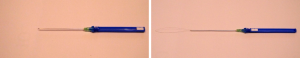
Free loop plus
The free loop plus is a device used to puncture the abdominal wall and pull suture threads from inside the abdominal cavity to outside the body. It is fitted with a φ 0.1-mm NiTi alloy suture thread that has been passed through a 90-mm 21 G stainless steel needle. Generally, the device is attached to the FJ clip and used to guide the traction suture to outside the body. Because the needle is of relatively small gauge, the risk of bleeding during puncture is low, and puncture can be repeated if the initial site proves to be unsuitable (Figure 2).
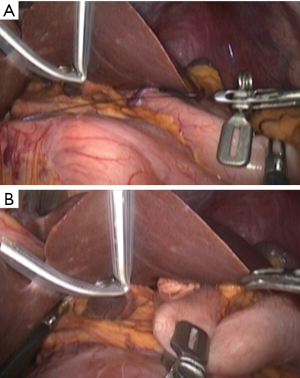
RPS for GIST-procedure
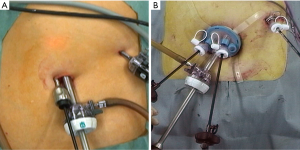
Surgery is performed with the patient in the supine position and legs spread apart. The surgeon stands between the patient’s legs, and the assistant stands to the left of the patient. A longitudinal incision, measuring approximately 1.5–2 cm, is made below the central depression of the umbilicus, and both ends of the central fascial defect are then grasped with Kocher forceps. An insufflation needle is inserted, and the abdomen is insufflated with CO2 gas. An XCEL trocar (Ethicon, Inc., Pittsburg, PA, USA), 100 mm in length and 12 mm in diameter, is inserted under optical viewing. A 10-mm oblique-viewing endoscope is inserted, and a 6-mm diameter, 65-mm long TERNAMIAN EndoTIP cannula (Karl Storz GmbH & Co., Tuttlingen, Germany) is inserted to the left of the umbilicus under endoscopic observation. The EndoTIP cannula is inserted slowly by rotating it and without cutting the fascia, so there is no leakage of CO2 gas. A single trocar—appropriately sized for the patient—is then inserted into the left epigastric region. If the tumor is ≥3 cm, the umbilical port incision must be extended 3–4 cm, and an x-Gate (Sumitomo Bakelite Co., Ltd., Tokyo, Japan) multi-channel port attached to allow for extraction of the surgical specimen (Figure 3A,B).
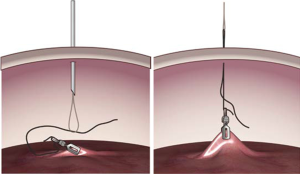
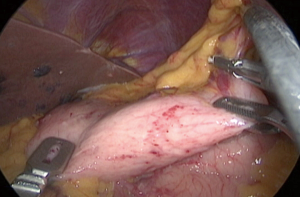
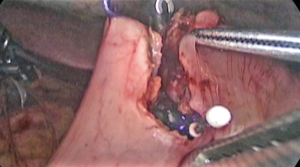
The FJ clip is used to lift tissue. A suture thread is tied to the butt end of the clip before the clip is inserted into the peritoneal cavity. Puncture is performed with free loop plus, and the traction suture, which is attached to the FJ clip, is slipped into the NiTi alloy thread loop in the abdominal cavity and withdrawn extracorporeally (Figure 4). Laparoscopy forceps (5 mm in diameter) are used to hold the forceps actuator in an oblique to horizontal direction, the forceps tip is opened, and the organ is grasped (Figure 5). If retraction of the left hepatic lobe is required, a 2-0 nylon suture thread is tied to the 12-mm FJ clip and passed through a 6-mm Penrose drain in preparation for the procedure. The FJ clip is used to grasp the tissues surrounding the diaphragmatic crus, and both ends of the suture are pulled out of the body, allowing the necessary retraction (Figure 6). The 12-mm FJ clip is used to grasp and apply traction to the gastric wall or to apply traction to the anterior wall of the gastric corpus (Figure 7A,B). Because the FJ clip is readily grasped and removed with laparoscopy forceps, the jaw can be easily repositioned as needed for the surgery (Figure 8). In patients undergoing laparoscopy and endoscopy cooperative surgery (16,17), an appropriate number of 5-mm FJ clips can be used to elevate the peritumoral tissues, achieve local stability, and perform the necessary peritumoral tissue dissection under oral endoscopic guidance that applied the techniques of endoscopic submucosal dissection (ESD) (Figure 9). The surgical defect is closed temporarily before final closure with a suture instrument. Suturing is facilitated by using the FJ clip to pull the tissue on the left and right and thus achieve countertraction during closure of the gastric wall. Immobilization of the root end of the jaw of the suturing instrument is useful when such an instrument is used together with an FJ clip. Depending on the patient, the gastric wall is sometimes closed with hand-sewn sutures under laparoscopic guidance, but even in these cases, the FJ clip is used to grasp both ends of the tissue for closure and to apply countertraction, facilitating the suturing. The FJ clip effectively grasps and applies traction to the gastric wall (Figure 10A,B). It does not dislodge, nor does the jaw injure the tissue.


