Hand-assisted laparoscopic surgery in Crohn’s disease
Introduction
In patients with Crohn’s disease (CD) who may have undergone multiple open surgeries, it is usually difficult to explore fully laparoscopic surgery again, especially if complicated by abscesses, fistulas or anastomotic leaks. Thus, there comes another alternative to laparoscopic surgery for the treatment of colorectal diseases named Hand-assisted laparoscopic surgery (HALS), which is commonly used in patients with higher surgical complexity or BMI (1,2). Several studies have reported that HALS maintains the advantages of laparoscopic surgery and has no differences compared with full laparoscopic surgery in the aspects such as duration of operation, pain, time for recovery, and hospital stays (3-7). The application of HALS in colectomy allows surgeons to have tactile feedback and manual assistance, and make the treatment of large inflammatory phlegmons or fibrotic masses easier, such as those associated with diverticulitis or CD (8,9). Similarly, the hostile abdomen with numerous adhesions or complex fistula may be more efficiently sorted out with a hand in the peritoneal cavity. This technique may broaden the application of minimally invasive colectomy (10).
Preparation
Firstly, the patient is in supine position, then straps or bean bag are needed for the security of patient when steep table position changes (4). Secondly, a nasogastric or an orogastric tube is placed for decompressing the stomach and a urinary catheter is placed in patient’s bladder.
Operating room personnel used for this procedure are identical as for an open right hemicolectomy. The nurse and assistant stand on the patient’s right side initially, while the surgeon is on the other side facing patient’s right colon. After all the trocars are placed, the assistant moves to the left side of patient in order to direct the camera.
Step 1: incision
In HALS, the first port was placed via a cut-down procedure and an ENDOPATH DEXTRUSTM (Ethicon Endo-surgery Inc., Cincinnati, OH, USA) was placed through a 7 to 7.5 cm midline incision around the umbilicus (1).
With the minimal invasive incision, the whole small bowel can be exteriorized and the proximal inflammation can be checked up to 5 cm from the ligament of Treitz. The surgeon is allowed to measure the remaining length of small bowel as well. At this point, complete intestinal inspection is an indication for early conversion to an open surgery, if necessary (11). One of the greatest benefits of HALS is this immediate access to the peritoneal cavity via the minimal invasive incision (Figures 1,2,3). The surgeon can examine the peritoneal cavity before making decision on whether to proceed with a laparoscopy or change into laparotomy (9). The laparoscopic equipment is kept in the operating theater remained intact. If intraperitoneal condition is favorable, the hand-assist device could be placed through this incision and the HALS could be performed. Otherwise, laparotomy could be performed by simply extending the incision. The author has used this benefit to reduce the rate of conversion to laparotomy, which might generate the most expense and are associated with the poorest outcomes. In addition, it also reduces the risk of trocar-related complications (12).
Step 2: placing the hand-assist device
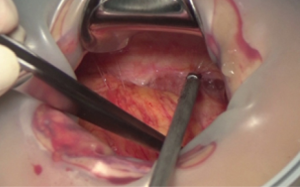
Once HALS is decided to be performed, the hand-assist device should be placed through the incision before the establishment of pneumoperitoneum. This allows evaluation and cut of abdominal adhesions (Figure 1), and facilitates the placement of the trocars under direct vision in order to avoid intra-abdominal injuries by trocar (13).
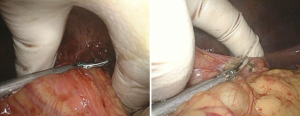
Via the basal port, small bowel and peripheral adhesion could be observed directly, even exteriorized (Figure 2). Adhesions beneath the incision could be directly released, which could save a lot of work under fully laparoscopy. Sometimes, great vessels like ileocolic artery could also ligate via the basal port.
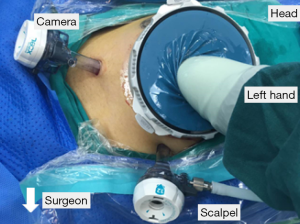
The trocar pattern described here is for right-sided colectomy under direct observation, and it can be changed according to the site of lesions and surgeon’s preference (Figure 3).
- The 12-mm camera port is localized 5 cm below the margin of basal port, slightly right or on the midline. This position of camera can clearly observe the surgical trunk of right colectomy, while avoiding interfering with the surgeon’s hand and the internal ring of the hand-assist device.
- The 12-mm trocar for surgeon is placed in the left upper quadrants at 5 cm above the umbilicus, or equal to the umbilicus. This position could allow the surgeon to easily reach the hepatocolic ligament.
