
Hybrid natural orifice transluminal endoscopic surgery colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors: intermediate follow up of a randomized trial
Introduction
There is now already a wealth of evidence in the literature indicating laparoscopic colectomy is associated with definite short term benefits including faster recovery, reduced postoperative pain, reduced wound infection, and faster return of bowel function and at the same time, it has comparable oncological outcomes with open colectomy (1,2). However, specimen retrieval still required a mini-laparotomy wound which is always the main cause of postoperative pain and pain or wound related complications. In 2009, we described a novel technique of laparoscopic colectomy without mini-laparotomy-known as hybrid natural orifice transluminal endoscopic surgery (NOTES) colectomy for patient suffered from left sided colonic tumors (3). It was in fact a marriage between laparoscopic and endoscopic operations, where laparoscopic colonic mobilization, transection, and colorectal anastomosis are performed intracorporeally, and the specimen is extracted transanally, without requiring mini-laparotomy. Complications related to the mini-laparotomy are therefore entirely abolished. As the preliminary results were promising, we set out to conduct a randomized trial to compare the short-term outcomes of patients who underwent hybrid NOTES colectomy (HNC) with those who underwent conventional laparoscopic colectomy (CL). The short term results from this RCT which was published in 2013 had showed that in selected group of patients, they can enjoy the full benefit of minimally invasive surgery with significant lesser wound pain as well as a lower wound infection rate (4). And this article is a follow up of previous trial, and aims to report immediate outcome between the two groups.
Methods
Between June 2009 to June 2012, 70 patients (35 patients in the HNC group and 35 patients in CL group) with left sided colonic tumor were recruited in a prospectively randomized trial to compare HNC and CL. Details on patient selection criteria, method of randomization, operative techniques, perioperative data and short-term outcomes have been reported previously (4).
Follow up protocol
All patients were followed up in our surgical clinic at 3-month intervals in the first 3 years, semi-annually in the subsequent 2 years, and then yearly afterward. Serum carcinoembryonic antigen was measured at every follow-up session in the first 5 years. Annual chest X-ray and transabdominal ultrasonography were performed to screen for recurrence until 5 years after surgery. Surveillance colonoscopy was performed 1 year after surgery and every 3 years thereafter if the first colonoscopy was normal; colonoscopy was performed more frequently if the patient’s condition indicated otherwise.
Main outcome measures
Pathological staging, number of lymph nodes harvested and size of tumor were compared between the two groups. Patient survival and disease recurrence following curative surgery were analyzed and compared. Curative surgery was defined as no gross macroscopic tumor present clinically or radiologically at the end of surgery. Disease recurrence was defined as clinically or radiologically proven recurrence, supported by histological tissue diagnosis whenever possible. Overall survival was defined as the time from the date of surgery to the date of death or most recent follow-up.
Statistical analysis
Statistical analyses were performed with SPSS v. 13.0 (SPSS, Chicago, USA). Clinicopathologic variables were correlated using the χ2 test, Fisher’s exact test, t-test or Mann-Whitney U-test. A Kaplan-Meier survival curve was constructed and statistically significant differences in survival were identified by the log-rank test. A two-sided P value of less than 0.05 was considered significant.
Results
Characteristics of the patients and tumors were listed in Table 1. The two groups were comparable with regard to age, sex, final histopathological stage of disease and size of tumor. No significant difference between the two groups in terms of operative time, blood loss and hospital stays and major complications. Patients in HNC group experienced significantly less wound pain when compared to conventional lap colectomy group. Number of lymph nodes harvested was also comparable between the two groups (Table 2).
Table 1
| Characteristics | HNC | CL | P |
|---|---|---|---|
| Sex (M:F) | 13:22 | 12:23 | 0.806A |
| Age (years) | 62 [51–86] | 72 [49–84] | 0.828A |
| Tumor size (cm) | 2 [2–4] | 3 [2–4] | 0.104B |
A, χ2 test; B, Mann-Whitney U-test. HNC, hybrid NOTES colectomy; CL, conventional laparoscopic colectomy.
