Transperineal extralevator abdominoperineal excision performed by double laparoscopic approach with no position change
Introduction
Conventional abdominoperineal excision (APE) for low rectal cancer is associated with higher rates of circumferential resection margin (CRM) involvement (1), intraoperative tumour perforation (IOP) and local recurrence and leads to poorer survival when compared with anterior resection. In response to these concerns, Holm et al. (2) emphasized the importance of full removal of the pelvic floor. Extralevator abdominoperineal excision (ELAPE) or cylindrical APE aims to improve the oncological outcome through removal of increased tissue in the distal rectum and en bloc excision of the levator ani. This creates a cylindrical surgical specimen without a waist and is associated in early reports with reduced CRM involvement, IOP and local recurrence compared with conventional APE.
The technique of ELAPE has been described with the patient in the prone jackknife position and a myocutaneous flap is used to repair the plevic defect. The operation has the disadvantages of a long operation time, greater trauma, and requiring the assistance of a plastic surgeon. Laparoscopic colorectal resection is now widely established and its benefits and safety have been extensively reported (3). To simplify the operation, we have been performing ELAPE with transperineal ELAPE performed by double laparoscopic approach without a change of the position of the patient.
Patient selection and pre-operative preparation
Patients with tumours located within 5 cm of the anal verge were treated with ELAPE procedures. This decision was confirmed at a multidisciplinary team meeting after the surgeon had reviewed the patient, confirmed tumour location with MRI and discussed surgical options with the patient (ultra-low AR vs. ELAPE in those patients with a tumour at approximately 5 cm).
The patients had preoperative bowel preparation the day before surgery. Prophylactic antibiotics were administered before the incision.
Procedure (Figure 1)
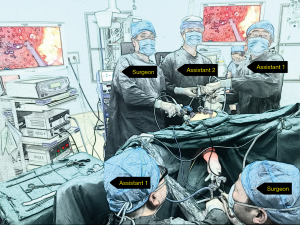
A standardized surgical procedure was performed by two experienced rectal cancer surgeons, working simultaneously throughout the whole procedure (Figure 2).
Abdominal approach
The patients were placed in the Trendelenburg and right lateral tilt position.
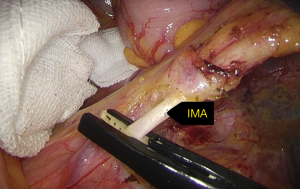
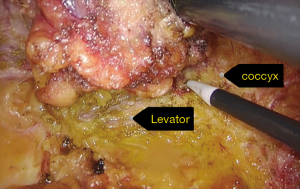
Port distribution was as follows: a 10-mm umbilical port together with a 30-degree teleangle scope inside (2D EndoEYE 10 mm video laparoscope, Olympus KeyMed), a 10-mm port at the planned right iliac fossa, two 5-mm ports inserted in each flank, and the last 10-mm port at the planned left sided colostomy site (Covidien, Mansfield, MA, USA). A high tie of the inferior mesenteric vessels (Lapro-Clip, Covidien, Mansfield, MA, USA) (Figure 3) and a complete mobilization of descending-sigmoid colon were performed. ELAPE was performed according to the description by Holm et al. (2) with the abdominal portion involving laparoscopic mobilization of the mesorectum as far down as the origin of the levator ani muscles. This level was defined laparoscopically by the neurovascular bundle laterally, the upper part of the vagina/seminal vesicles anteriorly and the coccyx posteriorly. The bowel was divided proximally, and a stoma was formed after closure of all trocar sites.
Trans-perineal approach
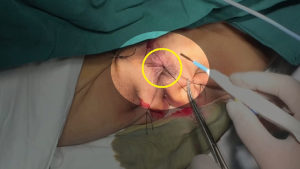
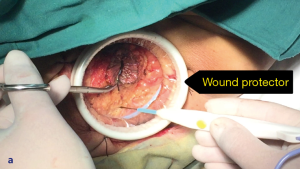
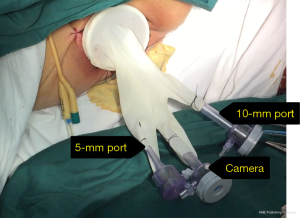
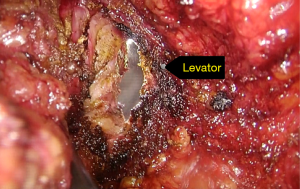
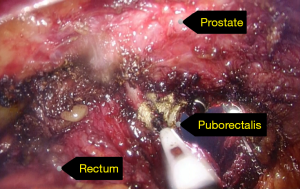
Perineal dissection consisted of dissection of the anus outside the external anal sphincter with preservation of the perianal skin and ischiorectal fat (Figures 4,5). Used a 3-port technique made by glove, the pelvic cavity was inflated with CO2 to a pressure of 7–8 mmHg (Figure 6). Dissection continued around the sphincter complex and followed the inferior surface of the levators to a point laterally where they originate from the pelvic sidewall (Figures 7,8), connected each other on the left side to the level where the abdominal dissection was terminated (Figure 9). Then amputated the puborectalis and remove the specimen by the guide of abdominal team (Figure 10).
An abdominal drain was sited in pelvic and directly closed the perineal wound in layers.
Post-operative management
All patients had CRMs >1 mm; no IOP occurred. The median length of stay was 8 days. After surgery, the planned follow up for the patient was every 3 months for the first 2 years and then every 6 months for the following 3 years.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study is approved by the institutional ethical committee of China-Japan Union Hospital of Jilin University and obtained the informed consent from every patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wibe A, Syse A, Andersen E, et al. Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum 2004;47:48-58. [Crossref] [PubMed]
- Holm T, Ljung A, Häggmark T, et al. Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 2007;94:232-8. [Crossref] [PubMed]
- Kuhry E, Schwenk WF, Gaupset R, et al. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 2008;CD003432 [PubMed]
- Xie Z, Zhang H, Cui X, et al. Transperineal extralevator abdominoperineal excision performed by double laparoscopic approach with no position change. Asvide 2016;3:491. Available online: http://www.asvide.com/articles/1266
Cite this article as: Xie Z, Zhang H, Cui X, Yu X, Fu W, Li C. Transperineal extralevator abdominoperineal excision performed by double laparoscopic approach with no position change. Ann Laparosc Endosc Surg 2016;1:47.