Step 3: cecal mobilization
The patient should be right side inclined upward lying position, which makes the small bowel and omentum fall to the left upper quadrant, exposing the cecum (4). The small bowel is mobilized to left upper quadrant with the hand and endo Babcock clamp. By grasping the bowel wall near the base of the cecum by surgeon’s hand and pulling cephalic and to the left, the inflammatory adhesions around cecum would be divided using ultrasonic scalpel (Figure 4). The surgeon should change the direction and strength of retraction by hand and fingers to achieve better exposure and tissue resistance. After releasing the critical adhesions, appropriate plane beneath the base of the small-bowel mesentery and around the cecum can be seen. Carefully open the overlying peritoneum membrane, then the correct retroperitoneal plane will be totally exposed.
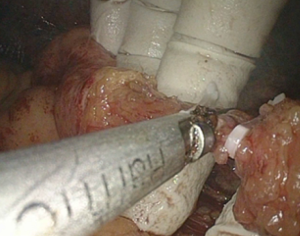
Moving cephalic and laterally, incising the white line of Toldt’s as much patience as possible, while the right colon is retracted medially and cephalically by surgeon’s hand. Ileocolic vessel can be hold in fingers, and ligated by clips (Figure 5). Properly broaden the plane to expose the duodenum from the covering mesentery.
The ureter is visualized as it courses over the right iliac vessels. It should be identified carefully before and after opening the peritoneum. The peristalsis could help to discriminate ureter form the gonadal vessels and the psoas tendon. If the ureter is suspected to be involved in the abscess or fistula by preoperative CT images, a temporary ureteral stent should be implanted before the abdominal procedure, and removed 1 or 2 days after surgery.
Step 4: hepatic flexure mobilization
Surgeon can now stand between the legs of patient, or still at the right side. In order to expose the attachments in the region of hepatic flexure, the patient is moved to reverse Trendelenburg with the right side lifted up, which makes the omentum and the colon move caudal (4).
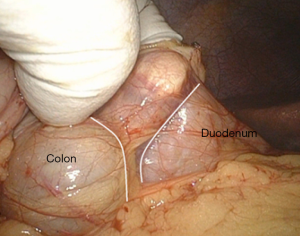
Carefully inserting the fingers into the plane between the peritoneum overlying the hepatic flexure and lateral-inferior wall of duodenum, to extend the plane between them (Figure 6). Incising medially until the gastrocolic ligament is divided. With the exposure by hand and fingers, plane between the gastrocolic ligament and the underlying transverse colon can be perfectly found (14).
Keeping the hepatic flexure elevated and held toward patient’s feet by hand-assist is very important. The surgeon need to make the anterior surface of the duodenum visual and intact so they can confirm that the hepatic flexure is mobilized toward the midline adequately.
After cutting the hepatocolic and gastrocolic ligament, the mesentery covering duodenum can also be detached under direct observation via the small incision around umbilicus. This could avoid injuries around the root of superior mesenteric vein. Once the duodenum and head of pancreas are fully exposed and the entire right colon is mobilized towards the midline, it is sufficient for exteriorization. Fully mobilization of the hepatic flexure to the midline makes extraction easier, which, if preferred, allows the surgeon to perform a wide stapled anastomosis.
Step 5: exteriorization, resection, and anastomosis
If mobilized properly, the colon from the terminal ileum to the mid transverse colon can be pulled out via the periumbilical incision. Adequate exteriorization of bowel and mesentery permits easier identification and ligation of the right colic or the right branch of the middle colic vessels than intracorporal vessel ligation.
Because of the variable anatomy of the right colon blood supply, it is necessary for the surgeon to identify the origins of the ileocolic, right colic, and right branch of the middle colic vessels relative to the superior mesenteric artery, before ligation is performed. Saving the right branch of the middle colic vessels can provide best blood supply to the anastomosis (4).
We also recommend side-to-side anastomosis between transverse colon and terminal ileum. The mesenteric defect is better to be closed (15,16).
Once the anastomosis is completed, the pneumoperitoneum is insufflated again for the inspection of anastomosis to ensure no volvulus of the two limbs in case of post-operative internal hernias. The abdomen and trocar sites are also checked for bleeding, and the fascia of the trocar sites is closed. Then the incision is closed after the pneumoperitoneum is deflated and the hand-access device is removed (17).
