
High ligation of inferior mesenteric artery in laparoscopic resection of rectal cancer: is it safe or dangerous?
Nowadays anterior resection and abdominoperineal excision for rectal cancer have been well standardized in laparoscopic approach. But there are still arguments about the level of the ligation of the inferior mesenteric artery (IMA) (1). Some surgeons tie the IMA at its origin from the aorta (high ligation). Others tie the IMA below the origin of the left colic artery (LCA) (low ligation). It is not clear if there is different incidence rate of anastomotic leakage and survival period between these two different levels of ligation of the IMA after radical resection of rectal cancer.
As everyone knows, the colon has two main sources of blood supply: the superior mesenteric artery (SMA) and the IMA. The main branches of the SMA include the ileocolic artery (ICA), the right colic artery (RCA) and the middle colic artery (MCA), which supplies the cecum, the ascending colon, and the transverse colon. The main branches of IMA include LCA, the sigmoid artery (SA) and the superior rectal artery (SRA), which supply the descending colon, the sigmoid colon and the up-half rectum.
In laparoscopic resection of rectal cancer, high ligation of the IMA appears easier to achieve than low ligation. The other advantage of high ligation is to reduce the tension of anastomosis (2). In theory, the descending colon ischemia and necrosis will not happen after high ligation of IMA in anterior resection for rectal cancer because there are some arterial arches between the MCA from the SMA and the LCA from the IMA. But is high ligation of the IMA really safe?
It is usually considered that there are two arterial arches between the MCA and the LCA, which maximally keep the blood supply for the descending colon after high ligation of the IMA. One is the marginal arterial arch, also known as the artery of Drummond. The other is Riolan’s arch.
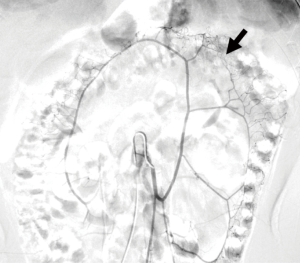
The artery of Drummond (Figure 1) is composed of arterial branches which supply the colon and runs in the mesentery close to the colon as part of the vascular arcade that connects the SMA and IMA. It is named by Hamilton Drummond [1882–1925], an English physician. But because of congenital developmental defects, the artery of Drummond is perhaps incomplete especially at the splenic flexure of colon, where is the site of watershed anastomosis of midgut and hindgut in the embryonic stage of development. This point is also called Griffiths’ point (3). At the Griffiths’ point, the anastomosis of the artery of Drummond may be substantial, tenuous, or absent (Figure 2). Angiographic studies show that anastomosis at Griffiths point is present in 48%, poor or tenuous in 9%, and absent in 43% (3). It means that the proportion of poor development of the artery of Drummond at the Griffiths’ point reaches as high as 50%. This has relevance in radiology, as it explains why the splenic flexure watershed site is the most common location for ischaemic colitis.

Riolan’s arch represents an important collateral circulation between the SMA and the IMA upon which the descending colon may be dependent. But the definition of Riolan’s arch, which named by Jean Riolan [1580–1657], a famous 17th century French anatomist, is deliberately vague. In general, Riolan’s arch refers to a distinguishing anatomical entity connecting the MCA with the LCA, additional to the artery of Drummond (Figure 3) (4). There are also many other interpretations and synonyms of Riolan’s arch (Table 1). The rate of emergence of Riolan’s arch is very different because of the difference of definition, race, research method and sample size in different reports. A book edited by the Chinese Society for Anatomical Sciences reports that the incidence rate of Riolan’s arch is 6.19%±1.13% in Chinese people. It illustrates that Riolan’s arch is usually in the state of no or only having a little blood flow. Some authors even think that the incidence of Riolan’s arch means there is severe stenosis in the SMA or IMA.
