Initial results of reduced port laparoscopic gastrectomy for gastric cancer
Introduction
Recent improvements of laparoscopic surgery enable to progress their technical maturity and their instruments. The laparoscopic surgery is indicated for the majority of the gastro-intestinal disease in their early stage of cancers. By the progress in their adaptation for the gastro-intestinal disease, we re-notice that the cosmetic superiority make the patients be happier for the life after the surgery.
The wave of single port laparoscopic surgery since 2008, we started the domestic surgical meetings of TANKO (as single port laparoscopic surgery) or reduced port laparoscopic surgery, for the safe progress of the operation and for the education. In those experiences, we focus the feasibility and the problems in reduced port gastrectomy, and reveal our trials as the initial results.
Operative procedure
In our operative procedure, as the conventional laparoscopic gastrectomy (LG), we used three 12 mm, two 5 mm trocars and Nathnson’s liver retractor. For the retraction of the resected specimens, we opened 3–4 cm at the umbilicus and covered the specimens in the tissue bag.
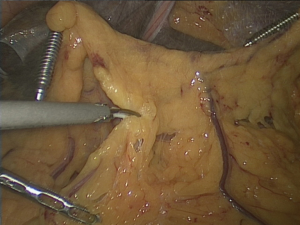
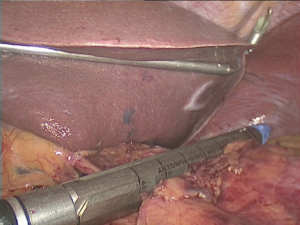
For the reduced port surgery, we placed the 4 cm wound retractor and placed 12 and 5 mm trocars in it at the opened umbilicus at the start of the surgery (Figure 1). In this procedure, we reduce one 12 and 5 mm trocars. In another four cases, we replaced one trocar of 3 mm from 5 mm. In two cases, we used EndograbTM (Virtual Ports laparoscopy system CO.: Israel) instead of the grasper for the assistant (Figure 2). For reduce the wound of liver retractor we used hanging liver retractor (EndoliftTM; Virtual Ports laparoscopy system CO.: Israel) which did not require the skin incision, in 16 cases (Figure 3).

Results
In our series, there is one case of hemostat during LG in each group. Reduced port laparoscopic gastrectomy (RPLG) from 2012 to 2014 took the same operation time and blood loss as the conventional our LG (Table 1).
Table 1
| Surgery | Number of cases | Procedure [DG(R-Y)/DG(B-1)/PG(D-T)/TG] | Median operative time (min) [range] | Median blood loss (g) [range] | Multi-channel-port device | Needle device | EndoGrabTM | EndoLiftTM |
|---|---|---|---|---|---|---|---|---|
| RPLG | 19 | 12/4/3/0 | 339 [216–544] | 50 [0–612] | 5 | 4 | 2 | 16 |
| LG | 61 | 41/10/7/3 | 377 [185–585] | 70 [0–500] | – | – | – | – |
EndoGrabTM, intra-corporeal tissue hanging device instead of grasper; EndoLiftTM, intra-corporeal liver hanging device as liver retractor; DG(R-Y), distal gastrectomy with Roux-en-Y reconstruction; DG(B-1), distal gastrectomy with Billroth-1 reconstruction; PG(D-T), proximal gastrectomy with Double-tract reconstruction; TG, total gastrectomy; RPLG, reduced port laparoscopic gastrectomy.
But the surgeon felt much stress to manipulate the tissues during the surgery.
Discussion
From the report in the meeting of 3rd Reduced Port Surgery Forum 2014 in Fukui (Figure 4), the procedures of RPLG were performed by two ways (1). The one was the using multi-channel ports device in the umbilicus. And the other way was using needle devices to reduce the ports of the surgery.
In the symposium of reduced port gastrectomy with lymphadenectomy for gastric cancer patients, the 317 RPLG cases from the five expert surgeons were reported. They include 75 of single port gastrectomy (Table 2). The results were not inferior in the bleeding, the number of resected lymph nodes, or intra- and post-operative complications than the conventional LG. One surgeon reported the much longer time in RPLG than conventional method.
Table 2
| Number | Presenter | Number of cases | Multi-channel-ports devices | Needle devices | Comparison vs. LG (bleed/operative time/number of nodes) |
|---|---|---|---|---|---|
| 1 | K. Shibao | 30 | 30 | 30 | Same/same/same |
| 2 | R. Takagawa | 126 | 126 | 0 | Same/longer/same |
| 3 | T. Urushihara | 77 | 77 | 0 | Same/same/– |
| 4 | N. Inaki | 39 | 39 | 39 | Same/same/same |
| 5 | K. Omori | 45 | 45 | 0 | Same/same/same |
| Number of total cases | 317 | 317 | 69 |
RPLG, reduced port laparoscopic gastresctomy; LG, laparoscopic gastrectomy.