Results to date
We have performed this surgery in 11 cases of gastric GIST. The patients were 5 men and 6 women who ranged in age from 50 to 79 years (mean, 64.5 years), and the surgeries were performed between September 2014 and August 2016. Case details are shown in Table 1. Mean operation time was 156 minutes (78–287 minutes). The blood loss volume was ≤30 g per patient, and the volume was so low in 8 patients that it could not be measured. In all 11 patients, the surgery was performed via two ports, one in the umbilicus and the other in the left epigastric region. Laparoscopic and endoscopic cooperative surgery was performed in 4 of the 11 patients. There were no intraoperative or postoperative complications, and the mean postoperative hospital stay was 9.9 days (range, 8–11 days). All surgeries were completed with two incisions: one at the umbilicus and one on the left side of the abdomen; no additional port was necessary (Figure 11).
Table 1
| Patient | Age (years) | Sex | Operation time (minutes) | Blood loss volume (g) | Post-operative stay (days) |
|---|---|---|---|---|---|
| 1 | 75 | Male | 81 | Negligible | 11 |
| 2 | 76 | Female | 215 | Negligible | 10 |
| 3 | 74 | Male | 237 | 3.4 | 10 |
| 4 | 45 | Female | 78 | Negligible | 9 |
| 5 | 44 | Male | 229 | 17.2 | 8 |
| 6 | 53 | Male | 156 | Negligible | 11 |
| 7 | 71 | Female | 180 | Negligible | 11 |
| 8 | 72 | Female | 115 | Negligible | 10 |
| 9 | 71 | Male | 144 | 30 | 10 |
| 10 | 50 | Female | 207 | Negligible | 11 |
| 11 | 79 | Female | 79 | Negligible | 8 |
Note that complications were not encountered in any patient. Negligible: amount too small to be measured. GIST, gastrointestinal stromal tumor; FJ, free jaw.

Discussion
Laparoscopic surgery has become widespread, and the procedures and instrumentation continue to advance. SPS and RPS are two examples of this advancement. SPS and RPS are now used for the treatment of many conditions (18,19). Laparoscopic instruments, such as the forceps and cameras used, continue to be made smaller, with high-performance small-diameter devices becoming available. Needlescopic surgery is now possible (20,21), further expanding the concept of RPS. Needlescopic surgery combined with RPS is being performed with increasing frequency, for colectomy, for example (21,22). RPS has been made possible by the use of non-standard sized forceps, and special instruments have been developed for elevating and retracting intraabdominal organs (23).
Many of the already made devices require specially designed forceps, and costs are increased if the devices used to grasp the organs are disposable. Further, if the jaw of the forceps is long, the jaw itself will cause interference when the organs are elevated, sometimes preventing sufficient elevation. It is also not possible to insert several instruments into a 5-mm port, and ports smaller than 5 mm cannot be used together during surgery.
As noted above, the FJ clip is available in two sizes to fit through ports of two commonly used sizes (5 and 12 mm) and thus facilitate sufficient elevation. These clips are optimally short. The number of teeth and angle of the grasping portion are continuously being perfected by the manufacturer and tested in animals. The concavities and convexities of the actuator are such that it can be grasped by commonly used 5-mm forceps, so specialized forceps are not needed. The clips are also economical because they are made of stainless steel and can be reused after sterilization. In terms of practical use, we believe the clips are best suited to sites that can be grasped by standard forceps and the direct grasping of the small bowel and colonic wall should be avoided.
Dedicated devices (24) are usually used to pull the suture attached to the FJ clip out of the body, but because no skin incision is required when the free loop plus is inserted, there need not be any hesitation to perform repeat puncture. Complications are unlikely.
