Technical tips of laparoscopic linear-stapled esophagojejunostomy (overlap method)
Introduction
Laparoscopic esophagojejunostomy is one of the most technically difficult aspects when expanding institutional indication from distal to total gastrectomy. Presently, either circular stapler or linear stapler is utilized for this anastomosis according to surgeons’ choice or situation. Both devices have their pros and cons, thus above all surgeons should fully understand their characteristics in clinical use. Laparoscopic side-to-side esophagojejunostomy, called as overlap method, was first developed by Prof. Inaba in Japan (1). In this chapter, a standardized procedure in our institution to perform overlap method is described (Figure 1).
Expected advantages of linear-stapled overlap method
Generally, operative field around the esophageal hiatus for esophagojejunostomy is deep and allows only small space. When performing laparoscopic esophagojejunostomy, assurance of nice visibility is an indispensable factor. One crucial issue is size of devices. The diameter of linear stapler’s shaft is 12 mm designed to pass through the common trocar, which is much smaller than that of circular stapler. As a result, better view can be obtained during handling the device in the peritoneal cavity. This advantage will be more enhanced when attempting to perform esophagojejunostomy in the lower mediastinal space after high level resection of the esophagus. Apart from this point, linear stapler can be applicable regardless of diameter of the esophagus or the jejunum. In circular stapler, sometimes insertion of anvil head or main body is difficult when operating small-sized patients. In terms of postoperative outcomes, it is generally pointed out that incidence of anastomotic stricture is quite rare (1,2).
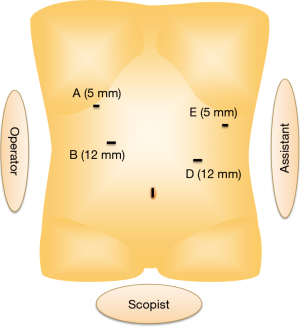
Position of the port placement
Patient is placed in supine position with legs apart and head-up tilted. Standard port setting for total gastrectomy or proximal gastrectomy (followed by double-tract reconstruction) is shown in Figure 2. First operator stands at the right side of the patient. A flexible laparoscope (2- or 3-dimentional) with high imaging resolution is used. Lateral segment of the liver is retracted using 11 cm-long Penrose drain. Center of the drain is fixed to the anterior part of the esophageal hiatus, and each end is retracted to the abdominal wall by attached threads.
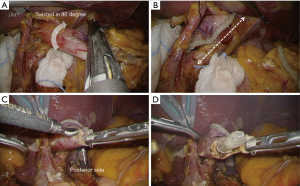
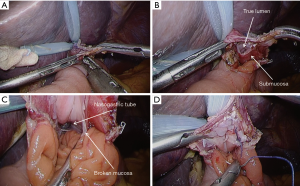
Division of the esophagus (Figure 3)

After all of the steps for lymph node dissection and mobilization, the abdominal esophagus is exposed. It is quite important not to cause either direct or thermal injury to the esophageal wall, aiming secure subsequent anastomosis. If the esophageal invasion from the tumor is recognized, retraction with a use of a cotton tape encircling the esophagus is effective. Usually, the esophagus is divided at the level just above the esophagogastric junction, however if esophageal invasion exists, intraoperative peroral gastroendoscopy is carried out to determine a proper resection line. Finally, the abdominal esophagus is twisted in 90 degree clockwise, and division is completed with a 60 mm linear stapler (Figure 4A), which is introduced from port B (shown in Figure 2). With this, stapling line of the esophageal stump resulted in vertical direction (anterior-posterior direction) (Figure 4B).