All speakers reviled the better cosmetic result than the conventional method, as the feasible procedure for the skilled surgeons in spite of the difficulty of the procedures.
In our series, same results were revealed even in the small number of the cases. We also used multi-channel device at the umbilicus and needle devices in addition to the hanging devices into the peritoneal cavity to reduce the surgical port.
The most important point in the reduced port surgery is the quality control as the results of the surgery. However, the approach to reduce the trocar in the setting of the surgery makes reduce the cosmetic and psychological invasion for the patients. The principle of the surgery is to save the patient from the disease, so we must never reduce the quality of the surgery in any procedures.
From the results of reported cases and our series, the gastrectomy with lymphadenectomy was performed safely as the conventional LG. But there are some important matters on this results that are the immature data by small number of series and short observed period. Moreover, the procedures will not be indicated commonly, because the procedures were performed by the skilled surgeons and the teams. To indicate RPLG for much wider institute, we have to plan to educate the procedures as the conventional laparoscopic surgery as the one of the advanced course of procedures.
Through these processes, recent presentations could show the skilled team and would initialize the RPLG safely. However, the feasibility will be improved with the time course. By the improved skills and the instruments, we have to point out the current problems to proceed the RPLG procedures.
Recent publications about RPLG also revealed the results of retrospective studies that there was no significant difference between RPLG and conventional LG in operating time, blood loss, number of nodes dissected, morbidity, or hospital stay. All of those are from expert surgeons (2-8). But the part of them might have some sample bias, for example, obesity of the patients (5). The indication for RPLG would be suitable for not obese patients in the current results.
There are three problems for the reduced port surgery. The first is the suitable instruments and their innovation. The second is technical difficulty for the operation itself. And the third is the education for the surgical skills. The third problem is the most important for this field. So, we had the surgical meetings of reduced port surgery for the improvement, the skills, devices, and the education. The problem might be solved by the standardized procedure of the laparoscopic surgery with the reduced port settings.
Conclusions
Reduced port surgery is the one of the desirable progressions in the laparoscopic surgery. We have to progress and indicate it with safe for the future patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Chikara Kunisaki) for the series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.01.11). The series “Advancement of Single-port, Reduced-port Laparoscopic Gastrectomy for Gastric Cancer” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Iida A, Fujii H. 3rd Reduced Port Surgery Forum 2014 in Fukui. Available online: http://www2.convention.co.jp/rps2014/
- Kunisaki C, Makino H, Yamaguchi N, et al. Surgical advantages of reduced-port laparoscopic gastrectomy in gastric cancer. Surg Endosc 2016;30:5520-8. [Crossref] [PubMed]
- Seo HS, Lee HH. Is the 5-ports approach necessary in laparoscopic gastrectomy? Feasibility of reduced-port totally laparoscopic gastrectomy for the treatment of gastric cancer: A Prospective Cohort Study. Int J Surg 2016;29:118-22. [Crossref] [PubMed]
- Jeong O, Park YK, Ryu SY. Early experience of duet laparoscopic distal gastrectomy (duet-LDG) using three abdominal ports for gastric carcinoma: surgical technique and comparison with conventional laparoscopic distal gastrectomy. Surg Endosc 2016;30:3559-66. [Crossref] [PubMed]
- Kim SM, Ha MH, Seo JE, et al. Comparison of single-port and reduced-port totally laparoscopic distal gastrectomy for patients with early gastric cancer. Surg Endosc 2016;30:3950-7. [Crossref] [PubMed]
- Shibao K, Matayoshi N, Sato N, et al. Reduced Port Distal Gastrectomy With a Multichannel Port Plus One Puncture (POP). Surg Technol Int 2015;26:92-9. [PubMed]
- Inaki N. Reduced port laparoscopic gastrectomy: a review, techniques, and perspective. Asian J Endosc Surg 2015;8:1-10. [Crossref] [PubMed]
- Usui S, Tashiro M, Haruki S, et al. Triple-incision laparoscopic distal gastrectomy for the resection of gastric cancer: comparison with conventional laparoscopy-assisted distal gastrectomy. Asian J Endosc Surg 2014;7:197-205. [Crossref] [PubMed]
Cite this article as: Iida A, Goi T, Fujimoto D, Hirono Y, Nishino T, Yokoi S, Watanabe T, Togawa T, Kimura T, Fujii H. Initial results of reduced port laparoscopic gastrectomy for gastric cancer. Ann Laparosc Endosc Surg 2017;2:16.