Table 2
| Variables | HNC | CL | P |
|---|---|---|---|
| Stages (I/II/III/IV) | 4/14/7/10 | 1/10/12/12 | 0.321C |
| No. of lymph nodes harvested | 12 [6–33] | 12 [6–29] | 0.06B |
B, Mann-Whitney U-test; C, Fisher’s exact test. HNC, hybrid NOTES colectomy; CL, conventional laparoscopic colectomy.
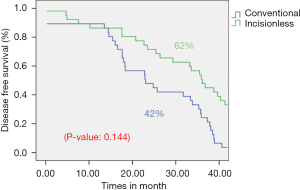
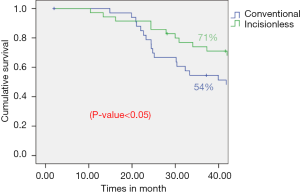
Within median follow up of 37–45 months, no statistically significant difference was observed in disease recurrence rate (conventional: 8.57%; hybrid: 5.71%; P value: 0.22) (Table 3) and 3-year disease free survival rates (conventional: 42%; hybrid: 62%; P value: 0.144) (Figure 1). While the overall 3-year survival rate is statistically shorter in the conventional group (conventional: 54%; hybrid: 71%; P value <0.05) (Figure 2).
Table 3
| Patient | Stage | Details |
|---|---|---|
| Hybrid NOTES colectomy | ||
| An 84-year-old female | Stage 2 | Diagnosed liver metastasis in post op 10 months |
| Refused further treatment | ||
| A 72-year-old female | Stage 1 | Developed anastomotic recurrence in post-op 3 months |
| Open TME performed | ||
| Conventional laparoscopic colectomy | ||
| An 83-year-old female | Stage 3 | Diagnosed anastomosis recurrence in post-op 2 yrs |
| Refused treatment and died | ||
| A 64-year-old female | Stage 2 | Diagnosed liver met in post-op 2 yrs |
| Refused treatment | ||
| A 66-year-old male | Stage 2 | Diagnosed liver met in post-op 4 yrs |
| Wedge resection performed | ||
NOTES, natural orifice transluminal endoscopic surgery.
Discussion
The technique and concept of trans-rectal natural orifice specimen extraction (trans-rectal NOSE) colectomy was first described in early 1990s, it was developed in an attempt to minimize the wound access trauma by abolishing the mini-laparotomy wound that used for specimen retrieval (5). Using trans-rectal route for extraction of colectomy specimen is a better option over other natural orifices as it is feasible for both sex and straightness of rectum also makes it relatively easy to access peritoneal cavity. To date, there were already numerous literature evidence indicating that NOTES colectomy are definitely associated with the presumed benefits namely less pain, lower analgesic requirement and faster recovery (4,6-8), and allowing patients to enjoy the full benefit of minimally invasive surgery. Nevertheless, one important potential clinical drawback of HNC is the need for opening up rectum in peritoneal cavity which runs the risk of peritoneal contamination and tumor seedling.
Bacterial contamination of peritoneal cavity is frequent in colorectal procedure (9). However, it was unknown whether opening rectum stump will further increase the bacterial load in the peritoneal cavity and results in clinically significant peritoneal sepsis. In our study, we would give prophylactic antibiotics during induction of anesthesia and complete one course of antibiotics post operatively, we would also ensure good mechanical bowel preparation so as to minimize the peritoneal soiling intra-operatively. And none of our study cases developed intra-abdominal sepsis in post-operative peroid. In 2012, Federico has conducted a study comparing the peritoneal contamination during laparoscopic sigmoidectomy with and without NOSE. And the result has showed that although a higher peritoneal contamination was found in NOSE (contamination rate of peritoneal fluid was 100% vs. 88.9% in NOSE and non-NOSE colectomy, P=0.23), but did not translate into infectious morbidity (10). Recently, there was also experimental study reporting a new device for reversible endoluminal colon occlusion (Coloshield) which can further reduce peritoneal contamination during trans-rectal NOTES procedure (11).