Preparation of the jejunal limb
In linear-stapled esophagojejunostomy, tension-free jejunal limb is essential to avoid embarrassing complications, such as injury of the intestinal wall. Creation of the jejunal limb is basically performed through mini-laparotomy, which is made by expansion of the umbilical port wound. Before making the mini-laparotomy, the jejunum, 20 cm distal from the Treitz ligament, is grasped by forceps by assistant surgeon under laparoscopic view to be kept with confirmation of the peristaltic direction. After making mini-laparotomy and placing a wound retractor, the grasped jejunum is extracted outside through it. After verifying vessels’ structure in the mesentery, the jejunum is divided using a linear stapler, usually approximately 20 cm distal from the Treitz ligament. The marginal vessel is basically divided, and if there is still strong tension so far, a branch of jejunal artery and vein is divided after clamping test using a temporary vessel clamper. The length of jejunal limb is designed as 40 cm. Jejunojejunostomy is done by side to side fashion using a 60 mm linear stapler, and the entry hole is closed by manual suturing in full-thickness layer. Mesentery gap resulted from jejunojejunostomy is also closed by hand suturing. Lastly, a small entry hole for stapler insertion for subsequent esophagojejunostomy is made at the end of the jejunal limb. Because decision of this position under laparoscopy is sometimes difficult, it is routinely done under direct vision with measuring the accurate distance and stretching the intestine.
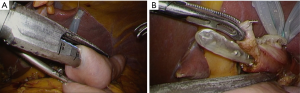
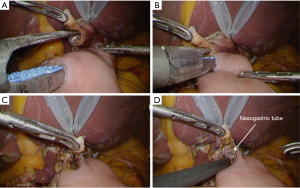
Esophagojejunal stapling (Figure 3)
After re-establishment of the pneumoperitoneum, a small hole is made at the posterior edge of the esophageal stump using high-frequency electrocautery with a guidance of nasogastric tube (Figure 4C,D). This hole should be ideally as small as possible, just allowing passage of the tube. The semi-separated staple line should be left as attached to the esophagus, because this part can be useful for retracting the esophagus during the anastomosis. Next, mobilization of the esophageal stump is examined. At least 45 mm length of the free wall should be ensured at the posterior site for subsequent stapling. The created jejunal limb is brought up to the upper abdomen basically via ante-colic route. If the tension seems tight because of a large amount of visceral adipose tissue, retro-colic route is chosen. The linear stapler is introduced from port B (as shown in Figure 2), and the cartridge site is inserted to the jejunal limb (Figure 5A). Then, the stapler is moved to an expected position for anastomosis as a simulation (Figure 5B). The operator grasps the semi-separated staple line of the esophageal stump to pull towards caudal. The stapler is moved to the posterior site of the esophagus, to insert the anvil folk into the esophageal lumen with a guidance of the nasogastric tube (Figure 6A). The stapler is clamped at the posterior wall of the esophagus. This clamping should be done several times, to make sure no step between the esophagus and the jejunum at the lateral side (Figure 6B). Firing of the stapler is usually employed by motor-driven systems to more accurately stabilize the stapler during handling. After firing, the stapler is gently removed, then hemorrhage from the intraluminal staple line is checked (Figure 6C). If bleeding is recognized, it can be controlled by soft coagulation using suction device with a metal tip. Finally, the nasogastric tube is passed through the anastomosis to check patency (Figure 6D).
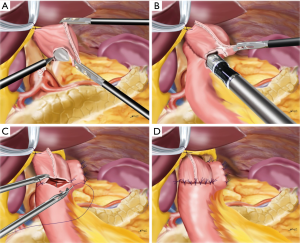
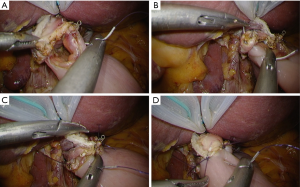
Closure of the entry hole (Figure 3)
It can be done either by interrupted or continuous suturing (normal or barbed suture). Likewise, knot-tying can be done either by intra or extracorporeal fashion according to surgeons’ preference. The author prefers interrupted suture with intracorporeal knot-tying technique using 3-0 absorbable monofilament thread, 12 cm in length. First, the left side edge of the entry hole is closed (Figure 7A), then the right side is done (Figure 7B). Next, the center of the entry hole is closed by another stitch (Figure 7C), paying attention that the mucosa is hidden inside. After these three fundamental stay sutures, spaces between these sutures are closed by additional sutures (Figure 7D), usually requiring 7–13 stitches in total. It is quite important to accurately stich in full-thickness layer, particularly at the esophageal wall side. After completion of the closure, the nasogastric tube is introduced 3–4 cm distally passing the anastomosis, to conduct air-leakage test to confirm tightness of the anastomosis (Figure 8).