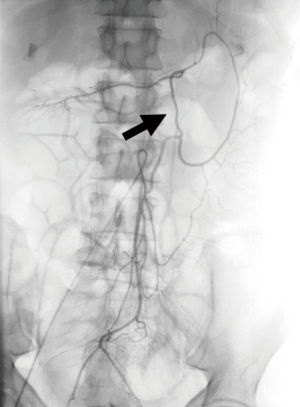
Table 1
| Central anastomotic artery of colon |
| Mesomesenteric artery |
| Middle-left colic collateral |
| Intermesenteric artery or arcade |
| Meandering mesenteric artery |
| Anastomosis (magna) of Riolan |
| Meandering artery of Riolan |
| Great colic artery of Riolan |
| Arch of Treves |
| Artery of Moskovitch |
| Artery of Gonzalez |
| Anastomosis maxima of Haller |
| Arcus magnus mesentericus |
Some reports show that the descending colon ischemia or necrosis will happen after high ligation of the IMA. Tsujinaka et al. (5) observed that 6 out of 302 patients (2.0%) with high ligation of the IMA developed proximal colon necrosis, which were confirmed by secondary surgery. Of these 6 patients, 2 died from associated complications. The results, which are obtained from the univariate analysis showed that advanced age, cerebrovascular disease, and hypertension were significantly associated with colon necrosis. In another report (6), 1,201 patients with sigmoid colon or rectal cancer who underwent high ligation of IMA were analyzed. Ten patients (0.83%) diagnosed postoperative colonic ischemia. Mortality was 10%. The symptoms of postoperative colonic ischemia occurred on the 5th day (range, 2nd–10th day) after operation. Over all, both the artery of Drummond and Riolan’s arch may not provide reliable blood supply to the descending colon after high ligation of IMA. But there were different opinions. Boström et al. (7) reported that symptomatic anastomotic leakage occurred in 12.3% (41/334) of patients in the high ligation group and in 10.6% (41/388) in the low ligation group. There was no statistical difference between two groups and high ligation was not independently associated with a higher risk of anastomotic leakage.
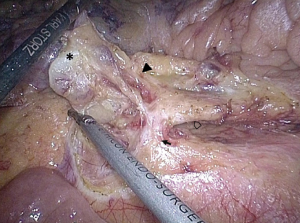
In conclusion, despite the controversy, the descending colon ischemia and necrosis after high ligation of IMA in anterior resection for rectal cancer should be pay great attention because of the existence of the Griffiths’ point and the low incidence rate of Riolan’s arch, especially for the patients with advanced age, cerebrovascular disease, and hypertension. Low ligation of the IMA with dissection the lymph nodes at the root of the IMA (Figures 4,5) perhaps is another choice. But that issue requires further study.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.10.12). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guraya SY. Optimum level of inferior mesenteric artery ligation for the left-sided colorectal cancer. Systematic review for high and low ligation continuum. Saudi Med J 2016;37:731-6. [Crossref] [PubMed]
- Bonnet S, Berger A, Hentati N, et al. High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum 2012;55:515-21. [Crossref] [PubMed]
- Meyers MA. Griffiths' point: critical anastomosis at the splenic flexure. Significance in ischemia of the colon. AJR Am J Roentgenol 1976;126:77-94. [Crossref] [PubMed]
- Lange JF, Komen N, Akkerman G, et al. Riolan's arch: confusing, misnomer, and obsolete. A literature survey of the connection(s) between the superior and inferior mesenteric arteries. Am J Surg 2007;193:742-8. [Crossref] [PubMed]
- Tsujinaka S, Kawamura YJ, Tan KY, et al. Proximal bowel necrosis after high ligation of the inferior mesenteric artery in colorectal surgery. Scand J Surg 2012;101:21-5. [Crossref] [PubMed]
- Park MG, Hur H, Min BS, et al. Colonic ischemia following surgery for sigmoid colon and rectal cancer: a study of 10 cases and a review of the literature. Int J Colorectal Dis 2012;27:671-5. [Crossref] [PubMed]
- Boström P, Haapamäki MM, Matthiessen P, et al. High arterial ligation and risk of anastomotic leakage in anterior resection for rectal cancer in patients with increased cardiovascular risk. Colorectal Dis 2015;17:1018-27. [Crossref] [PubMed]
- Li A. A 63-year-old male patient with rectal cancer who underwent anterior resection. Asvide 2016;3:495. Available online: http://www.asvide.com/articles/1270
Cite this article as: Li A. High ligation of inferior mesenteric artery in laparoscopic resection of rectal cancer: is it safe or dangerous? Ann Laparosc Endosc Surg 2016;1:49.