Second issue for NOTES colectomy is the increased risk of tumor seedling. Initial introduction of laparoscopic colectomy, there were concerns of port sites or extraction sites recurrence, later have been proved unfounded in many studies (12). We believed that as long as proper oncologic principles and specimen handling are respected, the chance of pelvic tumor seedling using trans-rectal route should not be higher than trans-abdominal route. We have adopted two important measures to prevent tumor seedling, firstly, we would use cytocidal rectal washout before opening up the rectum. Second, we would exclude the tumor proximally and distally with non-cutting endostapler or cotton tap. The transanal endoscopic operation (TEO) devices not only provide a stable platform to maintain the pneumoperitoneum for extraction of specimen, also protect the rectal stump in contact with the tumor bearing colon. And from our intermediate follow up data, no significant difference in terms of disease recurrence rate and survival rate was observed between the two groups. There were wide variations of the method of rectal protection among studies on trans-rectal NOTES colectomy; according to a recent systematic review—25% none, 33% rigid rectoscope, 42% camera sleeve or retrieval bag (13), however little is mentioned on the oncological outcomes following NOSE colectomy. So more long term studies was warranted to assess any impact of NOSE on colectomy for malignant cases.
To conclude, it is safe for us to offer hybrid colectomy for selected patients with left sided colonic cancer, without adversely affect their oncological outcome and survival, while at the same time, benefit of minimally invasive surgery can be fully expressed.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.13). Li MK serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Aug 2016 to Jul 2018. Tung KL has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by PYNEH Ethical Committee and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chung CC, Tsang WW, Kwok SY, et al. Laparoscopy and its current role in the management of colorectal disease. Colorectal Dis 2003;5:528-43. [Crossref] [PubMed]
- Chapman AE, Levitt MD, Hewett P, et al. Laparoscopic-assisted resection of colorectal malignancies: a systematic review. Ann Surg 2001;234:590-606. [Crossref] [PubMed]
- Cheung HY, Leung AL, Chung CC, et al. Endo-laparoscopic colectomy without mini-laparotomy for left-sided colonic tumors. World J Surg 2009;33:1287-91. [Crossref] [PubMed]
- Leung AL, Cheung HY, Fok BK, et al. Prospective randomized trial of hybrid NOTES colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors. World J Surg 2013;37:2678-82. [Crossref] [PubMed]
- Franklin ME Jr, Ramos R, Rosenthal D, et al. Laparoscopic colonic procedures. World J Surg 1993;17:51-6. [Crossref] [PubMed]
- Wolthuis AM, Fieuws S, Van Den Bosch A, et al. Randomized clinical trial of laparoscopic colectomy with or without natural-orifice specimen extraction. Br J Surg 2015;102:630-7. [Crossref] [PubMed]
- Xingmao Z, Haitao Z, Jianwei L, et al. Totally laparoscopic resection with natural orifice specimen extraction (NOSE) has more advantages comparing with laparoscopic-assisted resection for selected patients with sigmoid colon or rectal cancer. Int J Colorectal Dis 2014;29:1119-24. [Crossref] [PubMed]
- McKenzie S, Baek JH, Wakabayashi M, et al. Totally laparoscopic right colectomy with transvaginal specimen extraction: the authors' initial institutional experience. Surg Endosc 2010;24:2048-52. [Crossref] [PubMed]
- Saida Y, Nagao J, Nakamura Y, et al. A comparison of abdominal cavity bacterial contamination of laparoscopy and laparotomy for colorectal cancers. Dig Surg 2008;25:198-201. [Crossref] [PubMed]
- Costantino FA, Diana M, Wall J, et al. Prospective evaluation of peritoneal fluid contamination following transabdominal vs. transanal specimen extraction in laparoscopic left-sided colorectal resections. Surg Endosc 2012;26:1495-500. [Crossref] [PubMed]
- Senft JD, Carstensen B, Mischnik A, et al. Endolumenal colon occlusion reduces peritoneal contamination during a transrectal NOTES procedure: a controlled porcine survival study. Surg Endosc 2016;30:2946-50. [Crossref] [PubMed]
- Kuhry E, Schwenk WF, Gaupset R, et al. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 2008;CD003432 [PubMed]
- Wolthuis AM, de Buck van Overstraeten A, D'Hoore A. Laparoscopic natural orifice specimen extraction-colectomy: a systematic review. World J Gastroenterol 2014;20:12981-92. [Crossref] [PubMed]
Cite this article as: Tung KLM, Li MKW. Hybrid natural orifice transluminal endoscopic surgery colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors: intermediate follow up of a randomized trial. Ann Laparosc Endosc Surg 2016;1:46.