Prevention of internal hernia or torsion (Figure 3)
The jejunal limb is flipped to the left side of the patient, and the transverse colon is lifted up cephalad to expose Petersen’s defect. The assistant holds both jejunal and colon mesentery at the peripheral side close to the intestine, which will be a termination point for the subsequent continuous suture. As a suture material, a barbed non-absorbable thread is used for time saving, and suturing is started from the central portion of the Petersen’s defect (Figure 9A). In order to prevent torsion of the jejunal limb, it is fixed at several points. The jejunal stump is fixed to the left diaphragmatic crus (Figure 9B), and outlet intestine distally is fixed to either hepatoduodenal ligament (Figure 9C) or fat tissue around the gallbladder, which depends on each situation. A 19 Fr Blake-type drainage tube is introduced from port A (shown in Figure 2), and its tip is placed behind the anastomotic site.
Postoperative management
According to our clinical pathway, water-drinking is started on 1st day and soft meal is initiated on 3rd day after surgery. The drainage tube is removed on 3rd or 4th day, if there is no unfavorable change at its contents. Patients discharge the hospital 7th–9th day, if without any complication.
Pitfalls and management for difficult situation
Involvement of a nasogastric tube in stapling
This is one of the most well-known pitfalls of this procedure, usually happens at the beginning phase. To prevent this, close communication and careful confirmation with anesthesiologists is mandatory. For recovery, if re-anastomosis seems difficult, removal of the tube using scissors may be an alternative as a compromise procedure, expecting that remaining pieces will naturally drop down.
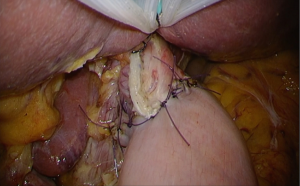
Migration of the anvil folk to the submucosal layer (Figure 10)
To avoid this complication, guidance by the nasogastric tube is the most effective. Full-thickness stiches to the esophageal wall would be also an effective measure for prevention. According to the author’s experience, if it happens, mucosal layer can be cut to create a true lumen, then mucosa should be sutured to the staple line to re-make it as normal situation (Figure 11).
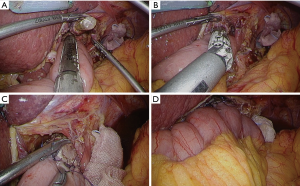
Anastomosis after high-level resection of the esophagus (Figures 12,13)

Anastomosis in the lower mediastinal space is the most difficult scene even for this procedure. In such a situation, ensuring wider operative field with better visibility is the most important things. The diaphragmatic crus should be divided at its right, left or anterior portion using energy device to widen the esophageal hiatus as possible. When performing high anastomosis, articulating function of the linear stapler is very useful to adjust the inserting axis to the esophageal lumen.
Acknowledgments
The author received honorarium for lectures from Johnson & Johnson and Medtronic.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.19). The author serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from May 2016 to Apr 2018. The author received honorarium for lectures from Johnson & Johnson and Medtronic.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Inaba K, Satoh S, Ishida Y, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 2010;211:e25-9. [Crossref] [PubMed]
- Nagai E, Ohuchida K, Nakata K, et al. Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery 2013;153:732-8. [Crossref] [PubMed]
- Kinoshita T. Typical case of laparoscopic esophagojejunostomy using overlap method.Asvide 2016;3:492. Available online: http://www.asvide.com/articles/1267
- Kinoshita T. Migration of the anvil folk to the submucosal layer with a repair for it during laparoscopic overlap esophagojejunostomy. Asvide 2016;3:493. Available online: http://www.asvide.com/articles/1268
- Kinoshita T. Laparoscopic overlap esophagojejunostomy after high-level resection of the esophagus. Asvide 2016;3:494. Available online: http://www.asvide.com/articles/1269
Cite this article as: Kinoshita T. Technical tips of laparoscopic linear-stapled esophagojejunostomy (overlap method). Ann Laparosc Endosc Surg 2016;1:48.