B-II reconstruction with Braun’s anastomosis after totally laparoscopic distal gastrectomy with D2 lymph node dissection for advanced gastric cancer
Introduction
B-II reconstruction with Braun’s anastomosis after totally laparoscopic distal gastrectomy (TLDG) with D2 lymph node is a difficult but mature surgical method. It needs operator superior skills. Here we describe the technique.
Methods
Patient
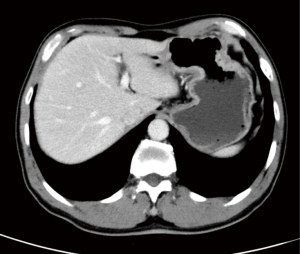
The patient is a 59-year-old man in the present video (Figure 1). He was diagnosed moderately differentiated adenocarcinoma of gastric antrum by gastroscopy and histological test and the tumor stage was assessed to be cT3N0–1M0 by CT scan preparation (Figure 2). It is suitable to perform B-II reconstruction with Braun’s anastomosis after TLDG with D2 lymph node dissection for those advanced gastric cancer patients. The study obtained the informed consent from the patient.
Surgical procedure
After general anesthesia, the patient was placed horizontal position with 20° head-up tilt. Legs were apart 30–45 degrees for the place of camera operator. The surgeon was positioned on the left side of the patient and the first assistant on the right side.
The 30° camera trocar-hole was inserted above the umbilicus using 12-mm trocar. Two trocar-holes were inserted on the left for the operator with a 12-mm trocar and a 5-mm trocar.
The other two trocar-holes then were inserted into the right with two 5-mm trocars for the first assistant.
After D2 lymph nodes dissection, duodenal transection was performed with a linear stapler. The stomach was resected by two firings of a linear stapler, and the resected specimen was placed in a plastic bag. Following these procedures, B-II reconstruction with Braun’s anastomosis was processed with endoscopic linear stapling devices. The gastrojejunostomy was performed at a point 20 cm distal to the Teritz ligament. The stomas were reconstructed on the dorsal sides of the residual stomach. And Braun anastomosis was performed 15 cm distal to the gastrojejunostomy.
Finally, the 12-mm trocar-hole above the umbilicus was extended to 4 cm around the umbilicus, the specimen was then extracted from the abdomen through the incision (Figure 3).
Results
The total length of operation was 190 min, and the entire bleeding is 40 mL. The pathology outcome after the surgery show it the moderately differentiated adenocarcinoma staging T2N0M0 with 0/34 lymph nodes positive. The patient ate liquid diet on the 3rd day and discharged from hospital with the wound class-A healing on the 7th day, without any significant complications.
Discussion
B-II is an operation in which the greater curvature of the stomach is connected to the first part of the jejunum in end-to-side anastomosis. This often follows resection of the lower part of the stomach. After the reconstruction, food goes through stomach and directly into upper jejunum. It allows to dissect more gastric tissue without the problem causing by a high level of tension at anastomosis and makes sure margin negativity, thus allowing the reconstruction after gastrectomy. However, this technique causes more dissectional and physiological changes, therefore, a higher chance of complications such as abdominal internal hernia, afferent loop obstruction, duodenal stump leakage, anastomosis and afferent loop obstruction, alkaline reflux gastritis, remnant gastric cancer (RGC), postoperative gastroparesis syndrome (2). Braun’s anastomosis can effectively diminish obstruction, twist, protrusion and edema, and allow food go through easier. Moreover, with diminishing reflux and reducing irritation to gastric mucosa at the same time, it can effectively reduce complications above (3). And we reconstructed the gastrojejunostomy on the dorsal sides of the residual stomach to form natural fold so that the regurgitation can be reduced.
Totally laparoscopic gastrectomy (TLG) (4) has been proved to be safe and effective. It has so many advantages associated with TLG. In TLG, the whole anastomotic procedure can be clearly viewed, so such tension and injuries can be obviated, especially in an obese patient (5). However, the disadvantages of TLG include that it is difficult in intraoperative localization of the tumor, and additional costs for using many linear stapler cartridges. We overcame this problem by having endoscopy before the day of the operation again in order to confirm the exact location of the tumor and we marked the location of the tumor with nano carbon on the gastric wall (6).
Conclusions
In conclusion, TLDG with intracorporeal B-II reconstruction with Braun’s anastomosis using laparoscopic linear staplers was found to be safe and feasible. We consider that our operation may represent a good choice for reconstructions after laparoscopic distal gastrectomy.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.10.13). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zang W, Liu W, Chen S, et al. Totally laparoscopic distal gastrectomy. Asvide 2016;3:448. Available online: http://www.asvide.com/articles/1221
- Kondo K, Akiyama S, Ito K, et al. Risk of Cancer Development in the Gastric Remnant by B-II Resection. In: Takahashi T. editor. Recent Advances in Management of Digestive Cancers. Tokyo: Springer-Verlag, 1993:218-20.
- Jin ZD. Application of Braun's anastomosis in Billroth II gastrectomy. Medical Journal of Chinese People's Health, 2010.
- Kanaya S, Gomi T, Momoi H, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 2002;195:284-7. [Crossref] [PubMed]
- Chen K, Mou YP, Xu XW, et al. Comparison of short-term surgical outcomes between totally laparoscopic and laparoscopic-assisted distal gastrectomy for gastric cancer: a 10-y single-center experience with meta-analysis. J Surg Res 2015;194:367-74. [Crossref] [PubMed]
- Ye L. Nanocarbon lymphatic tracer technique of minimally invasive radical surgery in patients with gastric application results. Shaanxi Medical Journal 2015;44:57-9.
Cite this article as: Zang W, Liu W, Chen S, Teng W. B-II reconstruction with Braun’s anastomosis after totally laparoscopic distal gastrectomy with D2 lymph node dissection for advanced gastric cancer. Ann Laparosc Endosc Surg 2016;1:32.