Conclusions
At present, we in our department perform not only laparoscopic cholecystectomy but also laparoscopic appendectomy, partial gastrectomy, colectomy, and hernia repair, and these have all contributed to the development of RPS. We believe that the FJ clip will assume the role of forceps in many laparoscopic surgery settings in fields such as obstetrics and gynecology and urology. Recently, approval of the FJ clip was obtained from the US Food and Drug Administration (FDA). Thus, going forward, we believe the FJ clip will pave the way for new developments in RPS.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chikara Kunisaki) for the series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.02.18). The series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional ethical approval and individual informed consent were waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Han JH, Lee HJ, Suh YS, et al. Laparoscopy-assisted distal gastrectomy compared to open distal gastrectomy in early gastric cancer. Dig Surg 2011;28:245-51. [Crossref] [PubMed]
- Ohtani H, Tamamori Y, Noguchi K, et al. A meta-analysis of randomized controlled trials that compared laparoscopy-assisted and open distal gastrectomy for early gastric cancer. J Gastrointest Surg 2010;14:958-64. [Crossref] [PubMed]
- Peng JS, Song H, Yang ZL, et al. Meta-analysis of laparoscopy-assisted distal gastrectomy and conventional open distal gastrectomy for early gastric cancer. Chin J Cancer 2010;29:349-54. [Crossref] [PubMed]
- Wei HB, Wei B, Qi CL, et al. Laparoscopic versus open gastrectomy with D2 lymph node dissection for gastric cancer: a meta-analysis. Surg Laparosc Endosc Percutan Tech 2011;21:383-90. [Crossref] [PubMed]
- Cai J, Wei D, Gao CF, et al. A prospective randomized study comparing open versus laparoscopy-assisted D2 radical gastrectomy in advanced gastric cancer. Dig Surg 2011;28:331-7. [Crossref] [PubMed]
- Navarra G, Pozza E, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg 1997;84:695. [Crossref] [PubMed]
- Curcillo PG 2nd, Wu AS, Podolsky ER, et al. Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc 2010;24:1854-60. [Crossref] [PubMed]
- Rehman H, Ahmed I. Technical approaches to single port/incision laparoscopic appendicectomy: a literature review. Ann R Coll Surg Engl 2011;93:508-13. [Crossref] [PubMed]
- Ostlie DJ. Single-site umbilical laparoscopic appendectomy. Semin Pediatr Surg 2011;20:196-200. [Crossref] [PubMed]
- Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg 2012;255:667-76. [Crossref] [PubMed]
- Champagne BJ, Papaconstantinou HT, Parmar SS, et al. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg 2012;255:66-9. [Crossref] [PubMed]
- Omori T, Oyama T, Akamatsu H, et al. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc 2011;25:2400-4. [Crossref] [PubMed]
- Kawamura H, Tanioka T, Funakoshi T, et al. Dual-ports laparoscopy-assisted distal gastrectomy compared with conventional laparoscopy-assisted distal gastrectomy. Surg Laparosc Endosc Percutan Tech 2011;21:429-33. [Crossref] [PubMed]
- Henckens T, Van de Putte D, Van Renterghem K, et al. Laparoendoscopic single-site gastrectomy for a gastric GIST using double-bended instruments. J Laparoendosc Adv Surg Tech A 2010;20:469-71. [Crossref] [PubMed]
- Na JU, Lee SI, Noh SM. The single incision laparoscopic intragastric wedge resection of gastric submucosal tumor. J Gastric Cancer 2011;11:225-9. [Crossref] [PubMed]
- Hiki N, Yamamoto Y, Fukunaga T, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc 2008;22:1729-35. [Crossref] [PubMed]
- Hiki N, Nunobe S, Matsuda T, et al. Laparoscopic endoscopic cooperative surgery. Dig Endosc 2015;27:197-204. [Crossref] [PubMed]
- Yasuda K, Kitano S. Single port surgery: review of the literature and our initial experience. Asian J Endosc Surg 2009;2:29-35. [Crossref]
- Romanelli JR, Roshek TB 3rd, Lynn DC, et al. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc 2010;24:1374-9. [Crossref] [PubMed]
- Tagaya N, Kubota K. Reevaluation of needlescopic surgery. Surg Endosc 2012;26:137-43. [Crossref] [PubMed]
- Hosogi H, Strassel V, Martin C, et al. Single-port versus needlescopic versus conventional laparoscopic cholecystectomy: a comparative study. Asian J Endosc Surg 2011;4:120-6. [Crossref] [PubMed]
- Bae SU, Baek SJ, Min BS, et al. Reduced-port laparoscopic surgery for a tumor-specific mesorectal excision in patients with colorectal cancer: initial experience with 20 consecutive cases. Ann Coloproctol 2015;31:16-22. [Crossref] [PubMed]
- Schlager A, Khalaileh A, Shussman N, et al. Providing more through less: current methods of retraction in SIMIS and NOTES cholecystectomy. Surg Endosc 2010;24:1542-6. [Crossref] [PubMed]
- Majid A, Fernandez-Bussy S, Kent M, et al. External fixation of proximal tracheal airway stents: a modified technique. Ann Thorac Surg 2012;93:e167-9. [Crossref] [PubMed]
Cite this article as: Fujii H, Kawakami Y, Aotake T, Yoshiba H, Doi K, Onishi R, Hirose Y. Reduced-port surgery aided by the newly developed free jaw clip and free loop plus for local resection of gastric submucosal tumors. Ann Laparosc Endosc Surg 2017;2:51.