Human’s hand with five individual fingers is an exquisite instrument which give tactile feedback to the surgeon. Hand-assist procedure in difficult inflammatory cases should not be overstated. Occasionally, it may create problems with visualization for the novice during their early learning period, and may force the operator to creatively solve ergonomic problems (18,19).
Acknowledgments
Funding: This work was supported by National Natural Science Foundation of China (No. 81402019), 5010 Clinical Research Project of Sun Yat-Sen University (No. 2015007), and Science and Technology Planning Project of Guangdong Province (No. 2013B021800051).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bae SU, Park JS, Choi YJ, et al. The role of hand-assisted laparoscopic surgery in a right hemicolectomy for right-sided colon cancer. Ann Coloproctol 2014;30:11-7. [Crossref] [PubMed]
- Young-Fadok TM. Colon cancer: trials, results, techniques (LAP and HALS), future. J Surg Oncol 2007;96:651-9. [Crossref] [PubMed]
- Marcello PW, Fleshman JW, Milsom JW, et al. Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum 2008;51:818-26; discussion 826-8. [Crossref] [PubMed]
- Young-Fadok TM, Nelson H. Laparoscopic right colectomy: five-step procedure. Dis Colon Rectum 2000;43:267-71; discussion 271-3. [Crossref] [PubMed]
- Pyo DH, Huh JW, Park YA, et al. A comparison of hand-assisted laparoscopic surgery and conventional laparoscopic surgery in rectal cancer: a propensity score analysis. Surg Endosc 2016;30:2449-56. [Crossref] [PubMed]
- Yang I, Boushey RP, Marcello PW. Hand-assisted laparoscopic colorectal surgery. Tech Coloproctol 2013;17:S23-7. [Crossref] [PubMed]
- Hand-assisted laparoscopic surgery vs standard laparoscopic surgery for colorectal disease: a prospective randomized trial. HALS Study Group. Surg Endosc 2000;14:896-901. [Crossref] [PubMed]
- Iqbal M, Bhalerao S. Current status of hand-assisted laparoscopic colorectal surgery: a review. J Laparoendosc Adv Surg Tech A 2007;17:172-9. [Crossref] [PubMed]
- Meshikhes AW. Controversy of hand-assisted laparoscopic colorectal surgery. World J Gastroenterol 2010;16:5662-8. [Crossref] [PubMed]
- Cima RR, Pendlimari R, Holubar SD, et al. Utility and short-term outcomes of hand-assisted laparoscopic colorectal surgery: a single-institution experience in 1103 patients. Dis Colon Rectum 2011;54:1076-81. [Crossref] [PubMed]
- Fichera A, Peng SL, Elisseou NM, et al. Laparoscopy or conventional open surgery for patients with ileocolonic Crohn's disease? A prospective study. Surgery 2007;142:566-71; discussion 571.e1.
- O'Connell PR, Madoff RD, Solomon M. editors. Operative Surgery of the Colon, Rectum and Anus. Sixth Edition. FL: CRC Press, 2015.
- Loungnarath R, Fleshman JW. Hand-assisted laparoscopic colectomy techniques. Semin Laparosc Surg 2003;10:219-30. [PubMed]
- Lotti M, Capponi MG, Campanati L, et al. Laparoscopic right colectomy: Miles away or just around the corner? J Minim Access Surg 2016;12:41-6. [Crossref] [PubMed]
- Fazl Alizadeh R, Stamos MJ. Minimally invasive surgery for rectal cancer. Minerva Chir 2016;71:311-21. [PubMed]
- Keller DS, Ibarra S, Haas EM. Minimally invasive colorectal surgery: status and technical specifications. Minerva Chir 2015;70:373-80. [PubMed]
- Ballantyne GH, Leahy PF. Hand-assisted laparoscopic colectomy: evolution to a clinically useful technique. Dis Colon Rectum 2004;47:753-65. [Crossref] [PubMed]
- Takakura Y, Okajima M, Yoshimitsu M, et al. Hybrid hand-assisted colectomy for transverse colon cancer: a useful technique for non-expert laparoscopic surgeons. World J Surg 2009;33:2683-7. [Crossref] [PubMed]
- Meshikhes AW, El Tair M, Al Ghazal T. Hand-assisted laparoscopic colorectal surgery: initial experience of a single surgeon. Saudi J Gastroenterol 2011;17:16-9. [Crossref] [PubMed]
Cite this article as: Wu XJ, Ke J, Chen YF, Liu XH. Hand-assisted laparoscopic surgery in Crohn’s disease. Ann Laparosc Endosc Surg 2016;1:29.